Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 56(6); 2023 > Article
-
Original Article
An Important Strategy to Improve Adolescent Health Literacy: COVID-19 Modules in High School in Indonesia -
Nurina Hasanatuludhhiyah1
 , Visuddho Visuddho2
, Visuddho Visuddho2 , Abdul Khairul Rizki Purba1
, Abdul Khairul Rizki Purba1 , Annette d’ Arqom1
, Annette d’ Arqom1 , Ancah Caesarina Novi Marchianti3
, Ancah Caesarina Novi Marchianti3
-
Journal of Preventive Medicine and Public Health 2023;56(6):523-532.
DOI: https://doi.org/10.3961/jpmph.23.113
Published online: November 1, 2023
- 1,060 Views
- 95 Download
1Department of Anatomy, Histology, and Pharmacology, Faculty of Medicine Universitas Airlangga, Surabaya, Indonesia
2Medical Program, Faculty of Medicine Universitas Airlangga, Surabaya, Indonesia
3Public Health Division, Faculty of Medicine Universitas Jember, Jember, Indonesia
- Corresponding author: Nurina Hasanatuludhhiyah, Department of Anatomy, Histology, and Pharmacology, Faculty of Medicine Universitas Airlangga, Jl. Mayjen Prof. Dr. Moestopo No 47, Surabaya 60131, Indonesia E-mail: nurina-h@fk.unair.ac.id
Copyright © 2023 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
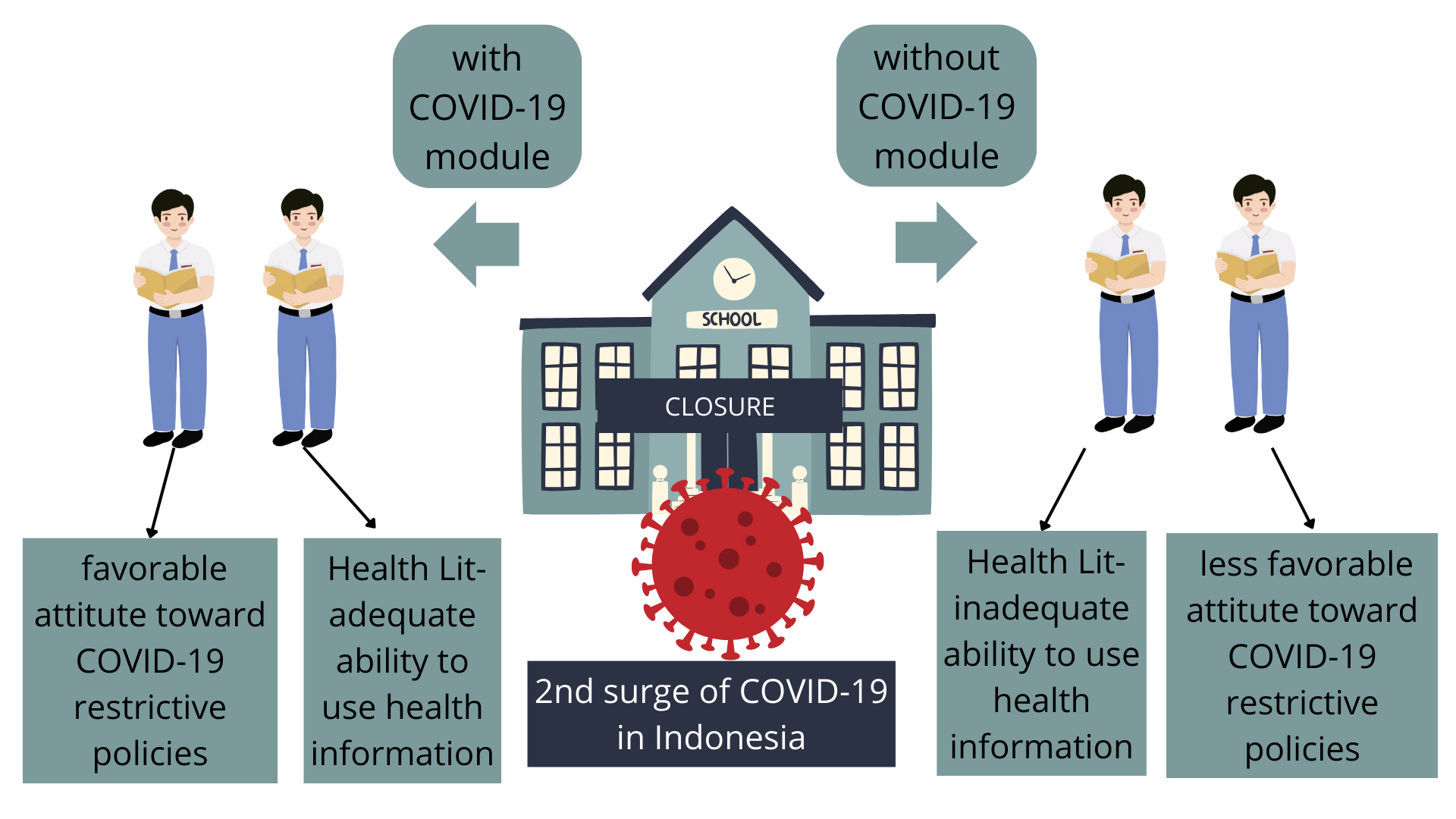
- During the second coronavirus disease 2019 (COVID-19) surge, cases increased sharply due to low awareness and compliance with measures to limit disease spread. Health literacy (HL) is an important component of public health initiatives, and schools are potential sources of health education to increase HL via the presentation of COVID-19 educational modules.
-
Methods
- This cross-sectional study involved an online questionnaire administered to students from 5 high schools in Surabaya and Sidoarjo, Indonesia, 6-7 weeks after the start of government-issued directives restricting public gatherings. We collected data on each respondent’s age, gender, parental education, and socioeconomic variables. HL was determined by the Health Literacy Measure for Adolescents. We additionally measured their attitudes and behaviors related to preventing the spread of COVID-19. The students were asked if they watched the COVID-19 module at school, their feelings about vaccination, and preferred online sources of COVID-19-related information.
-
Results
- Most of the 432 respondents had viewed COVID-19 modules at school. Module exposure was associated with significantly higher total and domain-specific HL and more positive attitudes toward government-issued COVID-19 restrictions on travel and public gatherings (p<0.05). However, behaviors to prevent COVID-19 spread and vaccine acceptance were not associated with module exposure. Most students chose social media as their source of COVID-19-related information.
-
Conclusions
- Schools can provide information to increase adolescents’ HL and the public’s support for health initiatives to prevent or limit the spread of COVID-19.
- In Indonesia, the second year of the COVID-19 pandemic (June to August 2021) saw rocketing cases and deaths that overwhelmed the nation’s healthcare system and exhausted its healthcare personnel [1]. The government responded by issuing policies to reduce COVID-19 spread by restricting public gatherings and promoting preventive behaviors to “flatten the curve” [2]. Simultaneously, the COVID-19 “infodemic” produced a metaphorical tsunami of information—much of it false or misleading—complicating efforts to disseminate accurate and evidence-based public health information. Misinformation can be dangerous and distort the public’s understanding of how to prevent or limit the spread of COVID-19 [3]. Additional hurdles included the public’s low education, disease awareness, and compliance with preventive behaviors [4]. Poor health literacy (HL) likely hampered COVID-19 control efforts [5].
- As defined by the European Health Literacy Consortium, HL comprises people’s knowledge, motivation, and competency to access, understand, appraise, and apply health information. This information informs day-to-day decisions concerning healthcare, disease prevention, and health promotion that likely affect the quality of life [6]. HL is associated with a reduced ability to understand, less awareness of health-related information [7], and less pandemic preparation [8], HL reflects an individual’s capability to understand and act on the information they receive. Individuals with high HL can determine which sources are trustworthy, potentially protecting against misinformation [9,10]. HL may similarly increase acceptance of (and compliance with) government-issued policies to prevent or limit the spread of COVID-19.
- Improving HL is important across the lifespan. Adolescents attending high school transition into adulthood and must prepare to participate as independent members of society. High schoolers demonstrate greater autonomy, decision-making capability, and responsibility for their health behaviors than children [11]. Consequently, their acceptance of government-issued policies and adherence to recommended disease-prevention measures deserve greater attention and should be foci of public health initiatives. One strategy for improving HL and attitudes toward the COVID-19 pandemic and adherence to preventive measures involves incorporating COVID-19 educational modules into high school curricula.
- Numerous studies have examined HL in various populations and established its association with health behaviors [12]; however, few studies have focused on adolescents [13]. More studies that examined HL in young adults and college students were completed during the early period of the COVID-19 pandemic. However, similar studies on high school students remain scarce. A 2020 Norwegian study, conducted during the early months of the COVID-19 pandemic, examined high school students’ HL and COVID-19 prevention behaviors and the potential associations of both variables [14,15]. To the best of the authors’ knowledge, no studies have attempted to examine how exposure to a COVID-19 educational module affects adolescents’ HL.
- This study measured adolescents’ HL, acceptance of government policies, adherence to COVID-19 prevention behaviors, COVID-19 vaccine acceptance, and potential associations of these factors with a COVID-19 educational module presented to high school students during the pandemic’s second surge. We also explored adolescents’ preferred online sources of COVID-19-related information.
INTRODUCTION
- Study Design and Data Collection
- This cross-sectional study recruited high school students living in Surabaya and Sidoarjo, Indonesia. The sample size was calculated (http://www.raosoft.com/samplesize.html) considering a 5% margin of error and 95% confidence interval; thus, the minimum sample size was 377.
- An online questionnaire was disseminated to the students through instructors at 5 high schools (selected for convenience) 6-7 weeks after government-issued restrictions were implemented to help slow the second COVID-19 surge. The questionnaire was developed and distributed following the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) principles, using an online survey platform https://app.surveyplanet.com/. The socio-demographic variables collected include age, gender, parental education, and socioeconomic levels. HL was measured by the Health Literacy Measure for Adolescents (HELMA), which comprised 44 items and 8 sections: access, reading, understanding, appraisal, use, communication, self-efficacy, and numeracy [16]. We modified an item within the numeracy section regarding the reference used for body mass index (BMI) classification. Asia-Pacific classification for BMI was employed in the item, rather than the World Health Organization (WHO) classification. The HELMA items were translated into Indonesian by 3 physician researchers proficient in both English and Indonesian and familiar with issues related to HL in adolescents.
- Attitudes were assessed by asking the students whether they agreed, were neutral, or disagreed with the government-issued policies that restricted travel and public gatherings. The preventive behavior score assessed respondents’ adherence to recommendations regarding mask-wearing, handwashing, physical distancing, crowd avoidance, and reducing mobility by determining (via self-report) how each respondent adhered to relevant health behavior recommendations. The items’ reliability and the validity of the questionnaire have been determined previously [17].
- The COVID-19 module was assigned by instructors of each school in an additional voluntary course during the COVID-19 pandemic. The module was constructed to contain information about COVID-19, especially about its prevention and how to get reliable information about COVID-19.
- Statistical Analysis
- We compared the groups’ binary baseline characteristics using the chi-square test. Numerical data were analyzed using the independent t-test (normally distributed) or the Mann-Whitney U test (not normally distributed). HELMA scores were calculated using the formula reported in the study that reported the tool’s development process and psychometric properties [16].
- Attitude scores were calculated by simply summing participants’ answers to 6 statements (disagree=1; neutral=2; agree=3; maximum score=18). Preventive behavior scores were calculated by simply summing participants’ answers to 5 questions (never =1; sometimes=2; usually=3; always=4; maximum score=20). Binary logistic regression models were used to evaluate the effect of socio-demographic characteristics. Binary logistic regression predicted the adjusted odds ratio (aORs) for an adequate HELMA score (>66.0); favorable attitude score (>12.0); favorable preventive behavior score (>15.0); and vaccine acceptance. A p<0.05 indicated a significant difference. SPSS version 17.0 (SPSS Corp., Chicago, IL, USA ) was used for all analyses.
- Ethics Statement
- This study was approved by the Ethics Committee, Faculty of Medicine, Universitas Airlangga (No. 136/EC/KEPK/FKUA/2021).
METHODS
- In total, 432 students were recruited from 5 senior high schools, as presented in Table 1. All completed the questionnaires, and 296 (69.0%) reported viewing the COVID-19 educational module at their respective schools. The median age was 17 years (interquartile range [IQR], 15-17). Most students were natural science majors (n=410, 94.9%). However, the proportion of students’ school majors did not differ between students who were and were not exposed to the COVID-19 module. At baseline, there were no significant between-group differences in parental education and socioeconomic status. Additionally, no significant between-group differences were observed in comorbidities and COVID-19 infection histories (Table 1).
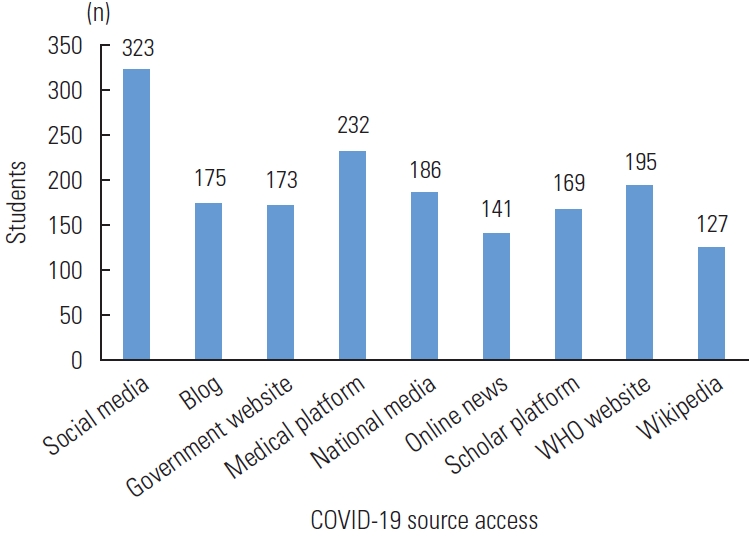
- The HL subscores for reading, use, and communication were considerably superior among students exposed to the COVID-19 module (p<0.05), as were HELMA scores (median, 64.2; IQR, 54.7-74.4) compared to those with no module exposure (median, 59.9; IQR, 51.1-72.2; Table 2). Most students reported using social media (n=323, 74.8%) to obtain COVID-19-related updates, including Instagram (n=296, 68.5%), Facebook (n=14, 3.2%), Twitter (n=92, 21.3%), YouTube (n=208, 48.1%), and TikTok (n=191, 44.2%). Other reported information sources were medical platforms (n=232, 53.7%), the WHO website (n=195, 45.1%), blogs (n=175, 40.5%), government websites (n=173, 40.0%), and scholarly platforms (n=169, 39.1%) (Figure 1). The HELMA results (Table 2) and the respondents’ preferred online sources of COVID-19-related information (Figure 1) are presented above.
- The impact of sufficient HL after completing the COVID-19 module was documented according to self-reported attitudes, adherence to recommended preventive behaviors, and vaccine acceptance. Students exposed to COVID-19 modules at their schools had better attitudes related to COVID-19 (12.4±2.6 vs. 11.7±3.0, p=0.026), including greater acceptance of government-issued COVID-19 policies such as school closures and restrictions on travel and public gatherings. Students exposed to the COVID-19 module demonstrated better adherence to preventive behaviors but lower vaccine acceptance; however, these differences did not rise to statistical significance (Table 3).
- We conducted an additional analysis to identify predictive factors for adequate levels of total HELMA and its 8 domains, favorable attitude and preventive behavior, and vaccine acceptance (Table 4). Exposure to COVID-19 modules tended to be associated with adequate levels of the HELMA, measured as a total score and subscores of all domains, but only the domain of use showed a statistically significant aOR value (aOR, 1.60, p<0.05). Several socio-demographic factors predicted adequate HELMA. Students’ major in natural sciences was associated with adequate levels for total HELMA and the domains of appraisal, communication, and numeracy, compared to social science majors (aORs, 3.08, 3.78, and 2.88, respectively; p<0.05). Age ≥17 years predicted adequate HELMA levels for the understanding, appraisal, and numeracy domains (aORs, 1.57, 1.68, and 1.86, respectively; p<0.05). Nevertheless, it was also associated with less vaccine acceptance than younger age (aOR, 0.24, p<0.05). Having a mother with a higher education degree also predicted adequate levels for the HELMA domains of reading, understanding, and use (aOR, 1.82, 1.83, and 1.69, respectively; p<0.05). On the contrary, high schoolers whose fathers had higher education degrees were less likely to have adequate HL in the use domain (aOR, 0.54, p<0.05). Surprisingly, men were less likely to have adequate HELMA levels in the self-efficacy and numeracy domains and adherence to preventive behavior than women (aORs, 0.65, 0.52, and 0.36, respectively; p<0.05). Low perceived economic status was also associated with a lower likelihood of having an adequate HL level in the communication domain (aOR, 0.34, p<0.05).
RESULTS
- We compared HL, attitudes toward COVID-19 control policies, adherence to COVID-19 preventive behaviors, and vaccine acceptance in high schoolers, some of whom were exposed to a COVID-19 educational module at their schools during the second COVID-19 surge. To our knowledge, this is the first cross-sectional study to investigate COVID-19-related factors using an online questionnaire and attempt to determine relationships between these factors and exposure to a COVID-19 educational module at school. A previous study found a correlation between HL levels and COVID-19 preventive behaviors [18] and improvements in students’ attitudes toward COVID-19 after exposure to an E-service-learning module [19]. Our results provide new evidence of the effectiveness of such modules for promoting public health initiatives, improving HL, and encouraging acceptance of government-issued policies aimed at preventing or limiting the spread of COVID-19.
- Most students in this study were exposed to the COVID-19 educational module at their high schools. These students demonstrated higher HL than those without module exposure for reading, use, and communication. These results agree with a Chinese study that showed a three-hour HL training intervention improved HL in adolescents compared to controls. Students who received HL training also had higher progress scores. This study concluded that the intervention effectively improved HL-related knowledge, attitudes, and skills. Importantly, the authors speculated that the application of student-focused and innovative teaching methods likely contributed to the substantial improvements in HL [20]. A quasi-experimental study from Indonesia found that HL improved from “inadequate” (60% of participants) to “excellent” (90% of participants) after exposure to a COVID-19 health education training intervention [21]. Thus, module-based training can increase HL. Such learning modules should be well-developed and delivered effectively. Dissemination of accurate public health information is particularly important for the COVID-19 pandemic (and resultant infodemic). Aside from their obvious applicability to future epidemics or pandemics, module-based educational applications could disseminate information about various health issues, including reproductive and mental health.
- Most students used social media—particularly Instagram— as their main source of COVID-19-related information. Other studies found similar results in adults [22]. Few studies have examined adolescents’ use of social media as a health information source. Esmaeilzadeh et al. [15] reported that the Internet and social media comprised the top 2 sources of health information related to high-risk behaviors in adolescents aged 15-18. Social media boosted misinformation during the COVID-19 pandemic and hindered the implementation of public health initiatives worldwide. For example, circulating conspiracy theories related to vaccine safety created undue anxiety and panic as the pandemic progressed [23,24].
- The use of social media as a stand-alone source of health information risks exposure to misinformation, particularly among those with low HL. Rosário et al. [25] found that university students who frequently used social media experienced more difficulty searching for information online and evaluating the validity and reliability of online information sources. However, these drawbacks should not negate the potential usefulness of social media for health education, including COVID-19 issues. Koenig et al. [26] found that Instagram had high acceptance among medical students and increased engagement in online teaching modules. A Chinese study used TikTok as a source for educational “micro-videos” that communicated health information to members of the younger generation [27]. Considering adolescents’ increasing use of social media, ensuring access and exposure to accurate health information is critically important [28].
- Government and public health agencies should look to social media as a potential source of valid and reliable health information presented in an understandable format [29]. Very few students used WHO or government websites as their primary source of online health information. A previous study discovered that university students who searched more frequently on public institution websites and health portals were more likely to be able to assess the reliability of health information than those who did not [25]. Thus, interventions should address specific competencies needed to acquire relevant and reliable health information. These learning modules could be incorporated into schools’ curricula to instruct students on these competencies, which become increasingly important over the lifespan. For example, COVID-19 modules could provide explicit education on identifying valid sources, applying scientific information to make everyday health decisions, and utilizing trustworthy sources such as official government websites to acquire COVID-19-related information. These factors are important for engaging adolescents in the public’s fight against this (and future) pandemic and infodemics [19].
- Adolescent students exposed to COVID-19 modules at their school had significantly higher attitude scores, meaning they agreed with government policies related to COVID-19 control, including restrictions on travel and public gatherings and school closures. However, the COVID-19 module was not associated with demonstrating actual preventive behaviors or with vaccine acceptance. Several studies showed a relationship between HL and attitudes and behaviors related to preventing COVID-19 [30,31]. A study of Jordanian adolescents found that most participants demonstrated basic COVID-19-related knowledge, a good attitude toward COVID-19 governmental policies, and good preventive behaviors. Similarly, a general population found that better COVID-19-related knowledge was associated with more consistent mask-wearing [32]. A study involving 1631 Taiwanese adolescents reported that good HL was correlated with good well-being during the COVID-19 pandemic [33]. Moreover, the results of our study are also in line with a survey in Norway (n=2205) that adolescents were more likely to have COVID-19 preventive behavior knowledge and practice, including social distancing. They were more likely to reduce their socialization with friends [14]. Thus, interventions that improve knowledge are crucial for adolescents. The COVID-19 educational module increased adolescents’ HL and attitudes. This approach has potential applicability to other health issues and could be delivered in an engaging and attractive format, such as forming online peer groups for high schoolers [34].
- Our study showed no significant difference between students with and without the COVID-19 module in certain domains of HL, including access, understanding, appraisal, self-efficacy, and numeracy, as well as preventive behavior and vaccine acceptance. We propose that our respondents living in urban areas had no difficulties accessing health information that was mostly disseminated through online platforms; therefore, COVID-19 module exposure would not have considerable influence on this domain [15]. Improving understanding, appraisal, self-efficacy, and numeracy would require a more intensive directive learning module. We believe that improving attitudes and behavior requires sufficient time and repeated interventions [35]. A brief exposure can lead to changes in attitudes, but not behavior [36]. In addition, during the COVID-19 period, preventive behavior or vaccination was not only a reflection of attitudes but also a form of compliance with social obligations and responsibility to the surrounding environment [37,38]. Students’ obedience to health protocols in Indonesia was impacted by a culture of adherence and responsibility to protect each other. Due to cultural norms, Asian students closely adhere to social obligations [39].
- We identified several socio-demographic factors that predicted adequate HL in certain domains. Age ≥17 years, which is perceived by most Indonesian people as an adult since those of this age are given elective rights, was associated with adequate levels of understanding, appraisal, and numeracy domains, despite lower vaccine acceptance. This could be related to their greater body of knowledge, as well as a greater sense of autonomy to take responsibility for the decision-making process, including in health-related matters, than those of younger age who often rely on their parents [11]. The mother having a higher education degree was a predictive factor for adequate levels of HELMA in the reading, understanding, and use domains. It was expected that the mothers would readily transfer their capabilities for processing the health information to their children [13]. It was not surprising that students majoring in natural sciences would predict adequate HL both for total HELMA and the HELMA domains of appraisal, communication, and numeracy since those students are exposed to more learning hours in human biology, which is closely related to health matters.
- Surprisingly our man respondents showed a lower likelihood for adequate HL levels in the self-efficacy and numeracy domains, as well as for adherence to preventive behavior. Our finding in young men is unique since many previous studies have reported that adult men were more likely than women to perceive COVID-19 as a less serious health problem and to be opposed to restrictive public policy measures. These tendencies partly account for higher COVID-19-related morbidity and mortality rates in men [40]. Lower HL in the self-efficacy domains could be related to less adherence to preventive behavior in this regard. Thus, any health initiative should be designed based on this gender difference and can be introduced earlier for man adolescents.
- There are some limitations to this study. Due to the second surge of COVID-19 in Indonesia, which mandated school closures, we used an online questionnaire platform. We could not use random sampling due to mobility restrictions and could only reach out to schools in urban areas. Future, well-powered studies on other, more representative samples are required.
- The COVID-19 pandemic and subsequent infodemic have complicated efforts to identify trustworthy and reliable online information sources, especially among adolescents. Therefore, an adequate level of HL is particularly important in helping them to collect and verify health information, and also improve their knowledge, attitude, and behavior toward COVID-19 control. Adolescents’ HL can be improved by incorporating a COVID-19 educational module into schools’ curricula. Schools should use similarly structured education programs, delivered innovatively and attractively, to improve HL over the lifespan. COVID-19 modules at school could also be used to promote other health initiatives and combat future pandemics and infodemics.
DISCUSSION
-
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
-
FUNDING
This project was supported by a research grant from the Faculty of Medicine, Universitas Airlangga in 2021 via RKAT, Contract No. 388/UN3/2021.
-
AUTHOR CONTRIBUTIONS
Conceptualization: Hasanatuludhhiyah N, Purba AKR, d’ Arqom A. Data curation: Hasanatuludhhiyah N, Visuddho V, Purba AKR, d’ Arqom A. Formal analysis: Hasanatuludhhiyah N, Visuddho V, Purba AKR. Funding acquisition: Hasanatuludhhiyah N. Methodology: Hasanatuludhhiyah N, Visuddho V, Purba AKR, d’ Arqom A. Project administration: Hasanatuludhhiyah N, Visuddho V, Purba AKR. Visualization: Hasanatuludhhiyah N, Visuddho V, Purba AKR, d’ Arqom A. Writing - original draft: Hasanatuludhhiyah N, Visuddho V, Purba AKR, d’ Arqom A. Writing - review & editing: Hasanatuludhhiyah N, Visuddho V, Purba AKR, d’ Arqom A, Marchianti ACN.
Notes
ACKNOWLEDGEMENTS
| Measurements |
COVID-19 module |
p-value | |
|---|---|---|---|
| With | Without | ||
| Attitude score, mean±SD1 | 12.4±2.6 | 11.7±3.0 | 0.026 |
| Preventive behavior score, mean±SD2 | 18.2±2.2 | 17.9±2.2 | 0.299 |
| Vaccine acceptance, proportion (%) | 278/296 (94.2) | 130/136 (95.6) | 0.562 |
- 1. World Health Organization Indonesia. Coronavirus disease 2019 (COVID-19) situation report – 65. 2021 Jul 28 [cited 2022 Jan 2]. Available from: https://cdn.who.int/media/docs/default-source/searo/indonesia/covid19/external-situation-report-65_28-july-2021-final.pdf?sfvrsn=a7697f51_5
- 2. Satuan Tugas Penanganan COVID-19. Indonesia fights back the covid-19 second wave. 2021 Jul 1 [cited 2022 Jan 2]. Available from: https://covid19.go.id/p/berita/indonesia-fights-backcovid-19-second-wave
- 3. Pan American Health Organization. Understanding the infodemic and misinformation in the fight against COVID-19. 2020 [cited 2022 Jan 2]. Available from: https://iris.paho.org/bitstream/handle/10665.2/52052/Factsheet-infodemic_eng.pdf
- 4. Satuan Tugas Penanganan COVID-19. Monitoring of adherence to health protocol in Indonesia. 2021 Apr 8 [cited 2022 Jan 2]. Available from: https://covid19.go.id/p/berita/monitoring-kepatuhan-protokol-kesehatan-tingkat-nasional-update-04-april-2021 (Indonesian)
- 5. Paakkari L, Okan O. COVID-19: health literacy is an underestimated problem. Lancet Public Health 2020;5(5):e249-e250ArticlePubMedPMC
- 6. Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health 2012;12: 80PubMedPMC
- 7. Liu C, Wang D, Liu C, Jiang J, Wang X, Chen H, et al. What is the meaning of health literacy? A systematic review and qualitative synthesis. Fam Med Community Health 2020;8(2):e000351ArticlePubMedPMC
- 8. Chima CC, Abdelaziz A, Asuzu C, Beech BM. Impact of health literacy on medication engagement among adults with diabetes in the United States: a systematic review. Diabetes Educ 2020;46(4):335-349ArticlePubMedPDF
- 9. World Health Organization. An ad hoc WHO technical consultation managing the COVID-19 infodemic: call for action. 2020 Sep 15 [cited 2022 Jan 2]. Available from: https://www.who.int/publications/i/item/9789240010314
- 10. Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int 2000;15(3):259-267Article
- 11. Halpern-Felsher B, Baker M, Stitzel S. Decision-making in adolescents and young adults. In: Diefenbach M, Miller-Halegoua S, Bowen D, editors. Handbook of health decision science. New York: Springer; 2016. p. 7-12
- 12. Visscher BB, Steunenberg B, Heijmans M, Hofstede JM, Devillé W, van der Heide I, et al. Evidence on the effectiveness of health literacy interventions in the EU: a systematic review. BMC Public Health 2018;18(1):1414ArticlePubMedPMCPDF
- 13. Sansom-Daly UM, Lin M, Robertson EG, Wakefield CE, McGill BC, Girgis A, et al. Health literacy in adolescents and young adults: an updated review. J Adolesc Young Adult Oncol 2016;5(2):106-118ArticlePubMed
- 14. Riiser K, Helseth S, Haraldstad K, Torbjørnsen A, Richardsen KR. Adolescents’ health literacy, health protective measures, and health-related quality of life during the Covid-19 pandemic. PLoS One 2020;15(8):e0238161ArticlePubMedPMC
- 15. Esmaeilzadeh S, Ashrafi-Rizi H, Shahrzadi L, Mostafavi F. A survey on adolescent health information seeking behavior related to high-risk behaviors in a selected educational district in Isfahan. PLoS One 2018;13(11):e0206647ArticlePubMedPMC
- 16. Ghanbari S, Ramezankhani A, Montazeri A, Mehrabi Y. Health literacy measure for adolescents (HELMA): development and psychometric properties. PLoS One 2016;11(2):e0149202ArticlePubMedPMC
- 17. Ihsan MN, Meliana A, Hasanatuludhhiyah N, Visuddho V, Purba AK, D’Arqom A. Attitude and behavior towards COVID-19 control among high school students in Surabaya and Sidoarjo. J Community Med Public Health Res 2023;4(1):25-32
- 18. Patil U, Kostareva U, Hadley M, Manganello JA, Okan O, Dadaczynski K, et al. Health literacy, digital health literacy, and COVID-19 pandemic attitudes and behaviors in U.S. college students: implications for interventions. Int J Environ Res Public Health 2021;18(6):3301ArticlePubMedPMC
- 19. Adkins-Jablonsky S, Fleming R, Esteban M, Bucio D, Morris JJ, Raut S. Impacts of a COVID-19 E-service-learning module in a non-major biology course. J Microbiol Biol Educ 2021;22(1):22.1.56ArticlePubMedPMCPDF
- 20. Yang HF, Chang CC, Tseng PL, Lai HR, Tasi JS, Huang WH, et al. Effectiveness of innovative instructional module for professional competence in health literacy in medical students. BMC Med Educ 2022;22(1):210ArticlePubMedPMCPDF
- 21. Falah F, Mobiliu S, Irbar I. The improvement of health literacy related to COVID-19 through education on health cadre of Dungigi primary health center Gorontalo. Sci J Health Pencerah 2021;10(1):9-13. (Indonesian)
- 22. Frey E, Bonfiglioli C, Brunner M, Frawley J. Parents’ use of social media as a health information source for their children: a scoping review. Acad Pediatr 2022;22(4):526-539ArticlePubMed
- 23. Germani F, Biller-Andorno N. The anti-vaccination infodemic on social media: a behavioral analysis. PLoS One 2021;16(3):e0247642ArticlePubMedPMC
- 24. Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One 2020;15(4):e0231924ArticlePubMedPMC
- 25. Rosário R, Martins MR, Augusto C, Silva MJ, Martins S, Duarte A, et al. Associations between COVID-19-related digital health literacy and online information-seeking behavior among Portuguese university students. Int J Environ Res Public Health 2020;17(23):8987ArticlePubMedPMC
- 26. Koenig JF, Buentzel J, Jung W, Truemper L, Wurm-Kuczera RI. Using Instagram to enhance a hematology and oncology teaching module during the COVID-19 pandemic: cross-sectional study. JMIR Med Educ 2021;7(4):e30607ArticlePubMedPMC
- 27. Zhu C, Xu X, Zhang W, Chen J, Evans R. How health communication via Tik Tok makes a difference: a content analysis of Tik Tok accounts run by Chinese provincial health committees. Int J Environ Res Public Health 2019;17(1):192ArticlePubMedPMC
- 28. Plaisime M, Robertson-James C, Mejia L, Núñez A, Wolf J, Reels S, et al. Social media and teens: a needs assessment exploring the potential role of social media in promoting health. Soc Media Soc 2020;6(1):2056305119886025ArticlePDF
- 29. Heiss R, Waser M, Falkenbach M, Eberl JM. How have governments and public health agencies responded to misinformation during the COVID-19 pandemic in Europe? 2021 [cited 2022 Jan 2]. Available from: https://eurohealthobservatory.who.int/monitors/hsrm/analyses/hsrm/how-have-governments-and-public-health-agencies-responded-to-misinformation-during-the-covid-19-pandemic-in-europe
- 30. Situmorang AG, Farahannisa KA, Rahmawati I, Rossyanti L. Education webinar increases the knowledge of the mask waste management during COVID-19 pandemic. J Community Med Public Health Res 2022;3(1):48-56
- 31. Patwary MM, Disha AS, Bardhan M, Haque MZ, Kabir MP, Billah SM, et al. Knowledge, attitudes, and practices toward coronavirus and associated anxiety symptoms among university students: a cross-sectional study during the early stages of the COVID-19 pandemic in Bangladesh. Front Psychiatry 2022;13: 856202ArticlePubMedPMC
- 32. Naser AY, Dahmash EZ, Alsairafi ZK, Alwafi H, Alyami H, Jalal Z, et al. Knowledge and practices during the COVID-19 outbreak in the Middle East: a cross-sectional study. Int J Environ Res Public Health 2021;18(9):4699ArticlePubMedPMC
- 33. Chen H, Zhang M, Su L, Cao H, Zhou X, Gu Z, et al. Knowledge, attitudes, and practices toward COVID-19 among Chinese teachers, Shenzhen: an online cross-sectional study during the global outbreak of COVID-19. Front Public Health 2021;9: 706830ArticlePubMedPMC
- 34. d’Arqom A, Indiastuti DN, Nasution Z. Online peer-group activism for thalassemia health education during the COVID-19 pandemic: a case study from East Java, Indonesia. J Health Res 2021;36(1):158-165Article
- 35. Kelly MP, Barker M. Why is changing health-related behaviour so difficult? Public Health 2016;136: 109-116ArticlePubMedPMC
- 36. Kian L, Zarifsanaiey N, Karimian Z. Effect of the e-flipped learning approach on the knowledge, attitudes, and perceived behaviour of medical educators. BMC Res Notes 2022;15(1):227ArticlePubMedPMCPDF
- 37. Patzina A, Dietrich H. The social gradient in COVID-19 vaccination intentions and the role of solidarity beliefs among adolescents. SSM Popul Health 2022;17: 101054ArticlePubMedPMC
- 38. Alfaray RI, Yodianto L, Dewayani A, Fauzia KA, Armyta DN, Rezkitha YA, et al. Correlation between knowledge of city of residence and COVID 19 on youth generations in Surabaya. J Public Serv 2021;5(1):116-122
- 39. Ho MJ, Lin CW, Chiu YT, Lingard L, Ginsburg S. A cross-cultural study of students’ approaches to professional dilemmas: sticks or ripples. Med Educ 2012;46(3):245-256ArticlePubMed
- 40. Galasso V, Pons V, Profeta P, Becher M, Brouard S, Foucault M. Gender differences in COVID-19 attitudes and behavior: panel evidence from eight countries. Proc Natl Acad Sci U S A 2020;117(44):27285-27291ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations

 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite



