Non-vaccination Against COVID-19 Among Venezuelan Refugees and Migrants Adults in Peru: A Cross-sectional Study, 2022
Article information
Abstract
Objectives
The purpose of this study was to determine factors associated with non-vaccination against coronavirus disease 2019 (COVID-19) among the Venezuelan immigrant population residing in Peru.
Methods
A cross-sectional study was conducted using data obtained from the Second Survey of the Venezuelan Population Residing in Peru in 2022. The dependent variable was vaccination status against COVID-19. The independent variables included socio-demographic, economic, and migratory characteristics of the included population. Crude and adjusted generalized linear Poisson-family models were used to calculate prevalence ratios with 95% confidence intervals (CIs).
Results
A total of 7739 Venezuelan migrants aged 18 years or older were included. The proportion of non-vaccination against COVID-19 was 5.7%. Regarding associated factors, unemployment (adjusted prevalence ratio [aPR], 1.31; 95% CI, 1.04 to 1.65) was linked to an increased likelihood of not being vaccinated against COVID-19. In contrast, women (aPR, 0.76; 95% CI, 0.61 to 0.95), possessing a migration permit (aPR, 0.41; 95% CI, 0.31 to 0.54), and having health insurance (aPR, 0.47; 95% CI, 0.27 to 0.81) were associated with a decreased likelihood of being unvaccinated.
Conclusions
The primary governmental and non-governmental institutions responsible for supporting and protecting the Venezuelan migrant and refugee population should improve vaccination access by issuing migration permits and providing health insurance.
INTRODUCTION
Vaccination against coronavirus disease 2019 (COVID-19) is an effective and safe strategy that has prevented over 19 million deaths worldwide [1]. In July 2022, the World Health Organization updated its global strategy for COVID-19 vaccination, aiming to achieve a 70% coverage rate in all countries to reduce the morbidity and mortality from this disease [1]. Since this revision, it is estimated that more than 5 billion people have received at least 1 vaccine dose, with the Americas region having one of the highest vaccination rates worldwide (204.08 total vaccine doses per 100 inhabitants) [2]. Although vaccination should be an equitable strategy across populations, vulnerable groups such as refugees or immigrants often lack adequate vaccination coverage due to barriers to access and certain characteristics of health systems [3,4]. In response to this, the World Health Organization SAGE Working Group on COVID-19 Vaccines recommended prioritizing vaccinations for migrant populations, given their greater vulnerability, risk, and needs [5].
Latin America and the Caribbean (LAC) is one of the regions that has hosted the largest populations of Venezuelan migrants worldwide, with close to 6 million Venezuelans relocating there in 2020 [6]. The emigration of Venezuelans began in 2010 due to political shifts that resulted in unfavorable living conditions, including inadequate access to food, healthcare, and education [7,8]. However, the greatest surge in Venezuelan migration has occurred from 2016 onwards, with exponential increases over the past 5 years [7,8]. Within LAC, Peru is the second-largest host of Venezuelan emigrants, accommodating over 1 million people by 2022 [9]. This influx of Venezuelans has posed an economic challenge for the Peruvian government, leading to difficulties for Venezuelans in accessing basic necessities, securing proper immigration status, combating food insecurity, and utilizing health systems and vaccination programs [10]. These challenges were exacerbated during the pandemic, making the Venezuelan population in Peru a high-risk group for contracting COVID-19 due to overcrowded living conditions and low-income jobs that hindered social distancing [11]. In Peru, the vaccination program conducted by the Ministry of Health has successfully administered at least 1 dose to over 26 million people [12]. However, as of October 2021, it was reported that only approximately 12% of the Venezuelan refugee and immigrant population had been vaccinated against COVID-19 [6]. In response, local Peruvian governments and non-governmental organizations have implemented promotional strategies to improve vaccination coverage among the Venezuelan population [11].
Previous research conducted among refugee or immigrant populations in Australia and Canada has identified several factors associated with vaccination against COVID-19 [13,14]. These factors include the age of the immigrant (with lower vaccination coverage observed in individuals over 50 years old), irregular migration status, and the length of time since migration (with lower coverage noted in those who migrated prior to the pandemic). Living in a rural area is also associated with a reduced likelihood of COVID-19 vaccination among migrants and refugees [13,14]. In addition to these factors, discriminatory behaviors, such as xenophobia, experienced by immigrants and refugees further hinder their access to equitable and adequate vaccination programs in their host countries [15]. However, most epidemiological studies conducted in LAC have focused on the prevalence and factors associated with vaccination intent in the general population [16,17], rather than considering Venezuelan immigrants, who are among the most vulnerable groups due to the impact of COVID-19 in this region.
Peru is one of the countries that have experienced unprecedented economic and health impacts due to COVID-19 [18,19]. These effects, coupled with the high concentration of Venezuelan immigrants, have led to a collapse of the health system and COVID-19 vaccination coverage [20]. Although the Peruvian population has reached more than 70% vaccination coverage [12], the current status of vaccination efforts among the Venezuelan immigrant and refugee population remains unclear. Consequently, the aim of the present study was to determine the factors associated with non-vaccination against COVID-19 among the Venezuelan immigrant population residing in Peru.
METHODS
Design and Data Source
An analytical cross-sectional study of the second Survey of the Venezuelan Population Residing in Peru (ENPOVE 2022) was carried out. ENPOVE 2022 was conducted by the National Institute of Statistics and Informatics (INEI), in February 2022 and March 2022 [21]. The primary aim of ENPOVE 2022 was to gather information on the demographic, social, economic, vulnerability-related, and protection needs of the Venezuelan refugee and migrant population in Peru, particularly in the context of the COVID-19 pandemic [20]. The design of ENPOVE 2022 allowed for representative estimates at the following levels of inference: (1) the total number of cities surveyed, (2) the metropolitan area of Lima and Callao, and (3) the remaining cities in the country [21].
The target population consisted of Venezuelan men, women, children, and adolescents who are refugees, asylum seekers, migrants, or individuals in need of protection. These individuals typically reside in private or communal housing in urban areas of the cities of Tumbes, Piura, Chiclayo, Trujillo, Chimbote, Ica, Arequipa, Lima, and Callao [22]. The information was collected for each household member aged 12 years or older. For those under 12 years of age, the information was provided by the head of household or a qualified informant. Trained interviewers used direct interview methods to collect data via a tablet. The research units included: (1) residences with a Venezuelan population, (2) households within these residences with a Venezuelan population, and (3) Venezuelan individuals living in the residences within the study area [22]. The ENPOVE 2022 defined a household as a group of people, related or not, who share main meals and attend to their essential needs collectively. It also recognized households consisting of a single individual [22].
For sample selection, ENPOVE 2022 utilized a sampling frame that incorporated basic information and cartographic material from the Cartographic Update and Registration of Dwellings and Establishments of the National Labor Market Survey. It also included information provided by the Peruvian National Superintendence of Migration [21,22]. This process resulted in a sample frame comprising 236 074 households with Venezuelan populations in Peru. From this, a total of 195 710 households were selected for the implementation of ENPOVE 2022, which represents 82.9% of the total number of households with Venezuelan members at the national level [22]. The sample selection process was probabilistic, stratified, and independent within each study city, yielding a total sample size of 3680 dwellings with Venezuelan residents. More detailed information regarding the sample design, procedures, and data collection can be found in the ENPOVE 2022 data sheet and report [21,22].
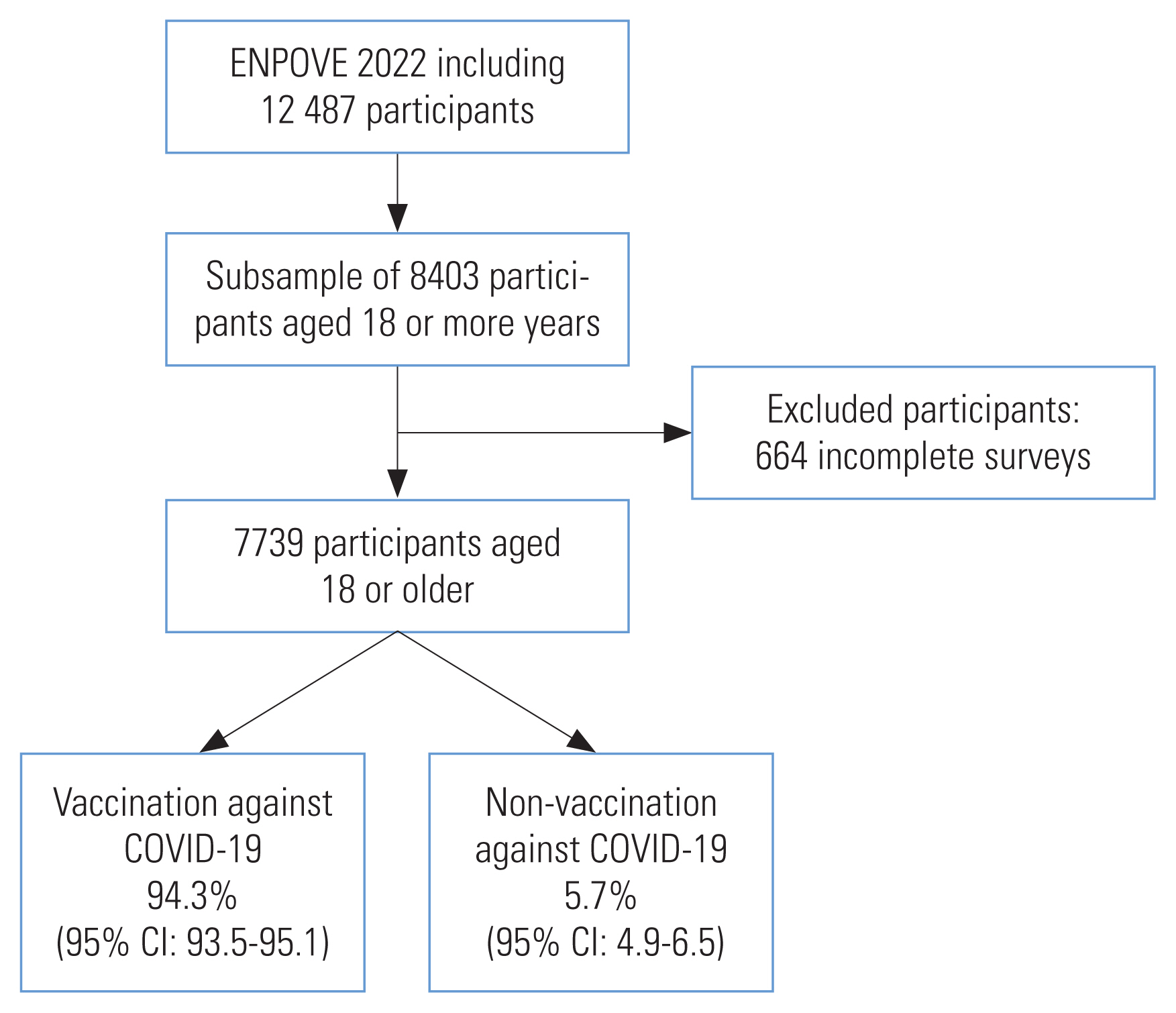
The ENPOVE 2022 database included a total of 12 487 participants. The sample selected for this study adults aged 18 years or older for whom complete data were available for the variables under study. Ultimately, the present study included a total of 7739 participants (Figure 1).
Variables Studied
The dependent variable was the vaccination status of migrants against COVID-19. This variable was dichotomized from the binary response to the question “Have you been vaccinated against COVID-19?” A positive response was categorized as “yes,” while a negative response was marked as “no”.
After reviewing the literature and considering the potential relationship with vaccination in the migrant population [23,24], the following independent variables were selected: gender (men, women), age group (18–59 or 60 years or older), education level (primary education or less, secondary education, or higher education), possession of a migration permit (yes or no), worked in the last week (yes or no), health insurance status (insured or uninsured), period of arrival in Peru (pre-pandemic [through 2019] or during the COVID-19 pandemic [2020 onwards]), experience of discrimination (yes or no), history or current COVID-19 (yes or no), presence of physical or psychological limitation (yes or no), and presence of any chronic disease (yes or no).
Statistical Analysis
Stata version 17.0 (StataCorp., College Station, TX, USA) was used for the statistical analysis, considering the complex sampling of ENPOVE 2022. Additionally, a subpopulation analysis was conducted using the subpop command (respondents aged 18 years or older) for all estimates.
A descriptive analysis of population characteristics was performed using absolute frequencies and weighted proportions. Each independent variable was compared with the weighted proportion, along with its 95% confidence interval (CI), of vaccinated and unvaccinated individuals. This comparison was performed using the chi-square test with a Rao-Scott correction. To evaluate the factors associated with non-vaccination, crude and adjusted analyses were performed using generalized linear models of the Poisson family with a log link. This yielded crude prevalence ratios (PRs) and adjusted prevalence ratios (aPRs) with 95% CIs. Variables were chosen for the adjusted model if they had a p-value of less than 0.20 in the crude model. The variance inflation factor was used to determine the presence of collinearity, and none of the values exceeded 10. A 2-tailed p-value of less than 0.05 was considered to indicate statistical significance.
Ethics Statement
During the implementation of ENPOVE 2022, informed consent was obtained from all respondents. All analyzed data were anonymized and contained no information that could lead to the identification of any respondent. The anonymized databases, along with other relevant ENPOVE 2022 documents, are available online and can be freely downloaded from the INEI microdata repository ( https://iinei.inei.gob.pe/microdatos/).
RESULTS
A total of 7739 Venezuelan migrants aged 18 years or older, who were surveyed in the ENPOVE 2022 and for whom complete data were available, were included (Figure 1). Most of these individuals were women (n=3999, 51.6%) and between 18 years old and 59 years old (n=7440, 96.3%). Our findings revealed that 29.7% did not possess an immigration permit, 23.6% did not work in the week prior to the survey, and 32.8% had previously contracted or currently had COVID-19. Additional details regarding the population characteristics can be found in Table 1.
In 2022, the proportion of non-vaccination against COVID-19 reported between February 2020 and March 2020 was 5.7% (95% CI, 4.9 to 6.5). The highest proportions of non-vaccination were found among individuals without a migration permit (10.5%), those with an education level of primary school or less (8.3%), and those who had migrated to Peru during the pandemic period (7.1%). Similarly, individuals without employment (7.1%), health insurance (6.7%), or a positive COVID-19 diagnosis (6.5%) reported higher proportions of non-vaccination (Table 2). Among the population that had been vaccinated against COVID-19 (94.3%), the proportions of individuals who had received 1, 2, and 3 doses were 8.4%, 61.9%, and 29.8%, respectively. The majority of men received the second dose (62.3%), whereas a higher proportion of women received all 3 doses of COVID-19 (32.2%). Regarding age, the largest proportion of individuals aged 18 years to 59 years received the second dose of the vaccine (63.2%), whereas a highest proportion of older adults (60 years and older) received 3 doses (68.1%). Further details regarding the distribution of the population based on the number of doses received are shown in Table 3.
Regarding the factors associated with non-vaccination among Venezuelan nationals, the crude analysis revealed that most determinants had a statistically significant association with the dependent variable. Exceptions included gender, age group, discrimination, physical and psychological limitation, and chronic disease. When adjusting the analysis for variables with a p-value less than 0.20 in the crude analysis, it was found that unemployment (aPR, 1.31; 95% CI, 1.04 to 1.65) was associated with an increased likelihood of not being vaccinated against COVID-19. In contrast, women (aPR, 0.76; 95% CI, 0.61 to 0.95), possessing a migration permit (aPR, 0.41; 95% CI, 0.31 to 0.54), and having health insurance (aPR, 0.47; 95% CI, 0.27 to 0.81) were linked to a decreased likelihood of non-vaccination (Table 4).
DISCUSSION
Based on our findings, the prevalence of non-vaccination against COVID-19 among Venezuelan migrants aged 18 years or older was 5.7%. The highest proportions of non-vaccination were observed among individuals with a lower education level, those who had arrived in Peru during the pandemic, and those who had not been diagnosed with COVID-19. Furthermore, the migrant population often lacked basic necessities such as a migration permit, employment, or health insurance. Notably, not having worked in the last week was associated with a higher likelihood of non-vaccination against COVID-19, while socio-demographic determinants such as gender, possession of a migration permit, and health insurance were associated with higher vaccination rates in this Venezuelan population.
Regarding non-vaccination, our data indicate that approximately 5 of every 100 Venezuelan individuals have not been vaccinated against COVID-19. This value is lower than those reported in studies of immigrants and refugees in Canada (21.8%) [14]; in refugees from Afghanistan, Sudan, and Myanmar in the United States (29.7%) [25]; and in immigrants of Mexican nationality in the United States (29.9%) [24]. In contrast, several studies conducted among migrants and refugees at a single health center in Turkey and a refugee camp in Jordan have reported non-vaccination rates exceeding 20%. However, these studies are not directly comparable to our findings due to the lack of representativeness of the study populations. Specifically, these studies were conducted among Palestinian refugees in a single refugee camp in Jordan, where the non-vaccination rate was 77.4% [23], and among pregnant Syrian refugee women at a single health center in Turkey, where the rate was 69.3% [26]. The discrepancy between the non-vaccination rates in our study and those conducted in Canada and the United States could be attributed to differences in sample size and the timing of the studies (conducted in 2020 and 2021). While such variations could produce different non-vaccination rates, the findings highlight a global health issue: the most vulnerable populations—such as refugees and immigrants—are not receiving COVID-19 vaccinations, despite being among the groups most susceptible to infection and transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Our findings indicate that some individuals of Venezuelan nationality still have not been vaccinated, which could be due to the main limitations faced by immigrants or refugees during the vaccination process [27]. These limitations are related to a lack of access to health services; immigration status; lack of transportation to vaccination centers; insufficient knowledge about the efficacy, safety, and effectiveness of vaccines; and discrimination [27].
Regarding factors associated with COVID-19 non-vaccination, findings indicate that unemployed Venezuelan nationals are relatively likely to remain unvaccinated, which aligns with studies conducted in the United States and Jordan [23,25]. In contrast, employed individuals often consider employer recommendations when deciding whether to get vaccinated [28]. Moreover, the fear of job loss due to severe illness increases the likelihood of vaccination among these individuals [29]. In Peru, the government has mandated full vaccination for workers to continue their employment, a strategy aimed at boosting vaccination rates in the country [30]. Venezuelan women were found to be less likely to be unvaccinated than men. The biomedical literature provides inconclusive evidence regarding gender-based differences among immigrants or refugees [31,32]. However, prior studies have indicated that women tend to perceive a higher risk from COVID-19, which could increase their likelihood of becoming vaccinated to mitigate the risk of severe illness and death from the disease [28,33]. Regarding immigration status and health insurance, several studies have identified the absence of health insurance and immigration permission as the prime barriers to accessing COVID-19 vaccination programs [34–36]. Immigrants without legal documentation often live in constant fear of immigration checks and potential deportation, even when government institutions open vaccination campaigns to immigrants, regardless of their legal status [32,37]. In Peru, the government has included undocumented Venezuelan immigrants in the national vaccination plan [38]. However, our findings suggest that a segment of the immigrant population has not been vaccinated against COVID-19 due to perceived rejection by healthcare personnel [15]. Given these factors, both governmental and non-governmental organizations should intensify their efforts to achieve full vaccination coverage among this vulnerable population and decrease mortality from COVID-19.
Our findings carry implications for public health. First, the Peruvian government should collaborate with non-governmental organizations, such as the United Nations Refugee Agency or VeneActiva. These institutions have a wider reach and more robust communication channels with this vulnerable demographic. Second, virtual or telephonic means of communication should be used to promote vaccination among the Venezuelan population, providing guidance on the benefits of vaccination compared to the outcomes of contracting COVID-19. Third, the government should intensify its efforts to increase the number of Venezuelans holding migration permits in Peru. This would enable these individuals to access health insurance. Finally, the consistent support of government institutions is crucial to ensure equitable access to COVID-19 vaccination.
The current study used a survey database that provided information on the socio-demographic, social, economic, and migratory characteristics of Venezuelan refugees and migrants in Peru during the COVID-19 pandemic. This provided a current overview of the vaccination status within this specific population. Notably, this is the first study to assess COVID-19 vaccination rates among the Venezuelan population living in Peru, and our findings could be instrumental in shaping health policies. However, the study does have limitations. For instance, it was not possible to establish causality among the study variables due to the lack of temporality in the measurement of these variables. Memory bias may also have impacted the data, as the events in question occurred at specific times, such as the individual’s arrival in Peru. Additionally, some variables of interest were not included as independent variables due to unavailability. These variables pertain to knowledge, beliefs (particularly anti-vaccine rumors), receipt of health communication about the vaccine, having a family member who has had COVID-19, socioeconomic status, and household characteristics (such as immigrants sharing the same nationality and culture, living conditions, or the presence of a cohabitant). In addition, the temporality of our results should be considered. The survey data were collected between February 2022 and March 2022, while the third vaccine dose became mandatory in Peru in April 2022. This means that our findings provide only a snapshot of the vaccination landscape at the start of 2022, before the introduction of the mandatory third dose [39]. Finally, the respondents may have been influenced by social desirability bias. Variables such as the presence of a psychological limitation or migration permit could lead to stigma or discrimination, potentially influencing the responses given.
In conclusion, our findings indicate that as of March 2022, 5% of Venezuelan nationals had not been vaccinated against COVID-19. In addition, determinants such as gender, possession of a migration permit, and health insurance appeared to facilitate COVID-19 vaccination among Venezuelans, while unemployment was related with non-vaccination. Governmental and non-governmental institutions should collaborate to devise strategies to improve vaccination access for Venezuelan immigrants and refugees. This could be achieved through the provision of migration permits and health insurance.
DATA AVAILABILITY
The databases are freely accessible and can be downloaded from the website of the Instituto Nacional de Estadística e Informática ( https://proyectos.inei.gob.pe/microdatos/).
Notes
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Both authors contributed equally to conceiving the study, analyzing the data, and writing this paper.
ACKNOWLEDGEMENTS
The authors thank the Universidad Científica del Sur for their support in the publication of this research. To Donna Pringle for reviewing the language and style.