Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 44(5); 2011 > Article
-
Original Article
The Effect of Eating Behavior on Being Overweight or Obese During Preadolescence - Hye Ah Lee1, Won Kyung Lee1, Kyoung-Ae Kong2, Namsoo Chang3, Eun-Hee Ha1, Young Sun Hong4, Hyesook Park1
-
Journal of Preventive Medicine and Public Health 2011;44(5):226-233.
DOI: https://doi.org/10.3961/jpmph.2011.44.5.226
Published online: September 28, 2010
1Department of Preventive Medicine, School of Medicine, Ewha Womans University, Seoul, Korea.
2Hospice & Palliative care Branch, National Cancer Control Institute, National Cancer Center, Goyang, Korea.
3Department of Nutritional Science and Food Management, College of Health Sciences, Ewha Womans University, Seoul, Korea.
4Department of Internal Medicine, School of Medicine, Ewha Womans University, Seoul, Korea.
- Corresponding author: Hyesook Park MD, PhD. 911-1 Mok 6-dong, Yangcheon-ku, Seoul 158-710, Korea. Tel: +82.2-2650-5756, Fax: +82.2-2653-1086, hpark@ewha.ac.kr
- *Clinical Trial Center, Ewha Womans University Medical Center
Copyright © 2011 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- Being overweight or obese is central to metabolic syndrome, and these characteristics constitute dominant risk factors for chronic diseases. Although behavioral factors, including eating habits and sedentary lifestyles, are considered to be determinants of obesity, the specific childhood factors that contribute to this condition have not been clearly defined.
-
Methods
- The subjects consisted of 261 children aged 7-9 years who were recruited from an elementary school during October 2003. Information was obtained from their parents using a questionnaire focused on eating behaviors and lifestyle factors, additional data were also collected via anthropometric measurements and biochemical examinations, including blood tests.
-
Results
- A total of 48 (18.4%) of the 261 children were overweight, and 34 (70.8%) had at least one other component of metabolic syndrome. Eating behaviors emerged as significant lifestyle-related risk factors for being overweight or obese. Those who engaged in overeating more than twice per week had three times the risk of being overweight (odds ratio [OR], 3.10, 95% confidence interval [CI], 1.39 to 6.92), and those who ate rapidly had three times the risk of being overweight (OR, 3.28; 95% CI, 1.68 to 6.41). Those who had fewer family meals (fewer than 2-3/month) had a nine times higher risk of being overweight than those who had family meals more frequently (at least 1/day) (OR, 9.51; 95% CI, 1.21 to 74.82).
-
Conclusions
- This study showed that being overweight or obese during preadolescence is associated with a higher risk of metabolic syndrome and is related to unhealthy eating behaviors. Thus, weight-control strategies and healthy eating behaviors should be developed early in life to reduce the risk for metabolic syndrome.
- Obesity has become a serious global public health problem. The International Obesity Task Force reported that approximately 155 million school-aged children are overweight or obese worldwide [1]. The overall prevalence of obesity in Korea has increased consistently, moving from 5.8% in 1997 to 9.7% in 2005 [2]. Being overweight or obese is central to developing metabolic syndrome, and these characteristics constitute the dominant risk factors for chronic illnesses such as cardiovascular disease and type 2 diabetes. Additionally, being overweight or obese during childhood has long-term adverse effects on health. Thus, national attention has been focused on preventing and reducing childhood obesity, particularly in preadolescents.
- Obesity is a complex problem resulting from a combination of genetic, behavioral, environmental, and socioeconomic issues [3], identification of the risk factors that are modifiable is central for obesity prevention and epidemiology. During the past few decades, behavioral changes such as the adoption of sedentary lifestyles and less healthy eating habits have contributed to obesity. Several studies have shown that a sedentary lifestyle that incorporates, for example, prolonged television viewing, physical inactivity, and unhealthy eating habits during childhood was associated with an elevated risk of developing obesity [4-6]. These findings have led to the hypothesis that the risks for obesity are not only genetic but are indeed amplified by an unhealthy lifestyle during childhood. Although behavioral factors, including eating behaviors and a sedentary lifestyle, are determinants of obesity, more specific behavioral contributors to obesity have not been clearly defined. Moreover, preventive strategies that focus on adolescents and young adults have been largely unsuccessful [4]. However, most studies have focused on adolescents or young adults, and studies of the clustering of metabolic components in preadolescent children have confirmed that the distribution of these components may provide useful information.
- Therefore, we identified the effects of specific lifestyle-related risk factors, such as eating behaviors, on being overweight or obese and on the distribution of the components of metabolic syndrome in overweight and obese preadolescents.
INTRODUCTION
- I. Study Subjects
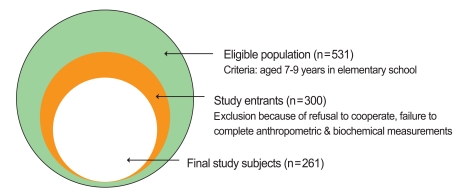
- The subjects consisted of 261 Korean children aged 7-9 years who were recruited from second and third grades at an elementary school in Seoul, Republic of Korea, during October 15 and 16 of 2003. The parents or guardians of the children provided consent for their child's participation in this study. Information, including lifestyle-related data, was obtained from the parents through an eating-behavior questionnaire, data were also collected by anthropometric measurements and biochemical blood examinations (Figure 1). More detailed methods of recruiting study subjects were provided in a previously published paper [7]. This study was approved by Institutional Review Board of Ewha Womans University Hospital.
- II. Data Collection
- Data on the lifestyles and eating behaviors data of children were gathered from parents or guardians; these data included number of days of moderate physical activity per week and time spent watching TV per day (<1 hour, 1-2 hours, >2 hours). This information was used to identify respondents with sedentary lifestyles. Frequencies of overeating, eating precooked/frozen food, and eating out were ascertained with a food-frequency questionnaire. Questions about eating rate (fast, medium, or slow) and family meals (1/day, 4-6/week, 1-3/week, and 2-3/month) were constructed on the basis of previous studies. These factors were recategorized based on a frequency test.
- Additional data on parental disease history, educational status, and current body mass index (BMI) were also obtained from the parents or guardians via questionnaire. If either parent had experienced a disease, it was included in the parental disease history.
- III. Measurements
- Medical examinations were conducted to collect information on anthropometric characteristics and to measure blood pressure and take blood samples. Height and waist circumference were measured to the nearest 0.1 cm, and weight was measured to the nearest 0.1 kg using a stadiometer and a calibrated scale with the child wearing only light clothing and no shoes. Blood pressure (BP) was measured on the right arm using a vital-signs monitor (Dinamap PRO 100; GE Healthcare, Little Chalfont, Buckinghamshire, UK) after the subject had been sitting comfortably for at least 5 minutes. Participants were instructed to fast for at least 8 hours prior to the examination in preparation for gathering data related to biochemical indices. Serum total cholesterol, high-density lipoprotein (HDL) cholesterol, triglycerides, and fasting glucose were measured with an automatic analyzer (model 7180; Hitachi, Tokyo, Japan).
- BMI was calculated as weight divided by height squared (kg/m2). Subjects were categorized as obese (≥95th percentile), overweight (85-94th percentile), or normal (<85th percentile) according to their current BMI using sex- and age-specific criteria from the 2007 Korean Children and Adolescents Growth Standards [8].
- We used the modified criteria developed by Cook et al. [9] to determine the clustering of risk factors for metabolic syndrome. Components of metabolic syndrome were judged to be present when at least one of the following risk factors was observed: waist circumference ≥90th percentile of subjects in this study adjusted for age and sex; systolic or diastolic BP ≥90th percentile of Korean children adjusted for age, sex, and height; fasting glucose ≥110 mg/dL, triglycerides ≥110mg/dL, and HDL cholesterol ≤40 mg/dL.
- IV. Statistical Analysis
- We compared the basic characteristics of normal, overweight, and obese participants using analysis of variance (ANOVA) and chi-square or Fisher's exact tests with trend analysis. The distribution of risk factors for metabolic syndrome was analyzed using a chi-square test. Bivariate and multivariate logistic regression analyses were conducted to evaluate the association between various factors and being overweight and obese. Factors with a significance of < 0.1 according to the bivariate logistic regression analysis were selected for a multivariate model. The multivariate logistic regression estimated the effect of lifestyle on being overweight and obese after adjusting for sex, age, education of the mother, maternal BMI, and parental diabetes. All analyses were conducted using SAS version 9.1 (SAS Inc., Cary, NC, USA). A p-value <0.05 was considered statistically significant.
METHODS
- The 261 subjects were aged 8.21 ± 0.70 years (mean ± standard deviation [SD]) and included 136 boys (52.1%). The proportions of subjects who were overweight and obese were 11% (n = 29) and 7% (n = 19), respectively. Maternal BMI was significantly higher in obese children compared with that in mothers of normal-weight children (24.7 kg/m2 vs. 23.4 kg/m2). The obese group included a significantly higher proportion of children of parents with diabetes mellitus (p < 0.05) (Table 1).
- High BP (90th percentile) was most the prevalent (28.0%) component of metabolic syndrome, whereas fasting glucose ≥110 mg/dL was the least common (0.8%). The overall prevalence of risk factors for metabolic syndrome was higher in the obese group than in the other groups. More than half of the overweight and almost all of the obese children had at least one risk factor for metabolic syndrome. Approximately 2% of all children and 21.1% of obese children had three or more risk factors, meeting the diagnostic criteria for metabolic syndrome (Table 2).
- When we compared lifestyle factors among BMI categories, overweight and obese participants were combined into an overweight group because the number of obese subjects was small. Time spent watching TV tended to be higher in the overweight group than in the normal-weight group, and this difference reached marginal significance (p = 0.07). About half of the obese children spent ≥2 hours per day watching TV, whereas about 25% of the others spent that much time watching TV. The rate at which children ate differed significantly different between normal-weight and overweight groups. More children in the overweight than in the normal-weight group were reported by their parents to eat rapidly (41.7% vs. 15.1%). Children in the overweight group were also significantly more likely to overeat (60.9% vs. 27.5%) and significantly less likely to eat family meals (10.4% vs. 2.4%) compared with the normal group. However, the groups did not differ with respect to physical activity (Table 3).
- Table 4 presents the associations between lifestyle-related factors and overweight or obesity. According to a bivariate analysis, those who spent >2 hours per day watching TV had an approximately two-fold greater risk of being overweight (odds ratio [OR], 2.19; 95% confidence interval [CI], 1.04 to 4.59). Those who ate fewer than three meals per month with their families had 4.18 (95% CI, 1.13 to 15.43) times the risk of being overweight than those who ate one meal with their families per day. Eating rate, overeating, and number of meals eaten with family remained significantly associated with being overweight in the multivariate logistic regressions analysis.
RESULTS
- We found that eating behaviors such as eating rapidly, overeating, and participating in family meals only infrequently were significantly associated with preadolescents' risk for being overweight. Despite their young age, almost all obese children had at least one risk factor for metabolic syndrome, and one-quarter of obese children met the criteria for a diagnosis of metabolic syndrome.
- The etiology of obesity is multidimensional. The dramatic increase in obesity during the past several decades suggests that environmental factors predominate over genetic effects [6]. Given that the incidence of obesity decreases with age, some studies have reported that becoming overweight at an early age has a more severe effect in adulthood than later overweight status has [10]. In the present study, children who were overweight or obese were at a greater risk for developing the risk factors for metabolic syndrome, a finding that was consistent with the results of previous studies [9]. Thus, this result provides additional evidence for the relationship between obesity and metabolic dysfunction. It also shows that additional studies are needed to identify the risk factors that can be modified to prevent childhood obesity. Potentially modifiable risk factors for obesity involve physical activity, watching TV, and an unhealthy diet. However, several interventional studies on increased physical activity and diet control have not provided consistent results or succeeded in modifying adult behavior. Because lifestyles and behaviors are established early in life, strategies to eliminate and/or modify the risk factors for obesity should be implemented during preadolescence [11].
- Obesity results from an imbalance between energy intake and energy expenditure. Epidemiological studies have shown that physical inactivity and a sedentary lifestyle are independently related to the development of obesity in children [12], adolescents [13], and adults [14]. Decreased opportunities for physical activity may contribute to obesity. Indeed, watching TV results in a lower metabolic rate than do other sedentary activities such as reading, writing, and playing board games [15]. One study showed that watching TV for long periods was associated with lower levels of HDL cholesterol and higher levels of leptin [3]. According to the Nurses' Health Study, watching TV for >2 hours per day was associated with a 23% increase in obesity in adult women [14]. One cohort study reported that >8 hours of TV watching per week at 3 years of age increased the risk for obesity at age 7 by 1.6 times [4]. In the present study, those who spent >2 hours per day watching TV had twice the risk of being overweight (95% CI, 1.04 to 4.59), but this effect disappeared after adjusting for other factors. Furthermore, unlike previous studies [5], we could not identify the risk posed by physical inactivity for being overweight. One longitudinal study showed that physical inactivity appeared to be the result of obesity rather than its cause. The authors stated that promoting physical activity has been largely unsuccessful [16]. Research on the etiology of obesity has been hampered by an inability to accurately assess such characteristics of physical activity as intensity, patterns, and quantity. Thus, the relationship between inactivity and obesity may reflect other, unknown factors and not indicate direct causality. Recently, an article reviewing studies that attempted to modify physical activity reported that physical interventions to deal with childhood obesity are unlikely to have a significant effect in improving BMI, although such interventions do have other beneficial health effects [17].
- Constant commercial advertisements accompanied by prolonged TV watching may lead to unhealthy eating patterns such as snacking, which typically involves a higher caloric intake than do more healthy eating habits [18-20]. This change to an unhealthy diet including low fiber intake, a lack of fruits and vegetables, increased sugar, and more convenience food is also widely believed to have contributed to the child obesity epidemic [21]. Moreover, eating behaviors and energy intake are also related to the development of obesity. Although one review article stated that unhealthy eating habits such as eating outside of the home, participating in few family meals, eating rapidly, and overeating may affect total caloric intake [6], only a few studies on eating behaviors and child obesity have been conducted. Consistent with previous findings, the present study revealed an association between being overweight and eating rapidly [11,22]. One study showed that those who have eaten rapidly from a young age also weighed more, had higher BMIs, and consumed more energy [23]. Several randomized controlled trial studies have also found that eating more slowly and reducing total food intake were useful for obese adolescents [24]. Because an abnormally rapid rate of eating may lead to additional eating before the stomach senses fullness, the rate of eating and the quantity of energy consumed may be positively related [23]. In the present study, eating rate appears to have been associated with overeating, as almost 60% of children who ate rapidly also engaged in overeating (data not shown).
- Unfavorable family circumstances have also been associated with overweight among children [25]. The frequency with which families eat together has decreased as the consumption of fast food and unhealthy meals have increased [6]. Mealtimes spent with parents contribute to the nutritional beliefs and attitudes held by children [26]. Several studies have reported that children who attended fewer family meals were more likely to be overweight [27,28]. Parents influence what, when, and how much children eat and can also directly guide their children's eating behaviors [26]. However, further research is needed to clarify the mechanisms by which family meals affect children's long-term health.
- This study had several limitations. First, we used self-reports to gather data on factors related to lifestyle, which may have influenced the validity of the results. However, previous studies have found that self-report data are fairly accurate [29]. Further studies are needed to verify the validity of using a self-reporting method to gather information on lifestyles. Second, we did not investigate energy intake. Third, the results were gathered from a cross-sectional sample of elementary school students, thus rendering it difficult to generalize our results. Finally, the small sample resulted in low statistical power.
- Nevertheless, our study had several advantages over previous similar studies because it considered various specific eating behaviors and focused on preadolescents, who have been relatively neglected by previous research. Childhood obesity rates may differ in Asian and Western countries because of the Westernized diet and environment. Thus, this study has value because few studies have been conducted on the distribution of the risk factors for metabolic syndrome and the prevalence of childhood obesity in the Asia-Pacific region. Finally, this study considered factors that are preventable and subject to efforts at prevention.
- This study showed that children who were overweight or obese were considerably more likely to engage in unhealthy eating behaviors. Our results have two clear implications. First, the acquisition of healthy eating habits early in life can contribute to weight control and the reduction of obesity. Second, participation in family meals may be important for preventing childhood obesity.
DISCUSSION
ACKNOWLEDGEMENTS
-
The authors have no conflicts of interest with the material presented in this paper.
-
This article is available at http://jpmph.org/.
Notes
- 1. Childhood obesity. International Obesity Taskforce. cited 2010 Dec 2. Available from: http://www.iotf.org/childhoodobesity.asp
- 2. Oh K, Jang MJ, Lee NY, Moon JS, Lee CG, Yoo MH, et al. Prevalence and trends in obesity among Korean children and adolescents in 1997 and 2005. Korean J Pediatr 2008;51(9):950-955. (Korean)Article
- 3. Hu FB. Sedentary lifestyle and risk of obesity and type 2 diabetes. Lipids 2003;38(2):103-108. 12733740ArticlePubMed
- 4. Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I, et al. Early life risk factors for obesity in childhood: cohort study. BMJ 2005;330(7504):1357. 15908441ArticlePubMedPMC
- 5. US Department of Health and Human Services. Physical activity and health: a report of the surgeon general. 1996. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention
- 6. Newby PK. Are dietary intakes and eating behaviors related to childhood obesity? A comprehensive review of the evidence. J Law Med Ethics 2007;35(1):35-60. 17341216ArticlePubMed
- 7. Kong KA, Park BH, Min JW, Hong J, Hong YS, Lee BE, et al. Clustering of metabolic risk factors and its related risk factors in young schoolchildren. J Prev Med Public Health 2006;39(3):235-242. (Korean). 16764498PubMed
- 8. 2007 Korean children and adolescents growth standard. Korea Centers for Disease Control and Prevention. cited 2009 Sep 28. Available from: http://www.cdc.go.kr/kcdchome/jsp/home/common/brd/COMMBRD0200Detail.jsp?menuid=100049&boardid=1012&pageNum=0&sub=0&boardseq=20915
- 9. Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med 2003;157(8):821-827. 12912790ArticlePubMed
- 10. Overweight and obesity. consequences. Centers for Disease Control and Prevention. cited 2009 Feb 27. Available from: http://www.cdc.gov/NCCDPHP/DNPA/obesity/childhood/consequences.htm
- 11. Sugimori H, Yoshida K, Izuno T, Miyakawa M, Suka M, Sekine M, et al. Analysis of factors that influence body mass index from ages 3 to 6 years: A study based on the Toyama cohort study. Pediatr Int 2004;46(3):302-310. 15151547ArticlePubMed
- 12. Gortmaker SL, Must A, Sobol AM, Peterson K, Colditz GA, Dietz WH. Television viewing as a cause of increasing obesity among children in the United States, 1986-1990. Arch Pediatr Adolesc Med 1996;150(4):356-362. 8634729ArticlePubMed
- 13. Lowry R, Wechsler H, Galuska DA, Fulton JE, Kann L. Television viewing and its associations with overweight, sedentary lifestyle, and insufficient consumption of fruits and vegetables among US high school students: differences by race, ethnicity, and gender. J Sch Health 2002;72(10):413-421. 12617028ArticlePubMed
- 14. Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA 2003;289(14):1785-1791. 12684356ArticlePubMed
- 15. Ainsworth BE, Haskell WL, Leon AS, Jacobs DR Jr, Montoye HJ, Sallis JF, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc 1993;25(1):71-80. 8292105ArticlePubMed
- 16. Metcalf BS, Hosking J, Jeffery AN, Voss LD, Henley W, Wilkin TJ. Fatness leads to inactivity, but inactivity does not lead to fatness: a longitudinal study in children (EarlyBird 45). Arch Dis Child doi: 10.1136/adc.2009.175927Article
- 17. Harris KC, Kuramoto LK, Schulzer M, Retallack JE. Effect of school-based physical activity interventions on body mass index in children: a meta-analysis. CMAJ 2009;180(7):719-726. 19332753ArticlePubMedPMC
- 18. Lank NH, Vickery CE, Cotugna N, Shade DD. Food commercials during television soap operas: what is the nutrition message? J Community Health 1992;17(6):377-384. 1293143ArticlePubMed
- 19. Dietz WH Jr, Gortmaker SL. Do we fatten our children at the television set? Obesity and television viewing in children and adolescents. Pediatrics 1985;75(5):807-812. 3873060ArticlePubMedPDF
- 20. Hu FB, Leitzmann MF, Stampfer MJ, Colditz GA, Willett WC, Rimm EB. Physical activity and television watching in relation to risk for type 2 diabetes mellitus in men. Arch Intern Med 2001;161(12):1542-1548. 11427103ArticlePubMed
- 21. Sallis JF, Glanz K. The role of built environments in physical activity, eating, and obesity in childhood. Future Child 2006;16(1):89-108. 16532660ArticlePubMed
- 22. Barkeling B, Ekman S, Rossner S. Eating behaviour in obese and normal weight 11-year-old children. Int J Obes Relat Metab Disord 1992;16(5):355-360. 1319970PubMed
- 23. Otsuka R, Tamakoshi K, Yatsuya H, Murata C, Sekiya A, Wada K, et al. Eating fast leads to obesity: findings based on self-administered questionnaires among middle-aged Japanese men and women. J Epidemiol 2006;16(3):117-124. 16710080ArticlePubMedPMC
- 24. Ford AL, Bergh C, Sodersten P, Sabin MA, Hollinghurst S, Hunt LP, et al. Treatment of childhood obesity by retraining eating behaviour: randomised controlled trial. BMJ 2010;340: b5388. 20051465Article
- 25. Yannakoulia M, Papanikolaou K, Hatzopoulou I, Efstathiou E, Papoutsakis C, Dedoussis GV. Association between family divorce and children's BMI and meal patterns: the GENDAI Study. Obesity (Silver Spring) 2008;16(6):1382-1387. 18369339ArticlePubMed
- 26. Birch LL, Fisher JO, Davison KK. Learning to overeat: maternal use of restrictive feeding practices promotes girls' eating in the absence of hunger. Am J Clin Nutr 2003;78(2):215-220. 12885700ArticlePubMedPMC
- 27. Anderson SE, Whitaker RC. Household routines and obesity in US preschool-aged children. Pediatrics 2010;125(3):420-428. 20142280ArticlePubMed
- 28. Gable S, Chang Y, Krull JL. Television watching and frequency of family meals are predictive of overweight onset and persistence in a national sample of school-aged children. J Am Diet Assoc 2007;107(1):53-61. 17197271ArticlePubMed
- 29. Orsini N, Bellocco R, Bottai M, Hagstromer M, Sjostrom M, Pagano M, et al. Validity of self-reported total physical activity questionnaire among older women. Eur J Epidemiol 2008;23(10):661-667. 18704705ArticlePubMed
REFERENCES
| Total (n = 261) | Normal (n = 213) | Overweight (n = 29) | Obese (n = 19) | |
|---|---|---|---|---|
| Sex (male) | 136 (52.1) | 115 (54.0) | 11 (38.0) | 10 (52.6) |
| Age (y) | 8.21 (±0.70) | 8.19 (±0.69) | 8.38 (±0.68) | 8.11 (±0.81) |
| Height (cm)** | 132.16 (±5.75) | 131.29 (±5.37) | 135.83 (±4.88) | 136.33 (±7.15) |
| Weight (kg)** | 31.03 (±6.66) | 28.86 (±4.03) | 37.89 (±3.74) | 44.89 (±9.63) |
| Parental factors | ||||
| Father’s BMI (kg/m2)* | 23.53 (±2.32) | 23.45 (±2.26) | 23.39 (±2.05) | 24.70 (±3.10) |
| Mother’s BMI (kg/m2)** | 21.33 (±2.45) | 21.11 (±2.33) | 21.49 (±2.00) | 23.44 (±3.26) |
| Father’s education (n = 258) | ||||
| Middle school | 6 (2.3) | 4 (1.9) | 1 (3.5) | 1 (5.3) |
| High school | 47 (18.2) | 36 (17.1) | 7 (24.1) | 4 (21.1) |
| College | 205 (79.5) | 170 (81.0) | 21 (72.4) | 14 (73.7) |
| Mother’s education† (n = 259) | ||||
| Middle school | 6 (2.3) | 4 (1.9) | 1 (3.5) | 1 (5.3) |
| High school | 103 (39.8) | 78 (37.0) | 17 (58.6) | 8 (42.1) |
| College | 150 (57.9) | 129 (61.1) | 11 (37.9) | 10 (52.6) |
| Parental diabetes* | 6 (2.3) | 3 (1.4) | 1 (3.5) | 2 (10.5) |
| Parental hypertension | 15 (5.8) | 11 (5.2) | 2 (6.9) | 2 (10.5) |
| Metabolic components | ||||
| WC (cm)** | 60.97 (±7.06) | 58.67 (±4.42) | 67.47 (±4.17) | 76.82 (±8.08) |
| SBP (mmHg)** | 108.16 (±9.67) | 106.51 (±8.49) | 114.83 (±10.78) | 116.53 (±11.98) |
| DBP (mmHg)** | 63.15 (±8.14) | 62.10 (±7.47) | 64.76 (±9.02) | 72.47 (±8.00) |
| Glucose (mg/dL) | 85.97 (±7.57) | 86.05 (±8.02) | 87.07 (±4.91) | 83.42 (±4.96) |
| Triglycerides (mg/dL)† | 62.66 (±1.61) | 62.65 (±1.59) | 55.13 (±1.55) | 76.22 (±1.86) |
| HDL cholesterol l (mg/dL)* | 60.67 (±10.39) | 60.72 (±10.33) | 63.55 (±11.06) | 55.63 (±8.49) |
BM: body mass index, WC: waist circumference, SBP: systolic blood pressure, DBP: diastolic blood pressure, HDL: high-density lipoprotein.
1 Numbers vary slightly due to missing data. Numerical values indicate the mean (± standard deviation) and categorical values are given as n (%).
† p < 0.1,
* p < 0.05,
** p < 0.001.
| Total (n = 261) | Normal (n = 213) | Overweight (n = 29) | Obese (n = 19) | p-value | |
|---|---|---|---|---|---|
| Waist circumference1 | 23 (8.8) | 1 (0.5) | 4 (13.8) | 18 (94.7) | <0.000 |
| Elevated BP1 | 73 (28.0) | 47 (22.1) | 13 (44.8) | 13 (68.4) | <0.000 |
| High glucose2 | 2 (0.8) | 2 (0.9) | 0.0 | 0.0 | 0.80 |
| High triglycerides2 | 24 (9.2) | 19 (8.9) | 0.0 | 5 (26.3) | <0.01 |
| Low HDL cholesterol3 | 7 (2.7) | 5 (2.4) | 1 (3.5) | 1 (5.3) | <0.73 |
| Clustering of metabolic risk factors | |||||
| ≥ 3 | 6 (2.3) | 2 (0.9) | 0.0 | 4 (21.1) | <0.0004 |
| 2 | 16 (6.1) | 4 (1.9) | 2 (6.9) | 10 (52.6) | |
| 1 | 78 (29.9) | 60 (28.2) | 14 (48.3) | 4 (21.1) | |
| 0 | 161 (61.7) | 147 (69.0) | 13 (44.4) | 1 (5.3) |
| Lifestyle factors | Normal | Overweight (BMI ≥ 85th percentile) | p-value |
|---|---|---|---|
| Physical activity (n = 261) | |||
| High (≥5 d/ wk) | 33 / 213 (15.5) | 7 / 48 (14.6) | 0.47 |
| Moderate (3-4 d/ wk) | 115 / 213 (54.0) | 22 / 48 (45.8) | |
| Low (<3 d/wk) | 65 / 213 (30.5) | 19 / 48 (39.6) | |
| Watch TV (n = 232) | |||
| < 1 h/d | 66 / 188 (35.1) | 12 / 44 (27.3) | 0.07 |
| 1 - 2 h/ d | 70 / 188 (37.2) | 12 / 44 (27.3) | |
| > 2 h/ d | 52 / 188 (27.7) | 20 / 44 (45.4) | |
| Eating behaviors | |||
| Overeating (≥2-3 times/wk) (n = 239) | 53 / 193 (27.5) | 28 / 46 (60.9) | <0.000 |
| Eating precooked/frozen food (≥1 time/d) (n = 252) | 11 / 208 (5.3) | 4 / 44 (9.1) | 0.31 |
| Eating out (≥1-3 times/wk) (n = 258) | 37 / 211 (17.5) | 9 / 47 (19.2) | 0.96 |
| Rate of eating* (n = 260) | |||
| Slow | 65 / 212 (30.7) | 1 / 48 (2.1) | <0.000 |
| Moderate | 115 / 212 (54.2) | 27 / 48 (56.2) | |
| Fast | 32 / 212 (15.1) | 20 / 48 (41.7) | |
| Family meals (n = 260) | |||
| 1/d | 116 / 212 (54.7) | 28 / 48 (58.3) | 0.03 |
| 4 - 6/wk | 29 / 212 (13.7) | 6 / 48 (12.5) | |
| 1 - 3/wk | 62 / 212 (29.2) | 9 / 48 (18.8) | |
| 2 - 3/mo | 5 / 212 (2.4) | 5 / 48 (10.4) |
|
Univariate |
Model 1 |
Model 2 |
|
|---|---|---|---|
| OR (95% CI) | aOR (95% CI) | aOR (95% CI) | |
| Watch TV | |||
| < 1 h/ d | 1.00 | 1.00 | 1.00 |
| 1 - 2 h/ d | 0.98 (0.43 - 2.19) | 0.95 (0.38 - 2.36) | 1.02 (0.39 - 2.69) |
| > 2 h/ d | 2.19 (1.04 - 4.59)† | 1.49 (0.62 - 3.63) | 1.29 (0.51 - 3.31) |
| Eating behaviors | |||
| Overeating (≥2-3 times/wk) | 4.11 (2.10 - 8.04)*** | 3.06 (1.43 - 6.55)* | 3.10 (1.39 - 6.92)* |
| Rate of eating† | 3.87 (2.24 - 6.67)*** | 3.28 (1.73 - 6.24)** | 3.28 (1.68 - 6.41)** |
| Family meal | |||
| 1 / day | 1.00 | 1.00 | 1.00 |
| 4 - 6 times/wk | 0.87 (0.33 - 2.28) | 0.93 (0.31 - 2.84) | 1.24 (0.38 - 4.00) |
| 1 - 3 times/wk | 0.61 (0.27 - 1.37) | 0.59 (0.24 - 1.44) | 0.66 (0.25 - 1.71) |
| 2 - 3 times/mo | 4.18 (1.13 - 15.43)† | 7.11 (1.07 - 47.20)† | 9.51 (1.21 - 74.82)† |
Figure & Data
References
Citations

- Identifying subgroups of eating behavior traits unrelated to obesity using functional connectivity and feature representation learning
Hyoungshin Choi, Kyoungseob Byeon, Jong‐eun Lee, Seok‐Jun Hong, Bo‐yong Park, Hyunjin Park
Human Brain Mapping.2024;[Epub] CrossRef - Associations between School Lunch and Obesity in Korean Children and Adolescents Based on the Korea National Health and Nutrition Examination Survey 2017–2019 Data: A Cross-Sectional Study
Yeji Kim, Kumhee Son, Jieun Kim, Miji Lee, Kyung-Hee Park, Hyunjung Lim
Nutrients.2023; 15(3): 698. CrossRef - First body fat reference curves for Macedonian children and adolescents: the MAKFIT study
Danilo Bojanic, Milovan Ljubojevic, Seryozha Gontarev, Georgi Georgiev, Lence Aleksovska Velickovska
Nutrición Hospitalaria.2023;[Epub] CrossRef - Early childhood eating behaviors associated with risk of overweight and its socio-ecological determinants in Korean preschool children
Yeri Kim, Jiye Kim, Bomi Lee, Seungyoun Jung, Seo-Jin Chung, Hyekyeong Kim, Nana Shin, Yuri Kim
Nutrition Research and Practice.2023; 17(4): 717. CrossRef - Yemekte Küçük Bir Gurme Olun: Çocuklarda ve Adölesanlarda Yeme Farkındalığı
Büşra ÖZYALÇIN, Sine YILMAZ
Gümüşhane Üniversitesi Sağlık Bilimleri Dergisi.2022; 11(1): 355. CrossRef - The association and mediation role of Food and Nutrition Literacy (FNLIT) with eating behaviors, academic achievement and overweight in 10–12 years old students: a structural equation modeling
Azam Doustmohammadian, Nasrin Omidvar, Nastaran Keshavarz-Mohammadi, Hassan Eini-Zinab, Maryam Amini, Morteza Abdollahi
Nutrition Journal.2022;[Epub] CrossRef - Eating Behavior Associated with Food Intake in European Adolescents Participating in the HELENA Study
Ivie Maneschy, Luis A. Moreno, Azahara I. Ruperez, Andrea Jimeno, María L. Miguel-Berges, Kurt Widhalm, Anthony Kafatos, Cristina Molina-Hidalgo, Dénes Molnar, Fréderic Gottrand, Cinzia Le Donne, Yannis Manios, Evangelia Grammatikaki, Marcela González-Gro
Nutrients.2022; 14(15): 3033. CrossRef - Psychological, Morphological, and Dietary Aspects of Eating Disorders in Youth
O V Filatova, E V Kutseva
IOP Conference Series: Earth and Environmental Science.2021; 670(1): 012022. CrossRef - The COMET study: Examining the effects of COVID-19-related perceived stress on Los Angeles Mothers’ dysregulated eating behaviors, child feeding practices, and body mass index
Shirlene D. Wang, Shivali Devjani, Mahima Chillakanti, Genevieve F. Dunton, Tyler B. Mason
Appetite.2021; 163: 105209. CrossRef - Parent–Infant Attachment Insecurity and Emotional Eating in Adolescence: Mediation through Emotion Suppression and Alexithymia
Roseriet Beijers, Marta Miragall, Yvonne van den Berg, Hanna Konttinen, Tatjana van Strien
Nutrients.2021; 13(5): 1662. CrossRef - Insufficient Sleep and Poor Sleep Quality Completely Mediate the Relationship between Financial Stress and Dietary Risk among Higher Education Students
Chen Du, Wenyan Wang, Pao Ying Hsiao, Mary-Jon Ludy, Robin M. Tucker
Behavioral Sciences.2021; 11(5): 69. CrossRef - Effects of intragastric balloon on obesity in obese Korean women for 6 months post removal
Hyeon-Ju Pak, Ha-Neul Choi, Hong-Chan Lee, Jung-Eun Yim
Nutrition Research and Practice.2021; 15(4): 456. CrossRef - Genetic, Environmental and Lifestyle Determinants of Accelerated Telomere Attrition as Contributors to Risk and Severity of Multiple Sclerosis
Michael Hecker, Jan Bühring, Brit Fitzner, Paulus Stefan Rommer, Uwe Klaus Zettl
Biomolecules.2021; 11(10): 1510. CrossRef - The orbitofrontal cortex functionally links obesity and white matter hyperintensities
Bo-yong Park, Kyoungseob Byeon, Mi Ji Lee, Se-Hong Kim, Hyunjin Park
Scientific Reports.2020;[Epub] CrossRef - Plasma fatty acid profile is related to cognitive function in obese Chinese populations (35–64 years): A cross‐sectional study
Qi Duan, Rong Fan, Ruqing Lei, Weiwei Ma, Bingjie Ding
Food Science & Nutrition.2020; 8(9): 4773. CrossRef - Multivariate association between brain function and eating disorders using sparse canonical correlation analysis
Hyebin Lee, Bo-yong Park, Kyoungseob Byeon, Ji Hye Won, Mansu Kim, Se-Hong Kim, Hyunjin Park, Tyler Davis
PLOS ONE.2020; 15(8): e0237511. CrossRef - The Impact of Group and Individual Therapy on the Correction of Food Behavioral Reactions of Patients with Chronic Non-Communicable Diseases
A. Shalimova, A. Isayeva, M. Vovchenko, L. Rieznik, O. Buriakovska, N. Emelyanova
Ukraïnsʹkij žurnal medicini, bìologìï ta sportu.2019; 4(1): 155. CrossRef - The Effect of Family-Based Empowerment on Obesity among Adolescents in Tana Toraja
R. Erni Yetti, Muhammad Syafar, Andi Zulkifli, Rahayu Indriasari, Burhanuddin Bahar, Suriah ., Agus Bintara Birawida, Bagoes Widjanarko, Zadrak Tombeg, Saskiyanto Manggabara, Anto J. Hadi
Pakistan Journal of Nutrition.2019; 18(9): 866. CrossRef - Dynamic functional connectivity analysis reveals improved association between brain networks and eating behaviors compared to static analysis
Bo-yong Park, Taesup Moon, Hyunjin Park
Behavioural Brain Research.2018; 337: 114. CrossRef - Attachment and eating: A meta-analytic review of the relevance of attachment for unhealthy and healthy eating behaviors in the general population
Aida Faber, Laurette Dubé, Bärbel Knäuper
Appetite.2018; 123: 410. CrossRef - First Reference Curve for Body Fat Percentage Among Schoolchildren of Babol in the North of Iran: An International Comparison
Hoda Tavakoli, Mahmoud Hajiahmadi, Haleh Esmaili, Reza Ghadimi
Journal of Pediatrics Review.2018;[Epub] CrossRef - Current Evidence on Vitamin D Deficiency and Metabolic Syndrome in Obese Children: What Does the Evidence from Saudi Arabia Tell Us?
Asma Alaklabi, Naser Alsharairi
Children.2018; 5(1): 11. CrossRef - Descriptive epidemiology of metabolic syndrome among obese adolescent population
Sharmin Mahbuba, Fauzia Mohsin, Farhana Rahat, Jebun Nahar, Tahmina Begum, Nazmun Nahar
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2018; 12(3): 369. CrossRef - Estimation of psychological features, body composition and status of actual nutrition of women with eating behavior disorders
Olga V. Filatova, Sergei S. Polovinkin, Irina V. Chervova, Evgenia I. Baklanova, Irina O. Plyasova
Obesity and metabolism.2018; 15(3): 28. CrossRef - Executive functioning and dietary intake: Neurocognitive correlates of fruit, vegetable, and saturated fat intake in adults with obesity
Emily P. Wyckoff, Brittney C. Evans, Stephanie M. Manasse, Meghan L. Butryn, Evan M. Forman
Appetite.2017; 111: 79. CrossRef - Effectiveness of a mouth rinsing function test for evaluating the oral function of children
Ayano Ogawa, Akiko Ishizaki, Takuya Asami, Hyosong Kwon, Kanako Fujii, Kimiko Kasama, Akinobu Tanaka, Shouji Hironaka
Pediatric Dental Journal.2017; 27(2): 85. CrossRef - Evaluation of a Smart Fork to Decelerate Eating Rate
Sander Hermsen, Jeana H. Frost, Eric Robinson, Suzanne Higgs, Monica Mars, Roel C.J. Hermans
Journal of the Academy of Nutrition and Dietetics.2016; 116(7): 1066. CrossRef - Functional brain networks associated with eating behaviors in obesity
Bo-yong Park, Jongbum Seo, Hyunjin Park
Scientific Reports.2016;[Epub] CrossRef - Overweight/Obesity, Eating Behaviors and Behavioral Problems Among School-age Children
Arunrat Charoenarp, Orawan Louthrenoo, Kulnipa Kittisakmo
Asian Journal of Clinical Nutrition.2016; 9(1): 30. CrossRef - Prevalence of overweight/obesity in relation to dietary habits and lifestyle among 7–17 years old children and adolescents in Lithuania
Natalija Smetanina, Edita Albaviciute, Veslava Babinska, Lina Karinauskiene, Kerstin Albertsson-Wikland, Ausra Petrauskiene, Rasa Verkauskiene
BMC Public Health.2015;[Epub] CrossRef - Executive functions and consumption of fruits/ vegetables and high saturated fat foods in young adults
Christine A Limbers, Danielle Young
Journal of Health Psychology.2015; 20(5): 602. CrossRef - Association Between Eating Speed and Metabolic Syndrome in a Three-Year Population-Based Cohort Study
Bing Zhu, Yasuo Haruyama, Takashi Muto, Takako Yamazaki
Journal of Epidemiology.2015; 25(4): 332. CrossRef - Sex differences in rates of obesity in bipolar disorder: postulated mechanisms
Anusha Baskaran, Danielle S Cha, Alissa M Powell, Dalya Jalil, Roger S McIntyre
Bipolar Disorders.2014; 16(1): 83. CrossRef - Overview of Noncommunicable Diseases in Korean Children and Adolescents: Focus on Obesity and Its Effect on Metabolic Syndrome
Hye Ah Lee, Hyesook Park
Journal of Preventive Medicine and Public Health.2013; 46(4): 173. CrossRef - Frequency of family meals and childhood overweight: a systematic review
J. Valdés, F. Rodríguez‐Artalejo, L. Aguilar, M. B. Jaén‐Casquero, M. Á. Royo‐Bordonada
Pediatric Obesity.2013;[Epub] CrossRef - Dietary behaviors as associated factors for overweight and obesity in a sample of adolescents from Aquitaine, France
Caroline Carriere, Coralie Langevin, Thierry Lamireau, Sylvie Maurice, Hélène Thibault
Journal of Physiology and Biochemistry.2013; 69(1): 111. CrossRef - Effect of organic school meals to promote healthy diet in 11–13 year old children. A mixed methods study in four Danish public schools
Chen He, Soren Breiting, Federico J.A. Perez-Cueto
Appetite.2012; 59(3): 866. CrossRef
 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


