Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 44(5); 2011 > Article
-
Original Article
Preventable Lifestyle Risk Factors for Non-Communicable Diseases in the Pakistan Adolescents Schools Study 1 (PASS-1) - Ali Khan Khuwaja1, Saleem Khawaja2, Komal Motwani2, Adeel Akbar Khoja2, Iqbal Syed Azam3, Zafar Fatmi4, Badar Sabir Ali5, Muhammad Masood Kadir6
-
Journal of Preventive Medicine and Public Health 2011;44(5):210-217.
DOI: https://doi.org/10.3961/jpmph.2011.44.5.210
Published online: September 28, 2010
1Department of Family Medicine, Aga Khan University, Karachi, Pakistan.
2Dow University of Health Sciences, Karachi, Pakistan.
3Department of Community Health Sciences, Aga Khan University, Karachi, Pakistan.
4Devision of Environmental Health Sociences, Karachi, Pakistan.
5Mental Health Association of Pakistan, Karachi, Pakistan.
6Department of Community Health Sciences, Aga Khan University, Karachi, Pakistan.
- Corresponding author: Ali Khan Khuwaja, MD, FCPS. Stadium Road, Karachi 74800, Pakistan. Tel: +92-21-486-4922, Fax: +92-21-493-4294, ali.khuwaja@aku.edu
Copyright © 2011 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- The rising burden of preventable risk factors for non-communicable diseases (NCDs) among adolescents is a major public health challenge worldwide. We identified the preventable risk factors for NCDs in adolescents.
-
Methods
- In a school-based study, pre-tested structured questionnaires were completed by 414 adolescents (14 to 17 years) at six schools in three cities in Pakistan. The chi-squared test and adjusted odds ratio (aOR) with 95% confidence interval (CI) were calculated in a multinomial logistic regression analysis.
-
Results
- Over 80% of the adolescents had unhealthy diets, and 54% were physically inactive. Most adolescents were exposed to passive smoking, and 14% were also current smokers. More than one-third of participants chewed betel nut, and one-quarter used oral tobacco. More girls were physically inactive (OR, 4.07; 95% CI, 2.69 to 6.17), whereas a greater proportion of boys were current smokers (OR, 2.17; 95% CI, 1.19 to 3.91), exposed to passive smoking (OR, 2.57; 95% CI, 1.72 to 3.83), and using betel nut (OR, 2.03; 95% CI, 1.34 to 3.06). Only 3.1% of the participants were without any preventable lifestyle risk factor for NCDs, and over 80% had ≥2 factors. Co-existence of risk factors was independently associated with fathers being blue-collar workers (aOR, 3.57; 95% CI, 1.07 to 11.92) and parents not treating their child fairly (aOR, 5.05; 95% CI, 1.29 to 19.78).
-
Conclusions
- Most of the adolescents studied had preventable risk factors for NCDs. These results warrant comprehensive and integrated interventions to prevent lifestyle risk factors, and parents are front-line stakeholders.
- Non-communicable diseases (NCDs) and their associated risk factors have emerged rapidly and are becoming a major public health challenge worldwide. The impact of NCDs is devastating in terms of premature morbidity, mortality, and economic loss [1,2]. There is an extensive literature demonstrating that NCDs are more likely to occur with unhealthy diet, physical inactivity, active and passive smoking, and use of betel nut and smokeless tobacco (SLT) [2-5], whereas prevention of these factors has positive effects on reducing NCDs rates and all-cause mortality [5,6]. It has been reported that up to 80% of deaths due to heart disease, stroke, and type 2 diabetes and 40% of deaths due to cancers could be prevented by eliminating known lifestyle risk factors [1].
- It is well established that the co-existence of two or more risk factors is associated with increased risk of developing NCDs than would be expected on the basis of the sum of the separate effects [7-9]. It is thus important to investigate the co-existence patterns of preventable risk factors, which may help in developing and implementing integrated preventative strategies. With some exceptions, most previously reported work from various countries has either investigated the combination of biological and clinical risk factors for NCDs in the general population [7,8] or has studied specific groups of adults and elderly populations [10,11], thus missing adolescents, who represent more than one-fifth of the world's population (more than 1.2 billion) [12].
- The World Health Organization has already warned of increasing NCDs among adolescents as a major public health problem [13]. The importance of this age group also lies in the fact that many serious diseases in adulthood have their roots in adolescence [12,14]. For these reasons, we sought to assess the proportion of preventable lifestyle risk factors for NCDs, to evaluate the degree of co-existence of these factors, and to determine any gender-specific differences in these factors among adolescents in Pakistan.
- Parents are always supposed to be the first teachers and trainers of their child. Children and adolescents usually spend a large proportion of their time with their parents, whose affection, liking, and care contribute vitally towards the health habits of their children. However, data are very scarce about parental factors associated with children's practicing healthy habits. In this study we also identified parental factors that are associated with co-existence of risk factors among study participants.
- Considering the great significance of maintaining good health in younger age groups, this multi-center work is of importance and will add to the international assessment literature and provide insights regarding preventable risk factors for NCDs among this part of the population. This work will provide a basis for further research and interventions in adolescents for the prevention of NCDs.
INTRODUCTION
- The Pakistan Adolescents Schools Survey 1 (PASS-1) was conducted in six secondary schools in three major cities (Karachi, Lahore, Quetta) in Pakistan in 2009. The schools included in this study represent the public and private sectors. In total, there were 432 students enrolled in the 9th and 10th grades in these schools; of these, 414 students participated, five were absent on the day of the interview, and 13 students did not agree to participate in this study. Permission was given by the school administration at all participating schools to conduct the study in their schools. Assent from study participants and consent from their parents were obtained before conducting the study. Earlier, the study protocol and questionnaire were also reviewed by the departmental research committee for possible ambiguities and ethical concerns.
- After an extensive literature search of related studies and questionnaires and with a consensus of the study investigators, a self-administered structured questionnaire was developed for this study. We identified six preventable lifestyle risk factors that are strongly associated with various types of NCDs. These were defined as:
-
Unhealthy dietary intake: <7 servings of fruits and/or vegetable in the last 7 days.
Physical inactivity: <30 minutes of moderate-to-vigorous activity for 4 or more days in the last 7 days.
Passive smoking: at least 30 minutes exposure to second-hand smoke most days of the week (at least 5) either at home, in public places, and/or at school for at least the last 6 months.
Current smoking: any number of cigarettes currently smoked, either regularly or occasionally.
Use of betel nut: any amount of betel nut chewed in the last 7 days.
Use of SLT: any amount of SLT (oral tobacco, snuff) used in the last 7 days.
- Parental educational level and working categories were also noted. Fathers who were working as professionals, administrators, bankers, and teachers were labeled as having a white-collar job, whereas those who were working in other categories, such as sellers, laborers, and manual workers, were labeled as having a blue-collar job. Additionally, students were asked two questions about their self-perception regarding their parents (Do you think your parents understand your worries and problems? Do you think your parents treat you fairly?). Both questions were obviously subjective, and participants responded 'yes' or 'no.' After determining face and content validity, the questionnaire was piloted among 50 students of the same age group in a separate school that was not included in the main study. The final questionnaire was distributed to all students in their classrooms, and they were asked to complete the questionnaire. Completion of the questionnaire required about 30 minutes. Study investigators were present during the data collection process to answer questions.
- A variable consisting of co-existence of preventable lifestyle risk factors for NCDs was created using unhealthy diet, physical inactivity, passive smoking, current smoking, current use of betel nut, and current exposure of smokeless tobacco. This variable was categorized into none, one, two, three, and four or more risk factors and was used as a dependent variable. Conversely, gender of study participant, educational level of mother and father, working status of mother and father, and parents' understanding of the adolescent and parents' fairness with the adolescent were used as independent variables.
- Data were analyzed using the SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). Frequencies and proportions were calculated for baseline characteristics of study participants and preventable lifestyle risk factors. The co-existence of risk factors was categorized as none, one, two, three, and four or more. To determine the difference in risk factors by gender and parental factors, the chi-squared test and unadjusted and adjusted odds ratios were calculated. In this study, the dependent variable was multi-categorical, and multinomial logistic regression analysis was used in the final model, adjusting for gender.
METHODS
- The age of the study participants ranged from 14 to 17 years, and all resided in urban areas. The distribution of the study participants by gender and parental factors is summarized in Table 1. The sample included a slight preponderance (53.9%) of boys. Over half (54.3%) of the adolescents' fathers had 13 years or more of schooling, and 40.6% of the mothers had a similar level of schooling. Half of the study participants' fathers had white-collar jobs, whereas most (80.2%) of the mothers were housewives. About one-third (31.9%) of the adolescents perceived that their parents had no understanding of them, and 38.4% also reported that their parents did not treat them fairly.
- Over 80% of the adolescents had an unhealthy diet, and this was almost equal between boys and girls (p=0.47). Over 54% of the study participants were physically inactive, and this was true of more girls than boys (p<0.001). Boys were more exposed to passive smoking (p<0.001) and more were current smokers (p=0.009). Similarly, more boys than girls chewed betel nut (p<0.001). About onequarter of the study participants were using SLT, and this was equal in boys and girls (Table 1).
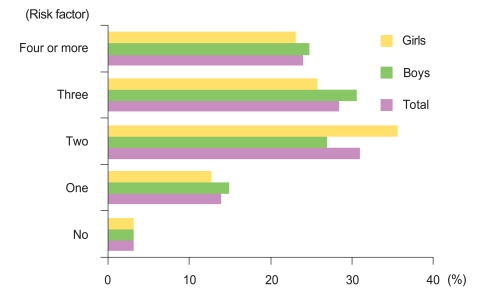
- The pattern of the co-existence of preventable risk factors for NCDs among adolescents is shown in Figure 1. Only 3.1% (boys, 3.1%; girls, 3.1%) of study participants were without any preventable risk factor for NCDs, whereas 13.8% (boys, 14.8%; girls, 12.6%) had one of these factors. About one-third of adolescents (boys, 26.9%; girls, 35.6%) had two, and 28.3% (boys, 30.5%; girls, 25.7%) had three of these preventable risk factors present. About one-quarter of the adolescents had four or more of the risk factors. The overall distribution of the number of coexisting risk factors was not significantly different between boys and girls (χ2=3.855; df=4; p=0.43).
- Table 2 shows odds ratios with 95% confidence intervals (CIs) of co-existence of preventable risk factors for NCDs with gender and parental characteristics of the study participants. Adolescents whose parents were not treating them fairly were more likely to have four or more preventable risk factors for NCDs. The pattern of the co-existence of these risk factors was also higher among adolescents whose fathers worked at blue-collar jobs. In the final model (Table 3), study participants whose fathers worked at blue-collar jobs were about four times more likely to have four or more preventable lifestyle risk factors adjusted odd ratios (aOR), 3.57; 95% CI, 1.07 to 11.92. This was found to be even higher among adolescents whose parents were not treating them fairly (aOR, 5.05; 95% CI, 1.29 to 19.78).
RESULTS
- This is one of the few reported studies and the first from Pakistan to describe the proportion and co-existence pattern of preventable risk factors for NCDs and their association with parental characteristics specifically in adolescents. This study of adolescents indicated an alarming level of these risk factors, which are preventable to a major extent and have very important public health consequences.
- Generally, there is a shift from the use of plant foods (vegetables, fruits) to meat and other animal products among adults and children [9,14], and this shift has significantly increased the incidence of various types of NCDs [1,15]. According to the US Centers for Disease Control and Prevention (CDC) [16], fewer than one-quarter of adolescents eat enough fruits and vegetables. A similar unhealthy dietary intake in adolescents has been reported in a small school-based pilot survey in a small city in Pakistan [14]. Another survey conducted among university medical students in Karachi reported that a majority of the students consumed junk food on a regular basis [17]. In this study as well, a large majority of adolescent boys and girls were not consuming adequate amounts of fruits and vegetables. This probably reflects emerging influences and trends in fast-food eateries and dining-out practices. It has also been observed that almost all school canteens have fast-food, deep-fried snacks, and high-calorie sugar-containing drinks available, with minimal amounts of fruits and vegetables. Moreover, it is not uncommon to promote and market fast-food and to have fast-food chains and outlets in schools in Pakistan.
- It has been well reported from various parts of the world that a general trend in physical inactivity has increased over time in both adults [15,18] and adolescents [14,19]. Recently, a community-based survey from urban Pakistan reported that the majority of adults were physically inactive, and this finding was stronger in women than in men [9]. In the present study as well, most of the adolescents, especially girls, were physically inactive. There are several possible explanations for this high proportion of physical inactivity, such as increased interest in watching television and movies and spending more time on computer and video games [9,14]. Generally, there is also a lack of safe outdoor playgrounds and walking tracks in major cities in developing countries, including Pakistan, particularly for girls and women. Another important reason for the high percentage of physically inactive girls may be that in our society, for cultural reasons, girls are generally not permitted to go outside the home and participate in sports or physical activity programs.
- Tobacco use, particularly at younger ages, increases the duration of tobacco exposure, leading to a higher risk of developing NCDs at comparatively early ages, during what are usually thought to be the most productive years of life. Worldwide [20], up to 100 000 children begin smoking every day. Recently, Lee and colleagues reported a prediction model for Korean adolescents' future smoking intentions, which consisted of five determinants: past smoking experience, parental smoking status, friends' smoking status, ownership of a product with a cigarette brand logo, and an offer by a close friend to smoke [21]. Khuwaja and Kadir [22] documented that a majority of adults in urban Pakistan began smoking when they were younger than 25 years; our results are consistent with this, revealing that about 15% of the adolescents labeled themselves as current smokers. Previously, various studies from developing and developed countries have reported that smoking was widespread among men [9,15]. However, our study found that a substantial number of girls were also smokers. A rising trend of smoking in females has also been reported from various other countries, including Japan, Malaysia, and Korea [20]. This emerging trend of smoking among young girls is concerning because along with the general hazards of smoking, there are additional health risks and consequences that are specific to their gender and likely to affect their pregnancies, reproduction generally, and the health of their children. Most of the adolescents in this study were also exposed to passive smoking, another well-proven risk factor for many NCDs [9,22]. Due to a lack of political com-mitment and poor awareness about the health hazards of passive smoking among the general population, smoking is not prohibited in most public places, public transport, or shopping areas in Pakistan.
- Use of betel nut and oral tobacco are also well-established risk factor for various NCDs [4,23]. Nonetheless, their use is widespread throughout the world, and in some countries, betel nut with other ingredients is a traditional item and is served at social, cultural, and entertaining gatherings [23]. Ali et al. recently reported that over half the adults in Karachi were using smokeless tobacco, and a majority of them began this habit before they were 15 years old [4]. In our study also, more than one-third of the adolescents were using betel nut on a regular basis, and about one-quarter of them were using oral tobacco. These results reflect the widespread use of betel nut and oral tobacco by adolescents, which may lead to a higher risk of developing a wide range of NCDs later in their lives.
- The tendency of the preventable risk factors for NCDs to cluster has important implications from a public health perspective [1,9]. The co-existence of risk factors specific for NCDs has been well reported from different parts of the world [11,24]. However, participants in these studies were not adolescents, whose behaviors influence the future course of these diseases. Moreover, some important preventable risk factors were missing from these papers, such as unhealthy diet, betel nuts, and oral tobacco. Belkic and Nedic [10] reported that only 13% of study participants had a low lifestyle-related NCD risk profile (not current smoker, body mass index <28, regular physical activity, no daily alcohol). Similarly, a high burden of lifestyle risk factors was documented by Bolormaa and colleagues in a NCD risk-factor survey among an adult population in Mongolia [24]. Our study also showed that a large number of adolescents had co-existing preventable risk factors for NCDs, and over 80% of the study participants had two or more of these risk factors. This study also revealed that co-existence of these risk factors was equally prevalent in boys and girls.
- Parents and family rearing are very important in helping children to develop healthy habits [14,25]. Additionally, parental occupation and education predict healthy habits in adulthood [26]. The economic well-being of parents and children's social adjustment are also well known play a part in this process [27]. It has been reported that lower economic level affects parenting behaviors through an adverse impact on parental psychological well-being [27]. In our study, children who reported that their parents were not fair with them were five times more likely to have unhealthy lifestyles. This may reflect a gap in the perception of care between child and parent. There are some likely explanations for this attitude in the relationship; probably the most important is a lack of quality time spent together and a lack of attention given by parents to their child. In an urban setting particularly, those who work in blue-collar jobs may be likely to work the longest hours and may be more likely to work on weekends as well; in contrast, those working in white-collar jobs may usually work for specified periods of time in a day and also enjoy more liberty on weekends and holidays. Our findings are consistent with this explanation; adolescents whose parents worked in blue-collar jobs were more likely to have lifestyle risk factors for NCDs.
- This study has some limitations that should be kept in mind. Although the study was conducted in a number of schools and study participants were well represented in each sociodemographic stratum, the results cannot be generalized to all Pakistani adolescents, as non-probabilistic sampling was used in the selection of schools. The questionnaire was developed after an extensive literature search, and the face and content validity were checked by experts; nevertheless, this questionnaire may require further validation before being used for all urban and rural communities in Pakistan. Because the data were collected at schools and smoking is a socially unacceptable habit, underreporting of smoking status may be expected. Moreover, the two questions about parental understanding and fairness with the child were selfperceived, and an element of subjectivity cannot be excluded. The selection of only urban schools is a potential source of selection bias, and these results should not be generalized to adolescents of rural schools. Other confounding biases cannot be ruled out because some other important variables, such as alcohol intake and screening time, were not reported.
- Nevertheless, this study indicated that almost all participants had at least one preventable lifestyle risk factor for NCDs, and co-existence of risk factors was very common. This work could help to guide comprehensive, multifaceted, and integrated interventional programs, which should focus on various health-promoting issues, such as improved access to healthy foods, prohibition of smoking at work and in public places, and restrictions on the sale of cigarettes and other tobacco products to adolescents and school-age children. The availability of and access to safe playing courts and grounds should be assured. Along with discontinuing advertisements and the promotion of unhealthy behaviors and practices in the media, there should be school-based educational strategies to increase knowledge and awareness about the risk factors of NCDs and their prevention. Being important stakeholders in promoting healthy lifestyles in their children, parents should be advised and counseled about good parenting. These preventive steps will provide cost-effective results in comparison with the very costly treatment and management of NCDs later. This study also provides grounds for conducting further research on a larger scale to identify the magnitude of preventable and modifiable risk factors in the development of NCDs and to develop and test educational and preventative interventions.
DISCUSSION
-
The authors have no conflict of interest with the material presented in this paper.
-
This article is available at http://jpmph.org/.
Notes
- 1. 10 facts about chronic diseases. World Health Organization. cited 2011 Jan 11. Available from: http://www.who.int/features/factfiles/chp/en/
- 2. Khuwaja AK, Qureshi R, Fatmi Z. Noncommunicable diseases and injuries: action needed in South Asia too. PLoS Med 2007;4(1):e38. 17411313ArticlePubMedPMC
- 3. Khowaja LA, Khuwaja AK, Nayani P, Jessani S, Khowaja MP, Khowaja S. Quit smoking for life--social marketing strategy for youth: a case for Pakistan. J Cancer Educ 2010;25(4):637-642. 20238199ArticlePubMed
- 4. Ali NS, Khuwaja AK, Ali T, Hameed R. Smokeless tobacco use among adult patients who visited family practice clinics in Karachi, Pakistan. J Oral Pathol Med 2009;38(5):416-421. 19434816ArticlePubMed
- 5. Weiderpass E. Lifestyle and cancer risk. J Prev Med Public Health 2010;43(6):459-471. 21139406ArticlePubMedPDF
- 6. Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V. The Indian Diabetes Prevention Program shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia 2006;49(2):289-297. 16391903ArticlePubMed
- 7. Vikram NK, Tandon N, Misra A, Srivastava MC, Pandey RM, Mithal A, et al. Correlates of Type 2 diabetes mellitus in children, adolescents and young adults in north India: a multisite collaborative case-control study. Diabet Med 2006;23(3):293-298. 16492213ArticlePubMed
- 8. Zhang L, Qin LQ, Cui HY, Liu AP, Wang PY. Prevalence of cardiovascular risk factors clustering among suburban residents in Beijing, China. Int J Cardiol 2011;151(1):46-49. 20471118ArticlePubMed
- 9. Khuwaja AK, Kadir MM. Gender differences and clustering pattern of behavioural risk factors for chronic noncommunicable diseases: community-based study from a developing country. Chronic Illn 2010;6(3):163-170. 20444764ArticlePubMed
- 10. Belkić K, Nedic O. Workplace stressors and lifestyle-related cancer risk factors among female physicians: assessment using the Occupational Stress Index. J Occup Health 2007;49(1):61-71. 17314468ArticlePubMed
- 11. Chou KL. The prevalence and clustering of four major lifestyle risk factors in Hong Kong Chinese older adults. J Aging Health 2008;20(7):788-803. 18562762ArticlePubMed
- 12. Child and adolescent health and development. World Health Organization. cited 2011 Jan 10. Available from: http://www.who.int/child_adolescents_health/topics/prevention_care/adolescents/en
- 13. Michaud P, Suris JC, Viner R. Child and adolescent health and development. The adolescent with a chronic condition. WHO discussion paper on adolescence. 2007. cited 2011 Jan 10. Available from: http://whqlibdoc.who.int/publications/2007/9789241595704_eng.pdf
- 14. Khuwaja AK, Fatmi Z, Soomro WB, Khuwaja NK. Risk factors for cardiovascular disease in school children--a pilot study. J Pak Med Assoc 2003;53(9):396-400. 14620313PubMed
- 15. Taylor VM, Yasui Y, Tu SP, Neuhouser ML, Li L, Woodall E, et al. Heart disease prevention among Chinese immigrants. J Community Health 2007;32(5):299-310. 17922202ArticlePubMed
- 16. Key strategies for schools to prevent obesity. Centers for Disease Control and Prevention (CDC). cited 2011 Jan 10. Available from: http://www.cdc.gov/Features/ChildhoodObesity
- 17. Nisar N, Qadri MH, Fatima K, Perveen S. Dietary habits and life style among the students of a private medical university Karachi. J Pak Med Assoc 2009;59(2):98-101. 19260574PubMed
- 18. Willey JZ, Paik MC, Sacco R, Elkind MS, Boden-Albala B. Social determinants of physical inactivity in the Northern Manhattan Study (NOMAS). J Community Health 2010;35(6):602-608. 20574777ArticlePubMedPMC
- 19. Agazzi H, Armstrong K, Bradley-Klug KL. BMI and physical activity among at-risk sixth- and ninth-grade students, Hillsborough County, Florida, 2005-2006. Prev Chronic Dis 2010;7(3):A48. 20394687PubMedPMC
- 20. Fact sheet: smoking statistics. World Health Organization, Western Pacific Region. cited 2011 Jan 10. Available from: http://www.wpro.who.int/media_centre/fact_sheets/fs_20020528.htm
- 21. Lee S, Yun JE, Lee JK, Kim IS, Jee SH. The Korean prediction model for adolescents' future smoking intensions. J Prev Med Public Health 2010;43(4):283-291. 20689354ArticlePubMedPDF
- 22. Khuwaja AK, Kadir MM. Smoking among adult males in an urban community of Karachi, Pakistan. Southeast Asian J Trop Med Public Health 2004;35(4):999-1004. 15916105PubMed
- 23. Ali NS, Khuwaja AK. In: Preedy VR, Watson RR, Patel VB, editors. Betel nut (Areca catechu) usage and its effects on health. Nuts and seeds in health and disease prevention. 2011. Amsterdam: ElsevierArticle
- 24. Bolormaa N, Narantuya L, De Courten M, Enkhtuya P, Tsegmed S. Dietary and lifestyle risk factors for noncommunicable disease among the Mongolian population. Asia Pac J Public Health 2008;20(Suppl):23-30. 19533858PubMed
- 25. Alderfer MA, Fiese BH, Gold JI, Cutuli JJ, Holmbeck GN, Goldbeck L, et al. Evidence-based assessment in pediatric psychology: family measures. J Pediatr Psychol 2008;33(9):1046-1061. 17905801ArticlePubMedPMC
- 26. Fagan P, Brook JS, Rubenstone E, Zhang C. Parental occupation, education, and smoking as predictors of offspring tobacco use in adulthood: a longitudinal study. Addict Behav 2005;30(3):517-529. 15718068ArticlePubMed
- 27. Mistry RS, Vandewater EA, Huston AC, McLoyd VC. Economic well-being and children's social adjustment: the role of family process in an ethnically diverse low-income sample. Child Dev 2002;73(3):935-951. 12038561ArticlePubMed
REFERENCES
| Parental characteristics and lifestyle risk factors | Total | Boys | Girls | p-value1 |
|---|---|---|---|---|
|
n (%) |
||||
| Parental characteristics | ||||
| Schooling of fathers | ||||
| 13 years or more | 225 (54.3) | 136 (61.0) | 89 (46.6) | 0.003 |
| 0 to 12 years | 189 (45.7) | 87 (39.0) | 102 (52.9) | |
| Schooling of mothers | ||||
| 13 years or more | 168 (40.6) | 91 (40.8) | 77 (40.3) | 0.92 |
| 0 to 12 years | 246 (59.4) | 132 (59.2) | 114 (59.7) | |
| Working status of fathers | ||||
| White-collar job | 210 (50.7) | 115 (51.6) | 95 (49.7) | 0.71 |
| Blue-collar job | 204 (49.3) | 108 (48.4) | 96 (50.3) | |
| Working status of mothers | ||||
| Working | 82 (19.8) | 41 (18.4) | 41 (21.5) | 0.43 |
| Housewife | 332 (80.2) | 182 (81.6) | 150 (78.5) | |
| Parents’ lack of understanding with adolescent | ||||
| No | 282 (68.1) | 152 (68.2) | 130 (68.1) | 0.98 |
| Yes | 132 (31.9) | 71 (31.8) | 61 (31.9) | |
| Parents not treating their adolescent fairly | ||||
| No | 255 (61.6) | 146 (65.5) | 109 (57.1) | 0.08 |
| Yes | 159 (38.4) | 77 (34.5) | 82 (42.9) | |
| Preventable lifestyle risk factors | ||||
| Unhealthy diet | ||||
| No | 80 (19.3) | 46 (20.6) | 34 (17.8) | 0.47 |
| Yes | 334 (80.7) | 177 (79.4) | 157 (82.2) | |
| Physical inactivity | ||||
| No | 189 (45.7) | 136 (61.0) | 53 (27.7) | <0.001 |
| Yes | 225 (54.3) | 87 (39.0) | 138 (72.3) | |
| Passive smoking | ||||
| No | 183 (44.2) | 75 (33.6) | 108 (56.5) | <0.001 |
| Yes | 231 (55.8) | 148 (66.4) | 83 (43.5) | |
| Current smoking | ||||
| No | 355 (85.7) | 182 (81.6) | 173 (90.6) | 0.009 |
| Yes | 59 (14.3) | 41 (18.4) | 18 (9.4) | |
| Betel nut use | ||||
| No | 261 (63.0) | 124 (55.6) | 137 (71.7) | <0.001 |
| Yes | 153 (37.0) | 99 (44.4) | 54 (28.3) | |
| Smokeless tobacco | ||||
| No | 313 (75.6) | 167 (74.9) | 146 (76.4) | 0.71 |
| Yes | 101 (24.4) | 56 (25.1) | 45 (23.6) | |
| Independent variables |
Preventable lifestyle risk factors1 |
|||
|---|---|---|---|---|
| One | Two | Three | Four or more | |
| Gender | ||||
| Boys | 1.00 | 1.00 | 1.00 | 1.00 |
| Girls | 0.85 (0.25, 2.85) | 1.32 (0.42, 4.15) | 0.84 (0.27, 2.66) | 0.93 (0.29, 2.98) |
| Schooling of fathers | ||||
| 13 years or more | 1.00 | 1.00 | 1.00 | 1.00 |
| 0 to 12 years | 0.98 (0.29, 3.28) | 0.97 (0.31, 3.04) | 0.93 (0.30, 2.95) | 1.05 (0.33, 3.36) |
| Schooling of mothers | ||||
| 13 years or more | 1.00 | 1.00 | 1.00 | 1.00 |
| 0 to 12 years | 2.16 (0.64, 7.30) | 1.76 (0.56, 5.54) | 1.51 (0.48, 4.77) | 1.79 (0.56, 5.74) |
| Working status of fathers | ||||
| White-collar job | 1.00 | 1.00 | 1.00 | 1.00 |
| Blue-collar job | 1.44 (0.42, 4.94) | 1.06 (0.33, 3.42) | 1.42 (0.44, 4.59) | 3.20 (0.97, 10.55) |
| Working status of mothers | ||||
| Working | 1.00 | 1.00 | 1.00 | 1.00 |
| Housewife | 1.34 (0.25, 6.81) | 1.34 (0.28, 6.41) | 2.16 (0.45, 10.28) | 0.69 (0.13, 3.52) |
| Parents understanding the adolescent | ||||
| Yes | 1.00 | 1.00 | 1.00 | 1.00 |
| No | 0.80 (0.23, 2.99) | 0.85 (0.25, 2.93) | 1.26 (0.37, 4.34) | 1.27 (0.37, 4.47) |
| Parents treating their adolescent fairly | ||||
| Yes | 1.00 | 1.00 | 1.00 | 1.00 |
| No | 1.42 (0.35, 5.80) | 1.52 (0.39, 5.81) | 1.87 (0.49, 7.16) | 4.52 (1.17, 17.46) |
| Variables |
Preventable lifestyle risk factors1 |
|||
|---|---|---|---|---|
| One | Two | Three | Four or more | |
| Working status of fathers | ||||
| White-collar job | 1.00 | 1.00 | 1.00 | 1.00 |
| Blue-collar job | 1.47 (0.43, 5.07) | 1.08 (0.33, 3.48) | 1.48 (0.46, 4.81) | 3.57 (1.07, 11.92) |
| Parents treating their adolescent fairly | ||||
| Yes | 1.00 | 1.00 | 1.00 | 1.00 |
| No | 1.48 (0.36, 6.10) | 1.49 (0.39, 5.74) | 1.96 (0.51, 7.56) | 5.05 (1.29, 19.78) |
Figure & Data
References
Citations

- The relationship between food habits and physical activity and the IQ of primary school children
Alireza Khadem, Maryam Nadery, Sahar Noori, Rasool Ghaffarian-Ensaf, Abolghassem Djazayery, Ariyo Movahedi
Journal of Health, Population and Nutrition.2024;[Epub] CrossRef - Validation and Reliability of Lifestyle Instruments for Indonesian Adolescents with Hypertension Family History: A Rasch Model
Andra Kurnianto, Deni Kurniadi Sunjaya, Fedri Ruluwedrata Rinawan, Dany Hilmanto
Open Access Macedonian Journal of Medical Sciences.2023; 11(B): 109. CrossRef - Challenges of managing hypertension in Pakistan - a review
Adil Elahi, Arzina Aziz Ali, Aamir Hameed Khan, Zainab Samad, Hunaina Shahab, Namra Aziz, Aysha Almas
Clinical Hypertension.2023;[Epub] CrossRef - School Health Education Program in Pakistan (SHEPP): findings from a feasibility trial in pre-adolescent school children from a lower middle-income country
Aysha Almas, Romaina Iqbal, Abdul Ghani, Zainab Samad, Sania Sabir, Khawar Kazmi
Pilot and Feasibility Studies.2023;[Epub] CrossRef - Cardiovascular diseases preventive policy‐making process in Iran: A framework‐based policy analysis
Rahim Khodayari‐Zarnaq, Gisoo Alizadeh
World Medical & Health Policy.2022; 14(4): 679. CrossRef - Co-occurrence of non-communicable disease risk factors and its determinants among school-going adolescents of Kathmandu Metropolitan City
Kalpana Tandon, Nabin Adhikari, Bikram Adhikari, Pranil Man Singh Pradhan, Jianhong Zhou
PLOS ONE.2022; 17(8): e0272266. CrossRef - Batroxobin inhibits astrocyte activation following nigrostriatal pathway injury
Zhuo Zhang, Xue Bao, Dan Li
Neural Regeneration Research.2021; 16(4): 721. CrossRef - Lifestyle risk factors, non-communicable diseases and labour force participation in South Africa
Nozuko Lawana, Frederik Booysen, Asrat Tsegaye, Forget Mingiri Kapingura, Charles Hongoro
Development Southern Africa.2020; 37(3): 446. CrossRef - School health education program in Pakistan (SHEPP)—a threefold health education feasibility trial in schoolchildren from a lower-middle-income country
Aysha Almas, Romaina Iqbal, Sania Sabir, Abdul Ghani, Khawar Kazmi
Pilot and Feasibility Studies.2020;[Epub] CrossRef - Noncommunicable Disease Risk Factors Among Adolescent Boys and Girls in Bangladesh: Evidence From a National Survey
Nushrat Jahan Urmy, Md. Mokbul Hossain, Abu Ahmed Shamim, Md. Showkat Ali Khan, Abu Abdullah Mohammad Hanif, Mehedi Hasan, Fahmida Akter, Dipak Kumar Mitra, Moyazzam Hossaine, Mohammad Aman Ullah, Samir Kanti Sarker, SM Mustafizur Rahman, Md. Mofijul Isla
Osong Public Health and Research Perspectives.2020; 11(6): 351. CrossRef - Clustering patterns of behavioural risk factors for cardiovascular diseases in Bangladeshi adolescents: A population-based study
Asaduzzaman Khan, Riaz Uddin, Sheikh Mohammed Shariful Islam
Health Policy and Technology.2019; 8(4): 386. CrossRef - Evaluation of some diet habit and physical activity in adolescents in Tehran (2011)
B. Hossein Rashidi, H. Malek Afzali, F. Haghollahi, G. Ardalan, ME. Motlagh, H. Kazemi Jaliseh
The Journal of Qazvin University of Medical Sciences .2018; 22(1): 23. CrossRef - The Relationship of Social Capital with Lifestyle Among Adolescents: A Cross-Sectional Descriptive-Analytic Study
Bahare Zarei, Seyyed Abolfazl Vagharseyyedin
Modern Care Journal.2017;[Epub] CrossRef - Prevalence of Noncommunicable Diseases’ Risk Factors Among Secondary School Students in Eastern Iran in 2013
Elaheh Yari, Amir Tiyuri, Davood Beheshti, Hooriyeh Khodabakhshi, Gholamreza Sharifzadeh
International Journal of School Health.2016;[Epub] CrossRef - The Risk Factors of Child Lead Poisoning in China: A Meta-Analysis
You Li, Jian Qin, Xiao Wei, Chunhong Li, Jian Wang, Meiyu Jiang, Xue Liang, Tianlong Xia, Zhiyong Zhang
International Journal of Environmental Research and Public Health.2016; 13(3): 296. CrossRef - Protective effects of batroxobin on a nigrostriatal pathway injury in mice
Dan Li, Lei Tong, Hitoshi Kawano, Nan Liu, Lu Liu, Hong-Peng Li
Brain Research Bulletin.2016; 127: 195. CrossRef - Oral health and the provision of care to panjabi patients in the UK
Affifa Farrukh, Saad Sayeed, John Mayberry
Dental Update.2014; 41(7): 629. CrossRef
 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


