Mental Exercises for Cognitive Function: Clinical Evidence
Article information
Abstract
The purpose of this study was to examine the beneficial effects of a new cognitive intervention program designed for the care and prevention of dementia, namely Learning Therapy. The training program used systematized basic problems in arithmetic and Japanese language as training tasks. In study 1, 16 individuals in the experimental group and 16 in the control group were recruited from a nursing home. In both groups, all individuals were clinically diagnosed with senile dementia of the Alzheimer type. In study 2, we performed a single-blind, randomized controlled trial in our cognitive intervention program of 124 community-dwelling seniors. In both studies, the daily training program using reading and arithmetic tasks was carried out approximately 5 days a week, for 15 to 20 minutes a day in the intervention groups. Neuropsychological measures were determined simultaneously in the groups both prior to and after six months of the intervention. The results of our investigations indicate that our cognitive intervention using reading and arithmetic problems demonstrated a transfer effect and they provide convincing evidence that cognitive training maintains and improves the cognitive functions of dementia patients and healthy seniors.
INTRODUCTION
In Japan, the percent of the population of elderly people age 65 and over was 23.1% in 2010, an unprecedentedly high percentage, making Japan the world's first super-aging society. This super-aging environment necessitates the formation of a society in which all individuals can play an active role, even as they grow older. Ideally, it should be a society in which people can share their wisdom and knowledge, regardless of their age or gender, in order to maintain and improve the quality of life of all people and to maintain a healthy society.
Generally, an individual's quality of life increases with age; however, events like retirement can trigger a loss in one's sense of purpose in life and a feeling of disconnection from society, in turn lessening the quality of life. However, we believe that quality of life can be improved to one's last moments if the following four factors are given due consideration and if a social system dedicates its resources to achieving them for its population: cognitive stimulation, regular exercise, balanced nutrition, and a relationship with society.
To support the establishment of a social system that aims to realize these goals, we have been developing cognitive intervention programs to promote healthy, long lives so that individuals can continue to be intellectually stimulated, find their places as integral members of society, and maintain and improve their quality of life and mental and physical health.
Cognitive training is receiving increasing interest as a solution to age-related cognitive decline. Although the general public's interest in cognitive training, or mental exercises, is increasing, the generalizing or transfer effect of such training remains unclear. With regard to the changes in cognitive functions aging induces, it is important to note that while cognitive functions related to semantic knowledge do not decline with age, all cognitive functions are dependent on the prefrontal cortex, particularly the executive function, which declines linearly with age [1,2]. We previously demonstrated that cognitive intervention programs using intensive adoptive training of working memory [3,4] induce a plastic change in the brain structures of healthy young subjects in addition to improving their non-trained cognitive functions (transfer effects). Training which uses cognitive tasks, including working memory tasks, has been shown to improve performance on trained tasks as well as some untrained transfer tasks related to memory, intelligence, and response inhibition (for a review, [5]). Also, while the lateral prefrontal and parietal regions play a key role in working memory [6], studies demonstrated altered patterns of brain activity during untrained cognitive tasks, altered density of cortical dopamine D1 receptors, and altered white matter integrity after training on some working memory (WM) tasks associated with the prefrontal and parietal regions (for a review, [7]).
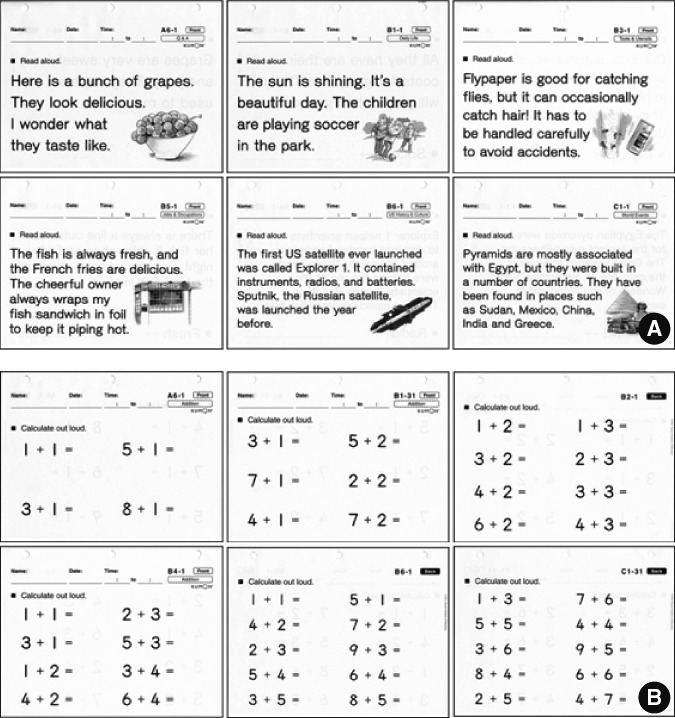
The purpose of this study was to examine the beneficial effects of Learning Therapy, a new cognitive intervention program designed for the care [8] and prevention of dementia [9]. The concepts of Learning Therapy are derived from our working memory training program, the tasks of which include systematized basic problems in arithmetic and Japanese language (Figure 1). The task of reading aloud is accomplished with a combination of several cognitive processes, for example, recognition of visually presented words, conversion of these graphic representations to phonological representations, analysis of the word meanings, and control of pronunciation. Solving arithmetic problems is also a task that cannot be accomplished without many cognitive processes, for example, recognition of visually presented numbers, performance of arithmetic operations, and control of hand movement. Both tasks are known to activate various brain areas including the prefrontal cortex of the bilateral hemispheres [10,11], in addition to other brain areas, and both clearly require working memory. Also, both tasks are simple and easy, so even people with senile dementia are able to understand, perform, and continue doing the tasks prepared in our program.
METHODS
Study 1
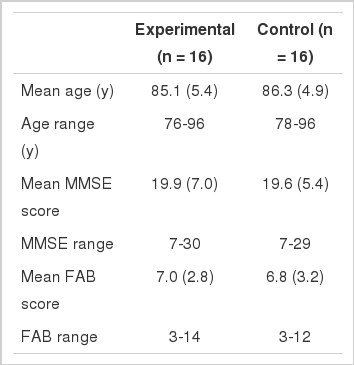
Sixteen individuals in the experimental group and 16 in the control group were recruited from a nursing home. Subjects were randomly assigned to these two groups. All of the individuals in both groups had a clinical diagnosis of senile dementia of the Alzheimer type [8]. None of the participants showed abnormalities such as tumors, cerebral bleeding, cerebral infarction, or pathological brain atrophy on an X-ray computed tomography examination. The baseline clinical and neuropsychological characteristics of the experimental and control participants are summarized in Table 1.
Study 2
We performed a single-blind, randomized controlled trial on our cognitive intervention program in community-dwelling seniors living in the same local community in Sendai, Japan [9]. In the first phase of the survey, we sent out information regarding the present study to all district residents ages 70 and over (total 3136; 1301 men, and 1853 women). We invited all these individuals to participate in a comprehensive geriatric assessment which included an assessment of medical and dental statuses, physical functions, and cognitive functions. We distributed leaflets describing the purpose and plans for this study to 962 individuals from which 269 applied for the study. The inclusion criteria were a Mini-Mental State Examination (MMSE) [12] score greater than 23 and a Geriatric Depression Scale score less than 15. Applicants who had a history of cerebrovascular diseases, who were active in another cognitive-related training program, and/or who were unavailable during the study period were excluded. In the end, 124 participants satisfying the inclusion and exclusion criteria were allocated into either the experimental group (n=62) or the control group (n=62) by random drawing using a computer.
In both studies, the daily training program using reading and arithmetic tasks was carried out in the intervention groups approximately 5 days a week, 15 to 20 minutes a day for six months. We prepared a wide range of materials (Figure 1).
In the first study, the lowest level arithmetic task was counting practice and the highest level was three-digit division. For the Japanese language tasks, the lowest level was reading and writing single syllables and the highest level was reading fairy tales aloud. The participants came to the learning center either on summons by the staff or by their own initiative every day from Monday to Saturday. Task worksheets of each task were prepared for each participant, each day, and participants would complete two to five of these worksheets daily. The participants' work was assessed by the Learning Center's staff and any mistakes were corrected by the participants. If the participants could not solve a problem by themselves, the staff members stationed between desks provided sufficient advice for them to be able to solve the problems. The study period ended when the participants completed each of the problems correctly.
In the second study, the lowest level of arithmetic-task difficulty was single-digit addition and the highest was three-digit division. For the Japanese language task, the lowest level of difficulty was reading and writing simple sentences and the highest level was reading fairy tales aloud. Prior to the training program, the appropriate degree of difficulty and workload for each subject was assessed by a diagnostic test, so that participants could continue to perform the learning tasks with ease. The participants in the experimental group were asked to go to classes in two elementary schools once a week. At the schools, five task worksheets of each task were prepared for each participant and the participants' work was assessed by the Learning Center's staff. Any mistakes were corrected by the participants. The study period ended when the participants completed each of the problems correctly.
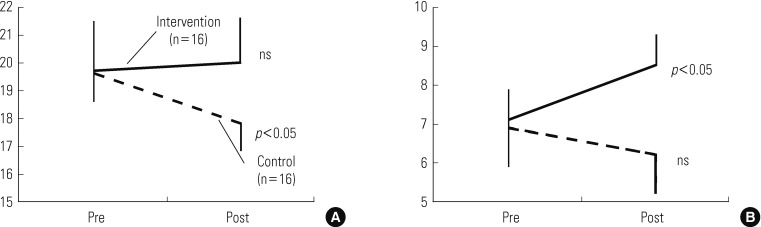
Neuropsychological measures were determined simultaneously in both the intervention and control groups prior to and six months after the intervention (post-test) by a MMSE [12], and Frontal Assessment Battery at bedside (FAB) [13]; therefore, the time span between the pre- and post-tests was six months. As for the second study, the Digit Symbol Substitution Test (DST) of the WAIS-R [14] was performed in addition to the MMSE and FAB. The neuropsychological characteristics of both groups were compared using an independent sample t-test at baseline and during follow up. A further analysis comparing baseline and follow-up scores separately for the learning and control groups was performed with a paired t-test. Statistical significance was set at p<0.05 for all of the comparisons.
RESULTS
Study1
The scores of the neuropsychological characteristics at the baseline and follow up are summarized in Figure 2. In the learning group, the FAB score showed a statistically significant (p<0.05) increase after the training had taken place. However, the MMSE score did not show any significant changes. In the control group, the MMSE score showed a statistically significant (p<0.05) decrease from baseline to follow up. Nevertheless, the FAB score did not show any significant changes. During the follow up, the MMSE and the FAB scores of the learning group were statistically significantly (p<0.05) higher than those of the control group. There was no relationship between the magnitude of change seen in the neuropsychological characteristics and initial scores on the MMSE or FAB in the learning group.
Study 2
The scores of the neuropsychological characteristics at baseline and follow up are summarized in Figure 3. In the experimental group, the FAB and DST scores showed a statistically significant (p<0.001) increase after the intervention. However, the MMSE score showed no significant changes. In the control group, the FAB and DST scores showed no significant change. The MMSE score decreased from the pre- to post-test; however, the decrease did not reach a statistically significant level (p=0.055). In the post-test, the MMSE score of the experimental group was higher than that of the control group. However, the difference did not reach a statistically significant level (p=0.05). The DST score showed no significant difference between the experimental and control groups in the post-test.
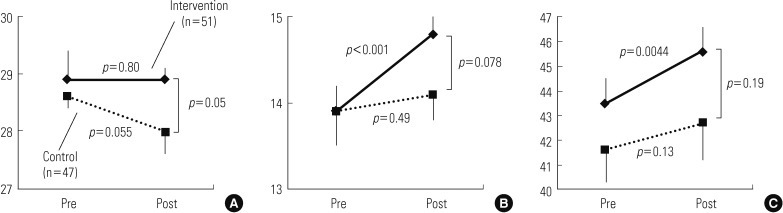
Changes in neuropsychological characteristics for study 2. All the subjects were community dwelling elderly people. (A) Mini-Mental Status Examination score, (B) Frontal Assessment Battery at bedside score, and (C) Digit Symbol Substitution Test of the WAIS-R score. Error bars indicate the standard error of the mean.
DISCUSSION
The results of these studies were convincing evidence that a daily training program involving reading and arithmetic problems has an immediate and beneficial effect on mental processing speed (as measured by DST) and executive function (as measured by FAB). These effects are also not directly tied to the intervention. Participants maintained their improvements six months after the training program.
Our intervention program is based on a system of daily training. Other previous cognitive intervention studies used a relatively short intervention period compared with the present study and also found long-term beneficial effects on cognitive functions. Previous intervention studies by the ACTIVE trial [15] and Mahncke et al. [16] showed improvements in cognitive functions. The results of many clinical studies of humans and experimental studies of animals support the idea that continuous stimulation of the brain causes changes in the brain. There is no doubt that the brain has a lifelong capacity for plasticity, which is why inducing changes in brain networks with a daily intervention program is a reasonable method of stimulation. The sustained beneficial effects on the non-directly targeted cognitive functions found in this study and in other intervention studies [16] may be related to the same mechanism. Although we found sustained high cognitive activity six months after the intervention, further observation to estimate the longevity of the improvement seen in the intervention is necessary.
In general, aging is viewed negatively as the loss of something that people have in their youth or as a form of regression. As a result, society has formed a false image that aging is something like an illness, that it is ugly, and that young people are superior to the elderly in many respects. However, we consider aging to mean that people can grow and become wiser as they reach the later stages of life. We call this concept "smart aging" and advocate it as a healthy outlook for society to adopt.
Events like retirement can trigger a loss of one's sense of purpose in life and initiate a feeling of disconnection from society as one grows in age, which in turn lessens the quality of life. However, we believe that the quality of life can be improved to one's last moments if the following four factors are given due consideration and if a social system dedicates its resources to achieving them for its population: cognitive stimulation, regular exercise, balanced nutrition, and a relationship with society.
Here, we proposed a smart, but inexpensive system for cognitive stimulation. The results of our investigations demonstrate that reading and solving arithmetic problems in our cognitive intervention program indeed has a transfer effect, and they are convincing evidence that cognitive training maintains and improves the cognitive functions of dementia patients and healthy seniors.
ACKNOWLEDGEMENTS
I thank professor Ichiro Tsuji at the Graduate School of Medicine, Tohoku University, for his suggestions and collaboration during the experimental setup and design. I also thank all the staff members involved in the Tsurugaya Project, and Kumon Learning Center for their technical support of the cognitive measures and intervention. This study was supported by RISTEX, JST, and a collaborative study between Tohoku University and Sendai City (Gakuto collaboration research project).
Notes
The author has no conflicts of interest with the material presented in this paper.