Smoking Is Associated With Abdominal Obesity, Not Overall Obesity, in Men With Type 2 Diabetes
Article information
Abstract
Objectives
Abdominal obesity increases mortality and morbidity from cardiovascular disease and there is a possibility that smoking effects obesity. However, previous studies concerning the effects of smoking on obesity are inconsistent. The objective of this study was to examine whether smoking is positively related to abdominal obesity in men with type 2 diabetes.
Methods
Subjects consisted of 2197 type 2 diabetic patients who visited Huh's Diabetes Center from 2003 to 2009. Indices of abdominal obesity were defined as visceral fat thickness (VFT) measured by ultrasonography and waist circumference (WC). Overall obesity was defined as body mass index (BMI).
Results
Statistically significant differences in WC and VFT by smoking status were identified. However, there was no statistical difference in BMI according to smoking status. Means of WC and VFT were not significantly higher in heavy smokers and lower in mild smokers. Compared to nonsmokers, the BMI confounder adjusted odds ratio and 95% confidence interval for VFT in ex-smokers and current-smokers were 1.70 (1.21 to 2.39) and 1.86 (1.27 to 2.73), respectively.
Conclusions
Smoking status was positively associated with abdominal obesity in type 2 diabetic patients.
INTRODUCTION
With the obesity epidemic on the rise, research on obesity has intensified. A previous study showed, that compared to overall obesity, abdominal obesity increases the risk of metabolic diseases, such as cardiovascular disease (CVD), diabetes, hypertension, dyslipidemia, and insulin resistance [1]. In addition, it has been reported that even with a body mass index (BMI) in the normal range, a significantly higher waist circumference (WC) or waist to hip ratio (WHR) increases the possibility of complications and obesity-related diseases [2]. Despite having low BMI levels compared to Western populations, the Korean population is at risk for type 2 diabetes due to relatively high central obesity and hypertension [3]. Recently, the rate of obesity has increased in Korea. According to the Korea National Health and Nutrition Examination Survey, the overweight and obese Korean population over 20 years of age has prevalence rates of 36.7% for men and 27.4% for women [4].
Smoking prevention and smoking cessation play important roles in improving overall health, however, many teenagers and women start smoking mistakenly believing that it will help them lose weight. In fact, it has been reported that 60% of female smokers do so to maintain or lose weight [5]. The smoking prevalence of Korean men over 30 years of age decreased from 72.37% in 1992 to 52.43% in 2006 [6], but Korea has had a relatively high level of tobacco use among males worldwide.
The association between smoking and obesity is as important health issue because both smoking and increased body weight are independent risk factor for CVD. However, the effect on obesity according to smoking status or smoking amount is particularly controversial. According to data from the World Health Organization MONICA project (monitoring trends and determinants in cardiovascular disease), men and women who smoked generally had lower BMI than never smokers [7]. Several previous studies have been reported that among smokers a U-shaped relationship between the number of cigarettes smoked and body weight [8,9]. In contrast, some studies claim that correlations between smoking and the distribution of fat are irrelevant [10]. The association of smoking and visceral fat among type 2 diabetic patients has not been extensively researched. Such studies had relatively small sample sizes and inconsistent findings. Therefore, the objective of this study was to examine whether smoking is positively related to abdominal obesity as measured by visceral fat thickness (VFT) and WC in type 2 diabetic patients.
METHODS
Study Subjects
We examined diabetes patients (n=9531) from January 2003 to June 2009 at Huh's Diabetes Center, a primary health care facility in Seoul, Korea. Our analysis only included men who had a smoking habit (n=3337) because of a low smoking prevalence among women. Patient exclusion criteria included 1) diagnosis with type 1 diabetes (identified with a fasting C-peptide level <0.5 ng/mL and with either a diagnosis of diabetes before the age of 30 years or a history of diabetic ketoacidosis), 2) absence of VFT and WC measurements, 3) a history of CVD, and 4) diagnosis with any type of cancer. A total of 2197 patients with type 2 diabetes mellitus were eventually enrolled in the study. The Yonsei Medical University College of Medicine ethics committee approved the study protocol.
Clinical and Biochemical Assessment
Patients were diagnosed with diabetes based on the American Diabetes Association criteria. For all participating patients, the study used data collected during the patient's first visit. A single trained study staff member collected all the data, including anthropometric indices. Participants were interviewed through a structured questionnaire in order to collect lifestyle data (such as smoking habits, alcohol consumption, and exercise). They were asked to describe their smoking habit (never-smoker, ex-smoker, or current smoker), alcohol consumption (nondrinker or drinker, regardless of the amount of alcohol), exercise routine (exercising or not exercising), as well as other demographic characteristics such as age, gender, and diabetes duration, and medication. The amount and duration of smoking among current smokers was also recorded. Smoking amount was categorized as 1 to 10, 11 to 20, or ≥21. Weight and height were measured for all subjects while they were wearing light clothing and not wearing shoes. Multiple measures of obesity indices were recorded and calculated, including BMI, WC, and VFT. BMI was calculated by dividing weight in kilograms by the square of height in meters. WC was measured midway between the lower rib margin and iliac crest. VFT was measured by high-resolution ultrasonography [11-13] and defined as the distance between the anterior wall of the aorta and the internal face of the rectoabdominal muscle perpendicular to the aorta. Transverse scanning was performed using a 3.5 MHz probe to measure VFT at 1 cm above the umbilicus. Blood pressure was measured using a standard mercury sphygmomanometer after the subjects had been seated for at least 10 minutes. Blood was collected after more than 10 hours of fasting, and fasting blood glucose, glycosylated hemoglobin, total cholesterol, high-density lipoprotein (HDL), triglycerides, and low-density lipoprotein were measured.
Statistical Analysis
The results are presented as mean±SD or number (%).The partial correlation coefficient was used to describe the association between VFT and other continuous variables of interest, after controlling for the effect of age. Differences in general characteristics between never-smoker, ex-smoker, and current smoker groups were compared using one-way ANOVA (for continuous variables) or the chi-square test (for categorical variables). The crude or adjusted mean VFT values were categorized according to smoking status and smoking amount. Analyses were adjusted for variables such as age, duration of diabetes, alcohol consumption, exercise, and BMI. We additionally adjusted for the use of any diabetes medication (medication; no medication) and for hemoglobin A1c (HbA1c) levels, in order to control for the effects of diabetes therapy or glycemic management.
Moreover, we analyzed the subgroup of patients (n=453) with available smoking amount data. High VFT was defined as a VFT of ≥47.6 mm [13]. The nonsmoker group included never-smokers and ex-smokers. A multivariate logistic regression model was used to test the independent association between smoking and high VFT, adjusting for potential confounding variables such as age, diabetes duration, alcohol consumption, exercise, and BMI. All analyses were conducted using the SAS version 9.1 (SAS Inc., Cary, NC, USA). All statistical tests were two-sided, and statistical significance was accepted for p<0.05.
RESULTS
Our results showed that among the type 2 diabetic patients participating in the study, approximately 50% were ex-smokers and 33.5% were current smokers. The mean age of participants was 55.5 years (age range, 28 to 87 years). The VFT mean values were 47.1, 49.2, and 49.8 mm for never-, ex-, and current smokers, respectively (Table 1). Current smokers had higher HbA1c and lipid profile levels, compared to never-smokers and ex-smokers. Drugs used in the treatment of type 2 diabetes include sulfonylurea, biguanide, acarbose, glitazone (TZDs), insulin, and statin. The percentage of type 2 diabetic patients who were on sulfonylurea, biguanide, acarbose, TZDs, insulin, and other hypoglycemic drugs were 51.7%, 36.7%, 12.2%, 9.7%, 10.7%, and 0.4%, respectively. The prevalence of any diabetes medication was different among the 3 groups (data not shown).
VFT, which was determined using ultrasonography, was best correlated with WC (r=0.667, p<0.000), followed by BMI (r=0.627, p<0.000) (Table 2). The correlation between VFT and clinical laboratory values of HDL, cholesterol, triglycerides, blood pressure, and insulin was also significant.
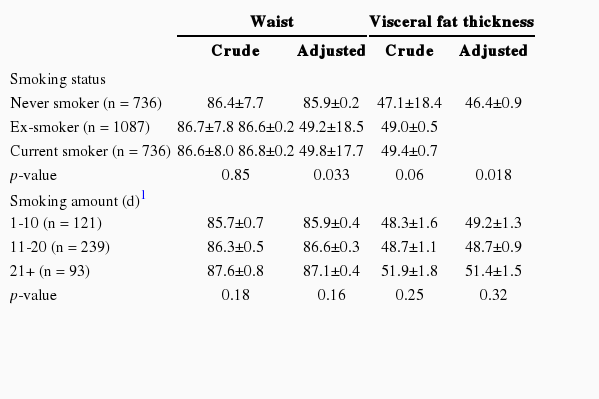
The mean VFT values are shown according to smoking status and amount in Table 3. Statistically significant differences in WC values were found between current smokers, ex-smokers, and never-smokers after adjusting for age, duration of diabetes, alcohol consumption, regular exercise, and BMI. Among current smokers, the number of cigarettes smoked per day also positively correlated with the abdominal obesity indicators WC and VFT, although the correlation was not statistically significant.
The association between smoking status and abdominal obesity, after adjusting for diabetes medication and HbA1c levels, was slightly attenuated but remained significant (Figure 1). Current smokers had the highest WC and VFT values, followed by ex-smokers, and then never-smokers. The BMI values, however, were not significantly different between current, never-, and ex-smokers.
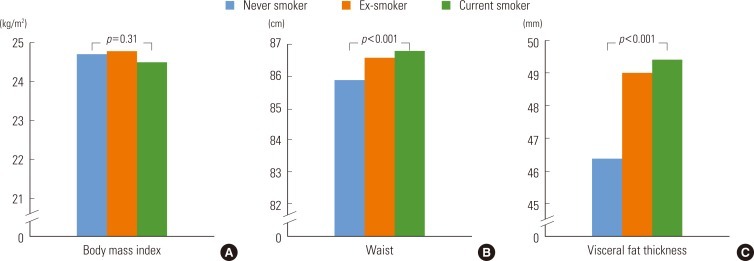
The means of body mass index (A), waist (B), and visceral fat thickness (C) according to smoking status. Body mass index was adjusted for age, alcohol drinking, regular exercise, duration of diabetes, medication of diabetes, and hemoglobin A1C. Waist and visceral fat thickness were adjusted for age, body mass index, alcohol drinking, regular exercise, duration of diabetes, medication of diabetes, and hemoglobin A1c.
This study examined the independent risk of high VFT levels in relation to smoking status, by using multivariate logistic regression analysis (Figure 2). The results showed that smoking significantly increased the risk of abdominal obesity, after adjusting for possible confounders such as BMI. We observed a linear increase in the odds ratio (OR) of abdominal obesity with increasing levels of both smoking status and amount. Patients who currently smoked more than 20 cigarettes per day had an adjusted OR of 1.93 (95% confidence interval, 1.16 to 3.21) compared to never-smokers.
DISCUSSION
Our data indicates that type 2 diabetes patients who smoke have significantly higher central adiposity, according to VFT and WC values, than non-smokers. Heavy smokers particularly have higher central adiposity than light smokers. When further adjustment was made for diabetes medication and HbA1c levels, this association between smoking status and abdominal obesity, although slightly attenuated, remained significant. Heavy smokers had higher abdominal obesity OR values than light smokers, even after adjusting for BMI. Among current smokers, heavy smokers showed significantly higher VFT values. For instance, participants who smoked more than 20 cigarettes per day showed higher VFT values than those who smoked less than 10 cigarettes per day. However, no dose-response relationship between the number of cigarettes smoked and abdominal obesity was observed.
Our study's consistent results demonstrate that current smokers have higher abdominal obesity than never- and ex-smokers. Shimokata et al. [14] previously reported positive association between smoking and abdominal obesity, regardless of whether BMI values were low. The WHR actually increased in patients who started smoking, despite their weight loss. However, according to data from the Scottish Health Survey, a decrease was observed in weight and BMI values of smokers compared to non-smokers [15]. Additionally, a recent study conducted in Turkey states that smoking inhibits visceral fat accumulation in women [16]. The study found that current smokers showed 26% less fat mass and 30% less visceral adipose tissue than non-smokers, although the differences were statistically insignificant for the men's data. Simon et al. [17] reported higher WHR for current smokers than subjects who quit smoking. Other studies claim that there is no significant association between smoking and fat distribution. Seidell et al. [10] state that smoking does not cause BMI increase, but that heavy smoking leads to higher WC. Moreover, one study claims that cigarette smoking is not related to a specific distribution pattern of body fat. Thus, studies report inconsistent conclusions regarding the relationship between obesity and smoking.
Some studies that claim an association between smoking and abdominal obesity have shown higher abdominal obesity levels in smokers compared to non-smokers; however, the mechanisms responsible for those results have not been proven conclusively. Previous studies have also shown an association between smoking and hormonal changes. Smokers of 2.4 mg Federal Trade Commission nicotine cigarettes have increased plasma beta-endorphin and cortisol levels, compared to non-smokers [18]. Significantly, increased cortisol levels lead to increased insulin resistance, which is associated with abdominal fat and diabetes [19]. Many epidemiological studies have demonstrated increased levels of testosterone, free testosterone, and androgen in men smokers [20-22]. In one such study, smokers had higher mean plasma estradiol levels compared to non-smokers [23,24]. Exposure to androgens is linked to abdominal fat in premenopausal women [25]. However, a negative correlation links testosterone and abdominal fat distribution in men [26]. Therefore, the relationship between smoking, body fat distribution, and sex hormones remains unclear and may be further complicated by confounding factors such as alcohol consumption and stress levels.
Nicotine consumption was previously shown to temporarily enhance metabolism during resting as well as during light physical activity. However, there has been no evidence that nicotine enhances human body energy expenditure in the long term. Moreover, some studies have demonstrated that smokers and non-smokers have similar basal metabolic rates. On the other hand, it has also been reported that smokers tend to weigh less than non-smokers and that smokers gain weight after quitting. Several studies have demonstrated that body weight seems to be highest in ex-smokers, lowest in current smokers, and intermediate in never-smokers [27-29]. Nevertheless, these results are controversial (not all results follow this pattern), and the biological mechanism involved has not been established. Additionally, most studies have investigated the association between smoking and obesity in healthy subjects. This association mechanism may be different in diabetes patients. Therefore, carefully designed follow-up studies of diabetic patients are required to consolidate the correlations documented in the present study.
Nevertheless, this study has some limitations. First, we only used baseline measurements obtained during each individual's first visit, for characterization. We did not account for possible changes in smoking status or other lifestyle behaviors during follow-up; there is the possibility that diabetic patients' WC, VFT, and glycemic control-related living habits had already changed by the time of the follow-up. Second, due to the cross-sectional design, this study could not elucidate mechanisms or determine the direction of causality. Third, although we adjusted for several known potential confounders, we cannot completely rule out the possibility of residual confounding such as stress and secondhand smoke. Stress-dependent cortisol values, in particular, have been strongly associated with abdominal obesity [30]. Finally, the contribution of fat mass distribution may vary among different populations. Accordingly, our results may differ from those of studies using data obtained from women or other ethnic group participants. Therefore, further investigation, using a longitudinal study design, is needed to determine whether smoking causes abdominal obesity in general.
This study also has several strengths. This study was performed using a relatively large cohort of type 2 diabetes performed in one institute. Additionally, both WC and VFT were measured using ultrasonography and were used as indices of abdominal obesity. Moreover, all data, including anthropometric indices, were obtained by a single trained study staff member. VFT is a simple noninvasive alternative to computed tomography and a reliable index for visceral fat measurement and identification of diabetic patients [13]. Furthermore, we assessed the association of abdominal obesity with not only smoking status but also smoking amount. Previous studies have lacked such detailed and accurate measurements of smoking amount. This study is important because it confirms a positive relationship between high smoking amount and abdominal obesity, where both are common risk factors in patients with type 2 diabetes.
In conclusion, our study found that smoking status was closely related to abdominal obesity. Further research is needed to elucidate the association of smoking status and/or smoking patterns and abdominal obesity. The findings of this study should be cross-validated to different populations; hence, further large-scale prospective studies are needed in type 2 diabetic patients. Re-evaluation of our conclusions should be continued since smoking may influence abdominal obesity, leading to other unfavorable health outcomes.
ACKNOWLEDGEMENTS
This study was supported by a grant (10526) from the Seoul City R&BD program.
Notes
The authors have no conflicts of interest with the material presented in this paper.