Mean Sojourn Time of Preclinical Gastric Cancer in Korean Men: A Retrospective Observational Study
Article information
Abstract
Objectives:
This retrospective cohort study aimed to estimate the mean sojourn time (MST) of preclinical gastric cancer in Korean men.
Methods:
The subjects consisted of voluntary male screenees aged 40 to 69 years who underwent subsequent screening gastroscopies after testing negative at a baseline screening performed between January 2007 and December 2011. A new case was defined if gastric cancer cells were present in the biopsy specimens obtained from gastroscopy. The follow-up period was calculated as the number of person-years between the date of baseline screening gastroscopy and positive findings at a subsequent screening. The MST was calculated using transition rates of gastric cancer to determine the best screening interval.
Results:
Of the 171 979 voluntary male screenees, 61 688 (36%) underwent subsequent screening gastroscopies between January 2007 and December 2011. A total of 91 incident cases were found during 19 598 598 person-years of follow-up. The MST of gastric cancer was 2.37 years (95% confidence intervals, 1.92 to 2.96), and those aged 40 to 49 years had a shorter MST than those 50 to 69 years did.
Conclusions:
These findings support the 2-year interval of screening recommended by the nationwide gastric cancer screening program in Korea. Further studies for the age-specific MST among women are needed.
INTRODUCTION
The main strategy of population-based cancer control is a national mass screening program of the asymptomatic normal-risk population [1]. However, the estimation of sojourn time is needed to decide an optimal interval of next screening [2]. Sojourn time is defined as the duration of the preclinical detectable phase and is an unobservable quantity; therefore, mean sojourn time (MST) was estimated [3,4]. To estimate MST, several statistical models using interval cases have been developed [5]. Interval cases can be identified by merging collected data with a national cancer registry database; however, merging data is prohibited according to the privacy and confidentiality laws in Korea [6]. Recently, Brenner et al. [7] estimated the MST of preclinical colorectal cancer using the annual rate of screening participation without identifying interval cases.
Gastric cancer is the second leading type of incident cancer in Korea [8], but the MST of preclinical gastric cancer in Korea has never been estimated to our knowledge. Therefore, this retrospective follow-up study aims to estimate the MST for gastric cancer screening in normal-risk Korean men.
METHODS
Study Population
The source population consisted of voluntarily attendees from cancer screening programs provided by the Korea Medical Institute (KMI). This non-profit foundation, established in 1985, specializes in comprehensive health examination services and comprises seven of the medical examination clinics in Korea [9]. In this program, gastroscopy is the primary modality for the initial and follow-up screening of gastric cancer.
The selection criteria for constructing the baseline cohort were voluntary screenee Korean men aged 40 to 69 years who underwent subsequent screening gastroscopies after receiving initial negative results during the first (baseline) screening between January 2007 and December 2011. These data were used to calculate the incidence rate (INC) of gastric cancer. The age at screening was determined by the date of conducting the baseline screening gastroscopy from January 2007. Every participant had to complete the structured questionnaire before undergoing screening. Those who reported a history of gastric cancer were excluded because their gastroscopy was a follow-up test, not screening test.
Detection of Gastric Cancer
When a gastroscopic finding suggested gastric cancer, the endoscopist obtained biopsy specimens that were then evaluated by gastrointestinal pathologists. A new case was defined if gastric cancer cells were confirmed in the biopsy specimens obtained from the gastroscopy [10].
All endoscopy reports, pathology reports, and questionnaires were retrospectively collected from the KMI databases. All screenees consented to gastroscopy and the use of their personal data for research. This study protocol was approved by the institutional review board of Jeju National University Hospital (no. 2013-05-023) and was registered in the Clinical Research Information Service System, Korea Centers for Disease Control and Prevention (no. KCT0000772) [11].
Statistical Analysis
To describe the basic characteristics of the study population, descriptive statistical parameters including number and column percentage were obtained after age stratification. The screenees were classified into age groups of 40 to 49, 50 to 59, and 60 to 69 years. The annual prevalence rate (PRE) per 100 000 screenees at the first (baseline) screening was calculated by dividing the number of biopsy-proven cases by the 5-year total number of screenees. For subjects who underwent subsequent screening gastroscopies after a negative gastroscopy finding at the first screening, follow-up periods were calculated as the number of the months between the date of the first screening gastroscopy and positive findings on subsequent screenings. If the last screening result was normal, the date of thais test was considered the end of follow-up for that subject. From this follow-up information, the annual INC per 100 000 person-years was calculated by dividing the number of new cases by the total number of years of follow-up. The 95% confidence intervals (CIs) for INCs are based on the Poisson distribution.
To estimate the MST of gastric cancer, the formula by Brenner et al. [7] was applied. The key assumption is that cancer prevalence among those who have not undergone a screening (non-participants), which cannot be observed directly, is the same as the observed prevalence among those who have undergone a screening (participants). Under this assumption, the equation of MST is MST=[PRE×(1-PAR)]/[INC+{PAR×LN(1-PRE)}]. In this equation, PRE indicates the annual prevalence of cancer among participants and non-participants, and annual INC represents the overall incidence of cancer in a population. Brenner et al. [7] denoted PAR as the annual rate of participation in screening; however, we defined PAR as the proportion of those who participated in a second screening among the subjects who had a negative gastroscopy at the first gastric cancer screening. The reason to modify the definition of PAR was that the follow-up in our study started after receiving a negative gastroscopy finding at the first screening, thus was only completed in subjects undergoing subsequent gastroscopies. In addition, the reciprocal of MST is the transition rate from preclinical (undiagnosed) to clinical (diagnosed) cancer. The upper and lower boundaries of MST were estimated based on the 95% CI of the INCs. All statistical tests were performed uusing STATA version 12 (StataCorp, College Station, TX, USA).
RESULTS
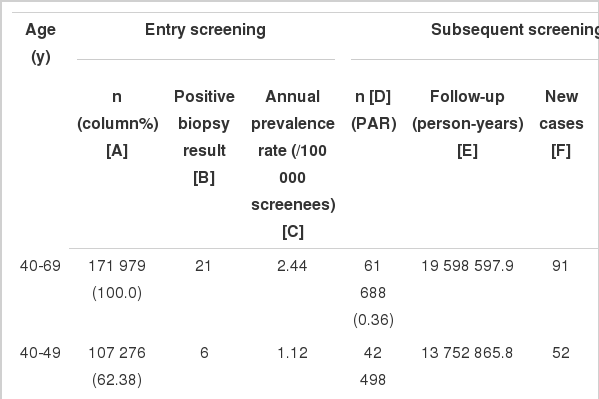
Figure 1 shows the overall process of cohort construction and follow-up. A total of 171 979 male screenees aged 40 to 69 years voluntarily participated in the KMI screening program for gastric cancer between January 2007 and December 2011. Twenty-one cases were detected at the entry screening, with the PRE of 2.44 per 100 000 screenees. Table 1 shows the distribution of PRE by age group.
Flowchart of the selection process and follow-up of the study participants from the Korea Medical Institute data collected between January 2007 and December 2011.
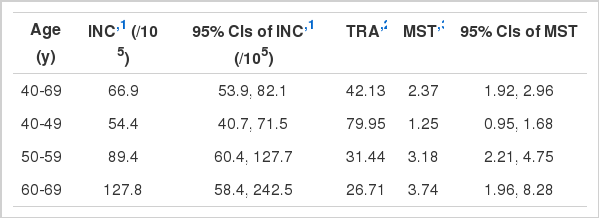
Among subjects with a negative gastroscopy at the baseline screening, 61 688 (36%) underwent subsequent screening endoscopies (PAR) totaling 19 598 598 person-years of follow-up. A total of 91 incident cases were found with an annual INC of 66.9 per 100 000 person-years (95% CI, 53.9 to 82.1). Using the numerical formula, the estimated MST of preclinical gastric cancer in Korean men was 2.37 years (95% CI, 1.92 to 2.96). Stratified with age groups, the 95% CIs of those aged 40 to 49 years did not overlap with those aged 50 to 59 and 60 to 69 years. Table 2 shows the distribution of the annual INC, the transition rate (TRA), and the estimated MST by age group.
DISCUSSION
The National Cancer Center in Korea recommends biennial screening with gastroscopy or upper gastrointestinal series in adults older than 40 years [12]. We found the overall estimated MST of gastric cancer to be 2.37 years in men aged 40 to 69 years supported the national guidelines of biennial screening. In addition, we found that those aged 40 to 49 years had a shorter MST than those aged 50 to 69 years did. This finding supports the rationale for the use of shorter intervals of screening in the younger population [13,14]. However, further studies are needed before detailed intervals by age groups are suggested especially since the estimated age-stratified MST in our study showed wider CIs due to a limited sample size.
MST can be estimated using several different methods if screening data is available [5], but data on the PRE at the first screen, cancer incidence in the absence of screening, and interval cancers are required [2,15]. Nowadays researchers in Korea cannot estimate MST using data on interval cancers because of legal restrictions [6]. In addition, the cancer incidence in the absence of screening can be obtained only from randomized clinical trials. However, conducting a randomized clinical trial for cancer screening in Korea is also impossible because of ethical reasons coinciding with the operation of the national cancer screening program [7]. Based on the hierarchy of evidence-based study designs, a longitudinal cohort study would be the next option to estimate MST. A longitudinal cohort study would allow for the estimation of the prevalent rate at baseline and the incident rate through subsequent screenings as well as PAR. Brenner et al. [7] estimated the MST of colorectal cancer using a national colonoscopy database and national estimates of colorectal cancer incidence in Germany that provided the prevalence, incidence, and PAR without having to identify interval cases. This formula was applied to the KMI screening gastroenteroscopy database in our study.
Using the formula by Brenner et al. [7] requires the acceptance of three assumptions. First, cancer prevalence among non-participants is accepted to be the same as the observed prevalence among participants. This assumption could be confirmed if cancer screening is conducted in asymptomatic healthy people. Second, it is assumed that the INC of targeted cancer among participants is constant over time; therefore, cancer detection by screening is also constant over time to allow for use of data from a single institute. Last, the TRA is assumed constant over time. We were also able to accept the last assumption because the TRA of a specific cancer does not depend on the screening process, rather on the biological growth of cancer cells.
Several limitations should be considered while considering the results of this study. The first issue is the applicability of the induced formula. Brenner et al. [7] used nationwide databases in the development of the formula to estimate MST, but an institutional database was used in our study. However, both studies follow a retrospective cohort design, so the required parameters were estimated directly. Additional studies are needed to evaluate the robustness and sensitivity of the formula across various settings. The second issue is the definition of INC. It differed between the study by Brenner et al. [7], which calculated the INC in their population, and that of this paper, which calculated the INC in subsequent screenees. Compared with the incidence definition by Brenner et al. [7], the incidence of this paper could be interpreted as the INC among participants (INCp). Therefore, our paper shifts the scope from nationwide to institution-wide; the incidence of this paper would be defined as the overall incidence of the study population. In addition, Brenner et al. [7], suggested a revised formula as INCp=-LN (1-PRE) where INCp is the incidence among participants, which should be constant over time. We found a difference between the estimated incidence among participants and the annual incidence estimated from our study population using the prevalence (Table 1). The last issue is the selection bias. Our study participants voluntarily participated in the screenings, so they did not represent all Korean men. However, our findings support the recommendation of a national cancer screening program in Korea. In addition, these might ascertain whether Brenner’s formula could calculate MST using limited information.
In conclusion, this study suggests that the estimated MST of gastric cancer in Korean men aged 40 to 69 years is about 2 years. This finding supports the 2-year interval that is already recommended by the national gastric cancer screening program in Korea. Further follow-up studies are required to investigate the MST by age group in women as well as the robustness of our analytic method in other settings. In particular, the MST for gastric cancer in women should be investigated using more subjects and over a longer period than that of the present study, especially considering the low incidence of gastric cancer in women.
ACKNOWLEDGEMENTS
This study was supported by a grant from the National R&D Program for Cancer Control, Ministry of Health and Welfare, Korea (no. 1320300). The authors would like to thank Professor Chung Mo Nam, Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea, for his help with the statistical analyses.
Notes
The authors have no conflicts of interest with the material presented in this paper.