Hormonal Replacement Therapy and the Risk of Lung Cancer in Women: An Adaptive Meta-analysis of Cohort Studies
Article information
Abstract
Objectives:
Approximately 10% to 15% of lung cancer cases occur in never-smokers. Hormonal factors have been suggested to lead to an elevated risk of lung cancer in women. This systematic review (SR) aimed to investigate the association between hormonal replacement therapy (HRT) and the risk of lung cancer in women using cohort studies.
Methods:
We first obtained previous SR articles on this topic. Based on these studies we made a list of refereed, cited, and related articles using the PubMed and Scopus databases. All cohort studies that evaluated the relative risk of HRT exposure on lung cancer occurrence in women were selected. Estimate of summary effect size (sES) with 95% confidence intervals (CIs) were calculated.
Results:
A total of 14 cohort studies were finally selected. A random effect model was applied due to heterogeneity (I-squared, 64.3%). The sES of the 14 articles evaluating the impact of HRT exposure on lung cancer occurrence in women indicated no statistically significant increase in lung cancer risk (sES, 0.99; 95% CI, 0.90 to 1.09).
Conclusions:
These results showed that HRT history had no effect on the risk of lung cancer in women, even though the sES of case-control studies described in previous SR articles indicated that HRT had a protective effect against lung cancer. It is necessary to conduct a pooled analysis of cohort studies.
INTRODUCTION
Lung cancer is the largest cause of cancer deaths among Koreans [1], and smoking is known to be the main cause of lung cancer [2,3]. However, 10% to 15% of total lung cancer patients have never smoked [4]. It has been argued that never-smokers’ lung cancer (NSLCa) should be recognized as a new disease [5] due to its unique epidemiological characteristics, including a high incidence in women and Asian individuals, as well as a higher frequency of adenocarcinomas [6,7].
Factors associated with NSLCa include passive smoking, occupational exposure, atmospheric pollution, past disease history, and genetic sensitivity [5,6]. However, the majority of these factors do not explain the epidemiological fact that NSLCa is more common in women. In particular, it has even been reported that passive smoking is unlikely to contribute to the incidence of NSLCa in Asian individuals [8]. As a result, the possibility of a relationship between lung cancer in women and estrogen has been debated, and more specifically, it has been proposed that oral contraception and hormone replacement therapy (HRT) may be associated with lung cancer [7,9-13].
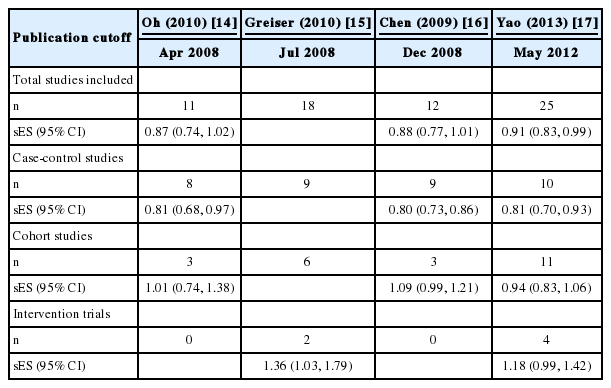
With the aim of investigating the association between the HRT history and the occurrence of lung cancer in women, we searched for systematic reviews (SRs) published up to September 2015, and found a total of four such studies (Table 1) [14-17]. The summary effect sizes (sES) with 95% confidence intervals (CIs) in case-control studies consistently reported a protective effect. In addition, Pesatori et al. [18] performed a pooled analysis of raw data from six case-control studies, and also reported a protective effect (sES, 0.77; 95% CI, 0.66 to 0.90), while consistent results were also confirmed in the case-control studies.
Conversely, the sES of cohort studies presented in Table 1 not only failed to show a consistent findings, but their findings were not statistically significant. Even considering the different endpoints of the literature searches, the four SRs show large differences in the number of cohort studies selected for each meta-analysis, and even show different relative risk (RR) and 95% CI values for the same studies in some instances (Table 2). Moreover, of the eleven cohort studies selected by Yao et al. [17], the papers by Adami et al. [19] and Persson et al. [20] were different follow-ups studies of the same cohort participants, and so one of these papers should have been excluded from the meta-analysis. Hence, the aim of the present study was to investigate whether HRT is a risk factor for lung cancer in women using an adaptive meta-analysis of cohort studies.
METHODS
Search and Selection of Relevant Literature
Since this study made use of four existing SR papers [14-17], a manually snowballing strategy was used to optimize the efficiency of the literature search [21-23]. Specifically, the literature search was based on the 12 cohort studies [19,20,24-33] used in the four SRs (Table 2), and for each of these studies, a list of the refereed articles as well as “Cited articles”, and “Similar (Related) articles”, as provided by PubMed (www.ncbi.nlm.nih.gov/pubmed) and Scopus (www.elsevier.com/Scpous), was acquired. September 2015 was the cutoff for publication. In order todetermine the final papers to include in the analysis, the following six exclusion criteria were applied: (1) laboratory studies (2) expert reviews (3) case-control studies (4) intervention trials (5) cohort studies containing no data about HRT and (6) cohort studies analyzing the same participants as another study included in the analysis.
Statistical Analysis
Two researchers confirmed the study hypothesis of each study and the presence of HRT data for each study, and also extracted the data regarding the risk of lung cancer associated with HRT in each study meeting the selection criteria. Relevant data were identified according to the following priorities: (1) adjusted RR (aRR), controlling for potential confounders, and its 95% CI were the first priority (2) in studies that did not provide an aRR, the crude RR (cRR) and its 95% CI were calculated based on the size of the exposure group and the non-exposure group at the beginning of follow-up and the number of lung cancer patients occurring in each group during follow-up (3) when the RR was still not clear, data presented in an SR were used. In such cases, after assessing heterogeneity using the I-squared value (%), a meta-analysis using a random effect model was performed on studies with I-squared ≥50%, obtaining sES and its 95% CI. Additionally, publication bias was assessed using symmetry of the funnel plot and Egger’s regression. A subgroup analysis was performed based on the risk data by dividing studies into those where aRR was available and those where it was not. A p-value <0.05 was considered to indicate statistical significance, and the StataSE version 14.0 (Stata Corp., College Station, TX, USA) were used to perform the statistical analysis.
RESULTS
Figure 1 displays the selection process of the studies that were ultimately included in this review. A total of 126 potential papers were identified through hand searching, from which 112 papers were excluded, resulting in a final selection of 14 cohort studies. Two papers were excluded because they derived their data from the same cohort as another study. The study by Adami et al. [19] used the same participants as Persson et al. [20], and Adami et al. [19] was excluded due to its shorter follow-up period. Brinton et al. [33] used the same cohort as Brinton et al. [34], and the most recently published of these two papers was included.
Table 3 displays the data source, nation, follow-up period, aRR/cRR, and 95% CI for the 14 cohort studies that were ultimately included. Tem of these studies [20,24-32] were included in the four SRs presented in Table 1, while the other four [34-37] were newly selected using the snowballing search method.
Figures 2 and 3 are the forest plot and funnel plot obtained from our meta-analysis of the 14 studies. Since the I-squared value was 64.3%, a random effect model was used, and the results showed that the association between HRT and lung cancer was not statistically significant (sES, 0.99; 95% CI, 0.90 to 1.09). The funnel plot was not symmetrical, and the Egger regression analysis showed an effect in the small-scale studies (beta=1.7, p=0.016). Meta-analysis of the six studies providing information about aRR [26,27,30,32,35,36] showed an sES of 1.05 (95% CI, 0.92 to 1.20; I-squared, 14.3%), and the remaining eight studies [20,24,25,28,29,31,34,37] showed an sES of 0.99 (95% CI, 0.90 to 1.09; I-squared, 70.4%) (data not shown).

Forest plot made using random-effects summary estimates for 14 cohort articles. ID, name of first author_year of publication [reference number]; ES, effect size; CI, confidence interval.
DISCUSSION
The limitations of the existing 4 SRs included non-replication of the selected studies, different RR values reported for the same studies, lack of statistical significance in cohort studies, and the need to update the results due to the May 2012 end date of the literature search. Therefore, in order to overcome these limitations, we performed a hand search ending in September 2015. Nevertheless, the results were still not statistically significant. To summarize, in SR research using observational studies, the case-control studies showed a significance protective association between HRT and lung cancer in women, but the cohort studies showed no association whatsoever [24,38,39].
The present study used the previous SRs rather than a search of electronic databases, and applied a snowballing search method using referred, cited and related papers. These methods led to the inclusion of an additional four studies [34-37]. However, since the publication dates of those studies were between 2008 and 2010, in theory they should have been selected in the SR by Yao et al. [17], which incorporated studies published by May 2012. This finding demonstrates the utility of a snowballing search strategy based on previous SRS, using lists of referred, cited, and related articles.
Siegrfied [40] summarized the pre-clinical and post-treatment evidences suggesting estrogen to be a risk factor and a prognostic factor for lung cancer. A recent pooled analysis of six case-control studies reported that HRT reduced lung cancer risk [18], but the present SR of 14 cohort studies found no statistically significant association. This discrepancy could be explained by the different of HRT duration reflected in casecontrol studies and cohort studies [40]. Thus, further epidemiological analysis incorporating HRT duration instead of a binary classification of each subject’s HRT history is necessary.
In conclusion, this adaptive meta-analysis of cohort studies did not showed a statistically significant association between HRT and lung cancer risk in women. In spite of the broader search strategy, if the appropriate information cannot be obtained from the selected papers, the validity of the meta-analysis will inevitably be compromised. In the present study, since aRR was available in only six studies (43%), a subgroup analysis was performed, and no significantly different findings were observed. Ultimately, a pooled analysis of cohort databases will be required to overcome this limitation [23,41].
Notes
Conflict of Interest
The authors have no conflicts of interest associated with the material presented in this paper.