Short-term Effect of Fine Particulate Matter on Children’s Hospital Admissions and Emergency Department Visits for Asthma: A Systematic Review and Meta-analysis
Article information
Abstract
Objectives:
No children-specified review and meta-analysis paper about the short-term effect of fine particulate matter (PM2.5) on hospital admissions and emergency department visits for asthma has been published. We calculated more precise pooled effect estimates on this topic and evaluated the variation in effect size according to the differences in study characteristics not considered in previous studies.
Methods:
Two authors each independently searched PubMed and EMBASE for relevant studies in March, 2016. We conducted random effect meta-analyses and mixed-effect meta-regression analyses using retrieved summary effect estimates and 95% confidence intervals (CIs) and some characteristics of selected studies. The Egger’s test and funnel plot were used to check publication bias. All analyses were done using R version 3.1.3.
Results:
We ultimately retrieved 26 time-series and case-crossover design studies about the short-term effect of PM2.5 on children’s hospital admissions and emergency department visits for asthma. In the primary meta-analysis, children’s hospital admissions and emergency department visits for asthma were positively associated with a short-term 10 μg/m3 increase in PM2.5 (relative risk, 1.048; 95% CI, 1.028 to 1.067; I2=95.7%). We also found different effect coefficients by region; the value in Asia was estimated to be lower than in North America or Europe.
Conclusions:
We strengthened the evidence on the short-term effect of PM2.5 on children’s hospital admissions and emergency department visits for asthma. Further studies from other regions outside North America and Europe regions are needed for more generalizable evidence.
INTRODUCTION
The adverse health effects of air pollution on respiratory and cardiovascular diseases are well known to the public. Regulation and monitoring of air pollution are performed at both the national and international levels. Particulate matter (PM) is one type of air pollutant. It is not a specific chemical entity, unlike other commonly known pollutants such as ozone, sulphur dioxide, and nitrogen dioxide. It is a physical category of dust with different components mixed together [1]. The particle size determines the different categorizations: PM10 (less than 10 μm aerodynamic diameter) and PM2.5 (less than 2.5 μm aerodynamic diameter). PM2.5 is also known as fine PM.
PM2.5 has been reported to play a major role in increasing the chance of mortality due to cardiovascular diseases because it can penetrate the capillary vessel of the lungs and reach the alveoli [2,3]. Extensive research has been conducted on the association between PM2.5 and respiratory diseases including asthma. Asthma is a syndrome in which reversible respiratory obstruction occurs and is characterized by hypersensitiveness to allergens. When stimulated, a person experiences wheezing and dyspnea. In most cases, asthma is caused by a genetic predisposition and is triggered by environmental allergens.
The prevalence rate of asthma is high in children. In the case of South Korea (hererafter Korea), the prevalence rate of asthma in children steadily increased due to urbanization and westernization. In 2010, a national study based on the International Study of Asthma and Allergies in Childhood questionnaire found that 10.1% of elementary school students and 8.5% of middle school students had experienced symptoms of asthma in the past 12 months [4]. These numbers should not be ignored.
Recently published systematic reviews and meta-analyses reported the pooled relative risk (RR) of the number of hospital admissions and emergency department (ED) visits due to asthma as 1.023 (95% confidence interval [CI], 1.015 to 1.031, per 10 μg/m3 increase) when examining the effects of PM2.5 on the total population, and 1.025 (95% CI, 1.013 to 1.037, per 10 μg/m3 increase) when the subject was confined to children only [5]. Another review that examined the effects of PM2.5 on ED visits due to asthma reported a pooled RR of 1.036 (95% CI, 1.018 to 1.053, per 10 μg/m3 increase) [6]. However, existing studies contain several limitations. These studies were not focused on childhood asthma and only presented pooled effect estimates in children as subgroup analysis. Moreover, most of the relevant studies were conducted in North America and Europe [7-28], and although studies conducted in other regions exist [29-32], they did not consider the varying effects of PM2.5 according to different regions. The design of the study, the background PM2.5 mean concentration and variation of the region where the study was conducted, and the time of study may change the effects as well, but these factors were not adequately considered in existing studies.
In addition to the two reviews mentioned above, seven new relevant papers have recently been published [22-28]. Of these, the time-series studies assessed the exposure to air pollution by using the exposure value of the population-weighted average in between the measuring points of air pollution [22,24,27], and the case-crossover design studies used the method of matching individual addresses with the PM2.5 measures [25,26], which yielded more accurate results. Therefore, by including these recent developments, we tried to calculate more accurate pooled effect estimates of the effects of PM2.5 on childhood asthma and assess the variations of effects induced by differences in some factors such as region or date of research, which have been not adequately examined yet.
METHODS
Selection Criteria
We first determined some criteria for selecting relevant studies. They are as follows:
1) The subject of study was limited to children and adolescents under the age of 20.
2) Study results were limited to computerized records of hospital admissions and ED visits. Outpatient visits were excluded. Hospital admissions confirmed through interviews were not eligible. Subjective symptoms, decrease in pulmonary function, and use of emergency inhalers were not considered endpoints.
3) Effect estimates had to be presented as an odds ratio (OR) or RR.
Search Terms and Study Selection
When deciding on search terms, we minimized keywords in order to increase the sensitivity of our searches. Some of the search terms we used were child*, pediatric*, fine particulate matter*, fine particle*, PM2.5, asthma*, hospitalization, hospitalisation, admission*, ed, er, and emergency. We searched studies to include in our meta-analysis using PubMed and EMBASE in March of 2016. Moreover, we selected the final eligible studies after having two authors each independently select references according to the criteria above and the same search terms and then comparing the two lists.
Statistical Methods
The effect size was expressed as RR. We considered the OR as a proxy to the RR. In order to have all the effect estimates chosen from the selected studies to reflect the same 10 μg/m3 increment of PM2.5 concentration, we implemented meta-analyses after recalculating the β coefficient and 95% CI presented in each study. Because the purpose of this study is to combine and identify the effects from regions all over the world, generalization of heterogeneous parts of the research group was its goal. Therefore, the random effects model using the DerSimonian and Laird [33] estimation method was mainly considered, rather than the fixed effects model [33,34]. When estimating the pooled effect, the model takes into account both the between-study variation and the within-study variation and provides a greater confidence level than the fixed effects model. The I-squared value (%) was calculated in order to identify heterogeneity.
In the primary meta-analysis of this study, an effect estimate that could represent the selected studies was used. We used the same lag value that was presented in the original paper [35], but if a study presented multiple estimates from different lags, we selected the one with the largest effect size. This is because, generally, these works report the greatest effect size [36]. If a study did not have one effect estimate that could represent the research, we selected two or more values that were obtained from subjects that were mutually exclusive (that is, if a study did not present an effect estimate in whole participants but presented two or more separate values from stratified groups, we included those in the meta-analysis). In order to identify publication bias, we conducted the Egger’s test and identified the degree of asymmetry through a funnel plot [37].
Moreover, we conducted category-specific meta-analyses in order to determine what factors influenced the effect of PM2.5, if those influences were robust, and what factors contributed to the heterogeneity of effect estimates. We conducted the analyses by sorting the effect estimates into categories of age, results (records of hospital admissions or ED visits), season, design of the study, region, and the lag of exposure. We also conducted a separate analysis according to whether or not different pollutants were adjusted in the statistical model.
We hypothesized that the components of PM2.5 would change according to the time of the study and that the size of the effect could change according to the components. In addition, we thought that the variation and the mean concentration of PM2.5 in the region where the study was conducted might change the size of the effect. Therefore, through mixed-effects meta-regression, we derived an effect estimate of the time of the study, and the mean and standard deviation of the concentration in the study region on RR for childhood asthma.
All statistical analyses performed using R version 3.1.3 (Comprehensive R Archive Network: http://cran.r-project.org) and we carried out a series of statistical analyses described above through the meta package. All statistical analyses set a 5% significance level for the two-tailed test.
RESULTS
Selection of Relevant Studies and Extracting Effect Estimates and Their Confidence Intervals
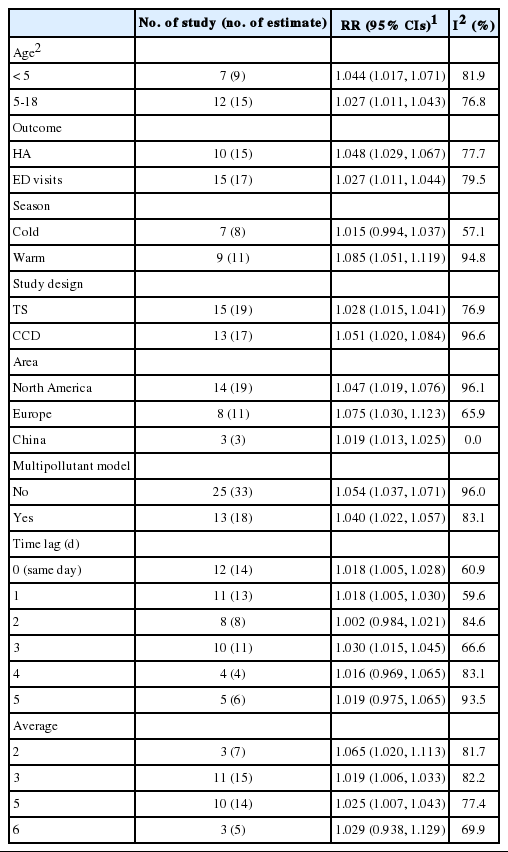
A total of 661 references were searched using the search terms mentioned above, and of those, we first selected 56 to examine in whole by excluding overlapping studies (n=171) and reading the titles and abstracts (n=490). Then we ultimately selected 26 studies according to the selection criteria and extracted effect estimates (Figure 1). The 26 studies were published between 1999 and 2016, and we summarized each of the research outlines and the main research results in Table 1. Most of the research was conducted in North America and Europe and both time-series and case-crossover designs were almost equally represented.
Selection process for systematic review and metaanalysis. PM2.5, fine particulate matter; ER, emergency room; CI, confidence interval.
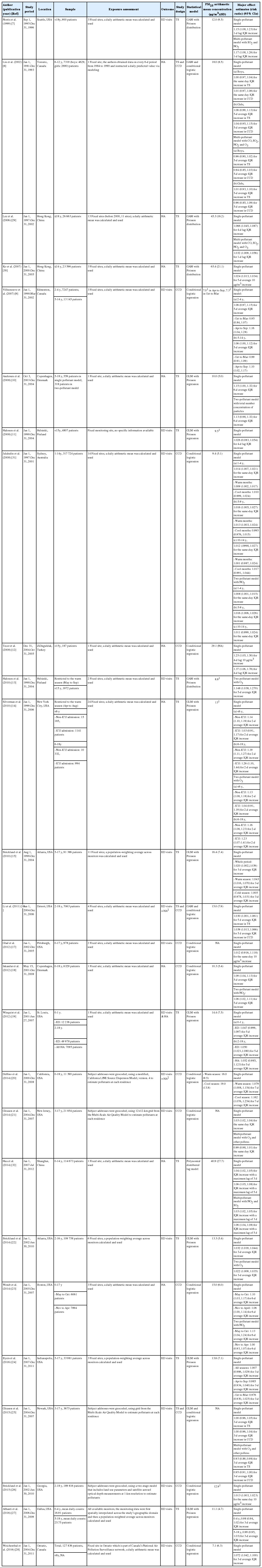
Summary of selected studies on the association of short-term fine particulate matter (PM2.5) exposure with pediatric HA and ED visits for asthma
After extracting all effect estimates and CIs from the main body of each research paper and its supplementary materials, we broke it down to a total of 244 effect estimates. Of those, we selected 33 representative effect estimates from each study to use in our primary meta-analysis.
Primary Meta-analysis
In the random effects model, we were able to find that when the concentration of PM2.5 increased by 10 μg/m3, the risk of a child’s hospital admission or ED visit increased by 4.8% (RR, 1.048; 95% CI, 1.028 to 1.067). The I-squared value, which shows the heterogeneity of the included studies, was 95.6%, a high figure. We presented a forest plot for the included effect estimates and pooled estimates (Figure 2).
Publication Bias
To schematically examine the tendency toward publication bias, we found a relatively symmetrical shape in the funnel plot and confirmed that there was not much of a bias because there was not statistically significant (p=0.42) in the Egger ‘s test (Figure 3).

Funnel plot for a possible selection bias in the primary meta-analysis (A). After removing three estimates (Anderson et al. [8], Tecer et al. [12], and Halonen et al. [13]) from the right-lower area in A, still symmetrical shape is shown (B). Each black circle denotes each effect estimate of the selected studies, and the vertical red dotted line denotes the pooled random effect risk ratio in the primary meta-analysis. The p-value is derived from Egger’s test.
Category-specific Meta-analyses
We found that the effects are greater on children below the age of five than on children ages 5 to 19, in warmer seasons, and in North America and Europe than in Asia. The pooled effect estimates extracted through the multi-pollutant model was also statistically significant (RR, 1.040; 95% CI, 1.022 to 1.057). According to the lags, the effect changed greatly from 0.2% to 6.5%, and the effect was large for 3-day lag and 3-day average lag (Table 2).
Meta-regression Analyses
We did not find a tendency toward change in the statistically significant RR according to the time of study and the standard deviation of the background concentration of the region of study. We found a negative tendency in the mean PM2.5 concentration by the region of study, but it was not statistically significant (β=-0.0008, p=0.14) (Figure 4).

Bubble plot and regression line for mixed-effect meta-regression of study mean fine particulate matter (PM2.5) concentration and effect estimate. The black circles denote each effect estimate and their sizes represent each weight. The bold red line indicates a linear relationship between study mean PM2.5 concentration and relative risk and the black dotted lines indicate a 95% confidence interval.
DISCUSSION
In the primary meta-analysis of the effect estimates obtained from the 26 studies, we found that in the short-term, when the concentration of PM2.5 increased 10 μg/m3, the risk of a child’s hospital admission or ED visit increased 4.8%, which is statistically significant. The effect of PM2.5 could be considered quite robust, since the effect was maintained to 4.0% even when we pooled the estimates extracted by the multi-pollutant model in this study. This number is greater than the 2.3% found among the total population presented in the aforementioned study of Zheng et al. [5]. These results show that children are more vulnerable to air pollution because their alveoli and airways are still growing, their immune systems are underdeveloped, and they spend more time outdoors, which increases ventilation [38].
Based on known biological mechanisms, the generation of reactive oxygen species (ROS) is accelerated because of the transition metal included in PM2.5. Oxidative stress from ROS may be related to epithelial cell destruction and allergic inflammation, and this process is known to be related to exacerbation of asthma [39]. Meanwhile, previous studies reported that arginase may participate in a process that fine particles exacerbate childhood asthma [40]. In vivo studies report that the overexpression of arginase influences the hyperresponsiveness of airways [41] and that fine particles exacerbate the airway’s responsiveness in asthma in murine models [42]. Human epidemiological studies have shown that the variation of the ARG1 and ARG2 genes—which are related to the manifestation of arginase in childhood asthma patients—is statistically significant [40,43].
In the preceding meta-analyses by Zheng et al. [5], they suggested 20 relevant studies on children’s asthma. We found a discrepancy between the selected studies of Zheng et al. [5] and ours even aside from seven papers published more recently. They cited several studies that we excluded in the process of extracting eligible studies. On the other hand, the six studies included in this study were not cited by the preceding study. We selected studies and extracted results carefully focusing on children. Therefore, we believe that the 26 references selected for this study comprise the best selection.
We found that when the concentration of PM2.5 increased by 10 μg/m3, the risk of a child’s hospital admission or ED visit increased by 4.8%. This value is greater than the 2.5% increase in children found in the preceding meta-analysis by Zheng, et al. [5]. The following are some reasons to explain this difference. First, the newly added original studies included several studies in which the RR exceeded 1.10 when the measure of effect estimates was converted to 10 μg/m3 per increase [7,9,13,20,23,28]. Second, while the previous study pooled the effect estimates from the 0-day, 1-day, or 2-day average lags, we used the model with the greatest effect size out of the lags reported in the original studies.
In this study, we found a difference in RR according to the season, and during the warmer seasons, the RR was 1.085 (95% CI, 1.051 to 1.119). The studies included in our meta-analysis showed quite consistent results [9,20,22,23,31]. We thought the reason for this was that during warmer seasons, children spend more time outdoors and therefore spend more time exposed to PM2.5. In addition, greater ventilation of buildings during these seasons makes it easier for air pollutants to penetrate inside the buildings. It was reported that the individual exposure concentration of PM2.5 that people living in well-ventilated environments showed high correlation to the concentration of the atmosphere [44]. The difference in components of PM2.5 according to the season may also be related, but because the extent of heterogeneity by region is too great, the evidence is not yet definitive [45-47].
In terms of the design of the studies, the pooled RRs for the time-series and the case-crossover design studies were 1.028 and 1.051, respectively. For the case-crossover design, the OR was calculated using the conditional logistic regression model. Compared to the RR, the OR has a tendency to overestimate the actual risk. However, it may be thought as a closer representation of reality than the exposure assessment of the time-series because a recently published case-crossover study more accurately matched air pollutants using the addresses of individuals [20,21,25,26]. Residential information of patients entering hospitals or visiting the ED cannot be reflected in time-series. If we suppose that PM2.5 having an influence on exacerbating asthma as true, even in one study region, there is a possibility that the large effect in certain area with a high concentration could be diluted because of smaller effects in other area with a low concentration. We think that the actual effect is somewhere between the RRs of the time-series studies and the ORs of the case-crossover studies.
When we examine the pooled RR of each lag, we can see that there is up to a 6% difference in value depending on the type of model. The effects of both the concentration three days before (3-day lag) and the average concentration over three days (3-day average lag) were considerable. This result is somewhat difficult to interpret. We need to consider the following factors when dealing with lags: that the ethnicities of the subject of study differ by regions and an accessibility to health services could change depending on the time of study. Through meta-regression analysis, we found a negative tendency among effect sizes depending on the mean concentration of PM2.5, but it was not statistically significant. Aside from the three studies in China which the mean concentrastion exceeded 30 μg/m3 (Figure 4), we did not find a negative tendency in the meta-regression analysis (β=-0.0004, p=0.90). Therefore, we could not draw conclusions in this study regarding such a limited tendency. A negative tendency means that the effect on asthma is smaller for regions where the mean concentrations of PM2.5 are higher. This means that the relationship between the mean concentration and the childhood asthma could be non-linear, or more specifically, supra-linear.
When we examine the results according to region in the category-specific analyses, the pooled RR of the three studies conducted in Shanghai and Hong Kong was 1.019, which is a smaller value than those in North America (1.047) and Europe (1.075). This is similar to the results of the previous meta-analysis that examined the short-term effects of PM2.5 on total mortality and cardiorespiratory mortality, and found that the pooled estimate in China was lower than in the US, Europe, Japan, and Australia [48]. A hypothesis that the components of PM2.5 in China are different from those of developed countries was raised regarding this finding. In other words, in China, the contributions of coal combustion and desert dust—rather than exhaust from automobiles—were greater than in other regions.
However, in a preceding meta-regression analysis including studies on PM10 and cardiorespiratory mortality conducted in China only, a statistically significant negative tendency was reported regarding the association between the mean concentrations of study regions and the effect sizes [49]. A study conducted across 27 US regions also reported that the effect of PM2.5 was greater in regions with lower background mean concentration, even though the result was not statistically significant [50]. In a cohort study on the effect of PM2.5 on cardiorespiratory mortality, the risks with the concentration level formed a supra-linear shape [2]. Therefore, for the regional effect variation in this study, the hypothesis that the effect was lowered in high concentrations seems more plausible, since only groups with resistance remain and detrimental effects on individuals vulnerable to PM2.5 occur in lower concentrations.
There are many other genetic and environmental factors reported to cause childhood asthma besides PM2.5. Another hypothesis, following hygiene theory, states that allergic reactions decrease when children are exposed to micro-organisms because immune reactions are suppressed. Since westernization is still in progress in China, the effects of PM2.5 on asthma may be small [51,52]. There may be an objection to this statement since the three Chinese studies included in this study were conducted in Shanghai and Hong Kong, two very westernized large cities, but the infrastructure of the residences and the lifestyles of children growing up in such regions are different from those of North America and Europe.
There are some limitations of this study. First, outpatient visits, use of inhalers, and other symptom outbreaks could all be considered health effects and consequences, but we confined the results to hospital admissions and ED visits which were mainly reported in previous studies. Therefore, the pooled effect estimate reported in our study might be underestimated. But in a study that uses surveys on symptoms and use of inhalers, the period between the exposure and outbreak could be imprecise. Moreover, results from a survey could be subjective. In cases of outpatient visits, we cannot exclude periodic follow-up cases. Second, we combined the RRs with the ORs because we deemed the OR to be proxy to the RR. Because of this, we may have calculated an overestimated value rather than the actual risk. However, in the case of Korea, hospitalization due to asthma among children between the ages of zero to 19 was 0.14% in 2014 [53]. The frequency of hospital admissions or ED visits due to asthma is rare so a possible bias will be negligible. Third, we could not control the innate heterogeneity of the selected studies. Components of PM2.5, ethnicities of the study population, and accessibility to health service as well as different age range, season, and adjusting variables or parameters in statistical models all probably affected the heterogeneity of the studies. However, we did not find a significant decrease of heterogeneity (Table 2). In order to obtain a more accurate pooled effect estimate, a meta-analysis should be conducted after an in-depth examination of the methods and quality of research.
The strength of this study is that we newly included seven recent studies in our meta-analysis. In addition, with a focus on children, we examined variations in effect of different possible factors, and presented the direction for future studies. In particular, we raised the need for an epidemiological study on regions besides China with high concentrations of PM2.5.
CONCLUSION
We found that in the short-term, when the concentration increased by 10 μg/m3, the risk of a child’s hospital admission or ED visit increased by 4.8%. If we consider the fact that air pollution affects a vast range of regions and many populations, this is not a negligible figure. A more fundamental solution is the reduction of the matter from emission sources, so we need to conduct studies on sources that emit PM2.5 and draft feasible environment-friendly policies for such emission sources.
ACKNOWLEDGEMENTS
This study was supported by the R&D Program for Society of the National Research Foundation funded by Ministry of Science, ICT and Future Planning, Republic of Korea (grant no. 2014M3C8A5030619).
Notes
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.