Validity of Self-reported Hypertension and Factors Related to Discordance Between Self-reported and Objectively Measured Hypertension: Evidence From a Cohort Study in Iran
Article information
Abstract
Objectives
Self-reporting can be used to determine the incidence and prevalence of hypertension (HTN). The present study was conducted to determine the validity of self-reported HTN and to identify factors affecting discordance between self-reported and objectively measured HTN in participants in the Ravansar Non-Communicable Diseases (RaNCD) cohort.
Methods
The RaNCD cohort included permanent residents of Ravansar, Iran aged 35-65 years. Self-reported data were collected before clinical examinations were conducted by well-trained staff members. The gold standard for HTN was anti-hypertensive medication use and blood pressure measurements. The sensitivity, specificity, positive and negative predictive values, and overall accuracy of self-reporting were calculated. Univariate and multivariate logistic regression were used to examine the discordance between self-reported HTN and the gold standard.
Results
Of the 10 065 participants in the RaNCD, 4755 (47.4%) were male. The prevalence of HTN was 16.8% based on self-reporting and 15.7% based on medical history and HTN measurements. Of the participants with HTN, 297 (18.8%) had no knowledge of their disease, and 313 (19.9%) had not properly controlled their HTN despite receiving treatment. The sensitivity, specificity, and kappa for self-reported HTN were 75.5%, 96.4%, and 73.4%, respectively. False positives became more likely with age, body mass index (BMI), low socioeconomic status, and female sex, whereas false negatives became more likely with age, BMI, high socioeconomic status, smoking, and urban residency.
Conclusions
The sensitivity and specificity of self-reported HTN were acceptable, suggesting that this method can be used for public health initiatives in the absence of countrywide HTN control and detection programs.
INTRODUCTION
The high prevalence of hypertension (HTN) makes it an important contributor to mortality and morbidity worldwide. In fact, high blood pressure (BP) is responsible for 13.0% of deaths globally, making it one of the leading global risk factors for mortality [1]. During the last 40 years, elevated BP has become more common worldwide, mainly due to population growth and aging in low-income and middle-income countries [1], whereas the prevalence of elevated BP in high-income countries has decreased [2]. Globally, approximately two-thirds of stroke cases and one-half of ischemic heart disease cases are attributable to non-optimal BP. These proportions are higher in more developed parts of the world [3].
HTN affects about one billion people worldwide, and it is estimated that by 2025, up to 1.56 billion adults worldwide will have HTN [4,5]. Worldwide, 7.1 million deaths (approximately 12.8% of the global total) and 64.3 million disability-adjusted life years (4.4% of the global total) are estimated to be due to non-optimal BP [3].
Since asymptomatic HTN is the most frequent form of HTN, regular BP measurements are the only way to diagnose HTN before the appearance of complications. In fact, HTN and its complications can be effectively controlled by early diagnosis and treatment of this condition. However, the rate of HTN control is very low worldwide [6,7].
Based on the existing evidence, the reduction of mortality due to stroke and heart failure depends largely on the early diagnosis and treatment of HTN, as long as the methods used to identify and treat patients are valid and evidence-based [8]. Thus, public knowledge about the disease, investigations into the prevalence of HTN and the proportion of individuals with HTN who receive treatment in specific regions, and efforts to identify the contributions of associated risk factors are all essential for the successful implementation of prevention strategies [9]. Self-reporting is a way to determine the incidence and prevalence of chronic diseases such as HTN. No previous report has assessed the validity of self-reported HTN in Iran. The present study aimed to determine the validity of self-reported HTN and to identify factors affecting discordance between self-reported HTN and objective measures of HTN among participants in the Ravansar Non-Communicable Chronic Disease (RaNCD) cohort.
METHODS
Study Design and Subjects
The RaNCD cohort study is part of the Prospective Epidemiological Research Studies in IrAN (PERSIAN) cohort, focused on permanent residents of Ravansar aged 35-65 years. In the PERSIAN cohort, all 18 cohort sites (covering different samples representative of the entire Iranian people, including different ethnicities) used the same questionnaire, which contained the following sections: general information (demographic information, socioeconomic status, lifestyle factors, occupational history, mobile device use, and physical activity), medical information (past medical history, past and present medicine use, family medical history, obstetric and gynecological history, oral health, and personal habits), and a nutrition questionnaire (food frequency questionnaire, dietary habits, water consumption, and supplement intake). In addition, biological samples containing blood, urine, hair, and nails were collected from all participants. The details of the study design and rationale for conducting the PERSIAN cohort have been presented elsewhere [10-12].
The population of Ravansar County is about 50 000, mainly of Iranian Kurdish ethnicity. In Ravansar County, there are 3 urban and 2 rural healthcare centers, as well as 32 active local primary health care units (health houses) in rural areas. One of the reasons for selecting Ravansar County as the location for this cohort study was that the population is mainly Kurdish, an ethnicity comprising roughly 45 million people in 4 countries who are very similar in culture, nutrition, lifestyle, and even genetic background. Furthermore, Ravansar County is located within 45 km of Kermanshah University of Medical Sciences, where the investigators of this study are based, which made the research very feasible.
Recruitment, Data Collection, and Measurements
Participants were invited to the study site for data collection. The PERSIAN cohort questionnaire consisted of 482 items divided into 3 major sections: general, medical, and nutrition. Each section was administered by a trained interviewer. To ensure that all procedures were performed in accordance with the PERSIAN cohort protocol, quality assurance (QA) and quality control (QC) measures were implemented by central and local QA/QC teams [10,11].
Each section was administered by a trained interviewer. There was no assigned order in which the sections needed to be completed; therefore, participants were directed to complete the sections based on the availability of the interviewers. Participants were invited by trained personnel who had a good command of Kurdish and other local languages. The invitation procedure included a face-to-face meeting at the participant’s home approximately 1 week prior to the appointment, and the cohort assistant called to remind the participant a day before the appointment.
For the purpose of this study, HTN was defined based on a systolic BP level of ≥140 mmHg and/or a diastolic BP of ≥90 mmHg, corresponding to the second stage of HTN [13], and/or a history of receiving treatment for HTN, determined by checking participants’ current medications. In order to investigate the use of anti-hypertensive treatments, participants were asked to bring all their medications (prescription and over-the-counter medicines) to the study center. Treatment of HTN was defined as current use of a pharmacological medication for the management of high BP. Participants taking an anti-hypertensive medication who did not show HTN on the day of the questionnaire were classified as having controlled HTN.
We used the wealth index as a proxy for economic status [14]. The wealth index was generated by applying principal component analysis to data on durable goods, housing characteristics, and other amenities. For the purposes of this study, participants were classified by age into 3 groups: 35-45 years, 46-55 years, and 56-65 years.
Statistical Analysis and Calculations
The validity of self-reported HTN was assessed in terms of sensitivity and specificity. Sensitivity was calculated as (true positives)/(true positives plus false negatives), and specificity as (true negatives)/(true negatives plus false positives). The positive likelihood ratio was defined as sensitivity/(1-specificity), and the negative likelihood ratio as (1-sensitivity)/specificity. The positive predictive value was defined as (true positives)/(true positives plus false positives), and the negative predictive value as (true negatives)/(true negatives plus false negatives).
Univariate and multivariate logistic regression were used to examine the role of demographic, socioeconomic and health-related behavioral factors in discordance (false positives and/or false negatives) between self-reported HTN and the gold standard. All variables with a p-value less than 0.3 in the univariate model were included in the multivariate analysis. A 2-sided alpha level of 0.05 was considered to indicate statistical significance. All analyses were carried out using Stata version 14.1 (StataCorp., College Station, TX, USA).
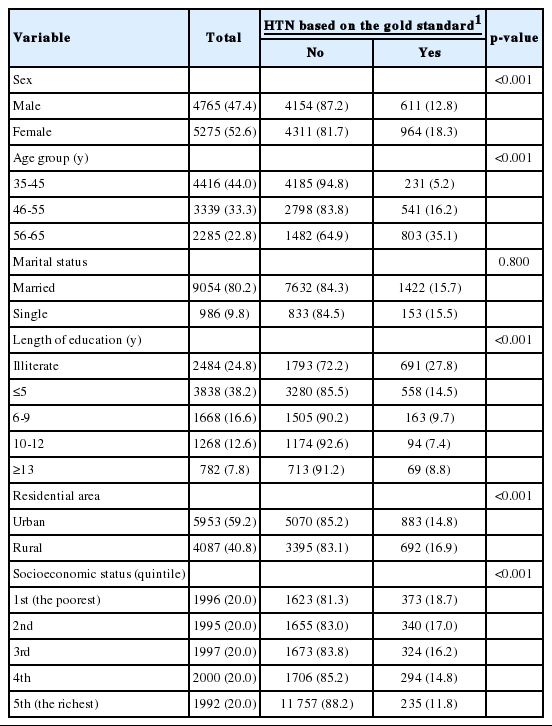
RESULTS
Of the 10 065 participants in the RaNCD cohort, 4755 (47.4%) were male. The plurality of individuals (44.0%) were aged 35-45 years, and the age category 56-65 years was the smallest (22.8%). The mean age of the male participants was 47.8±8.0 years, and the mean age of the female participants was 48.3±8.4 years. In total, 2484 of the participants were illiterate (24.8%), and only 7.8% had a post-secondary education. Almost 41.0% of the participants lived in rural areas (Table 1).
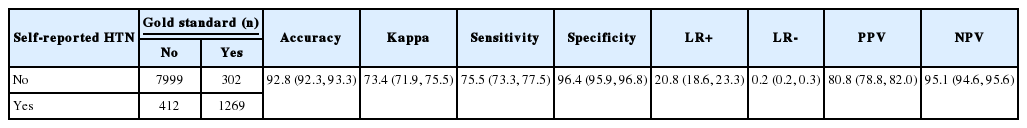
In the self-reported assessments, 25 people did not answer the questions and 61 were unaware of the concept of high BP; these participants were excluded from the study. Over 16% of the study population (n=1681; 16.8%) self-identified as having HTN, of whom 24.5% (n=412) had no HTN based on BP measurements or treatment for HTN (Figure 1). Based on history of treatment and/or BP measurements, 1571 participants had HTN (15.7%), of whom 297 (18.9%) were not aware of their disease, and 313 (19.9%) had uncontrolled HTN despite receiving treatment (Figure 1). Furthermore, 682 patients (59.1%) used 1 medication, 316 patients (27.4%) used 2 medications, and 152 (13.2%) used 3 medications. The highest number of reported anti-hypertensive treatments was 6 drugs used simultaneously. The sensitivity, specificity, and kappa values for self-reported HTN were 75.5%, 96.4%, and 73.4%, respectively (Table 2).
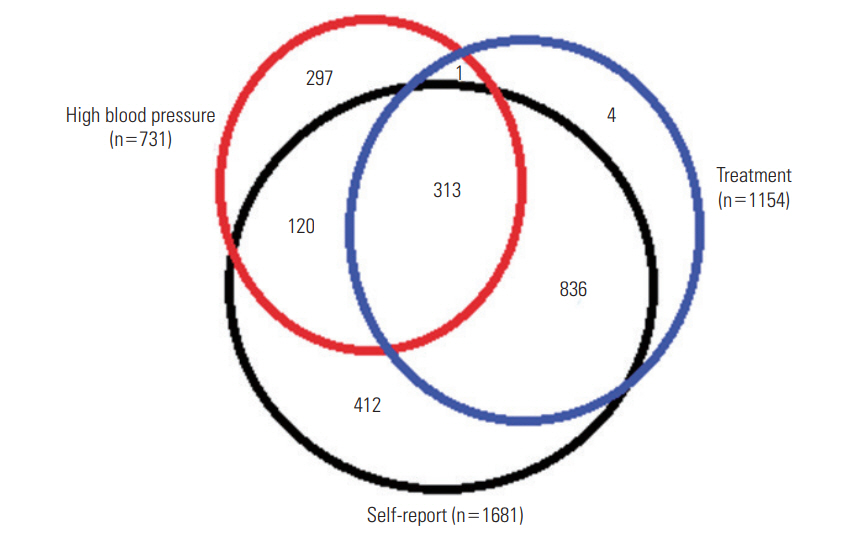
Frequency of people with self-reported, objectively measured hypertension and those who have received medication.
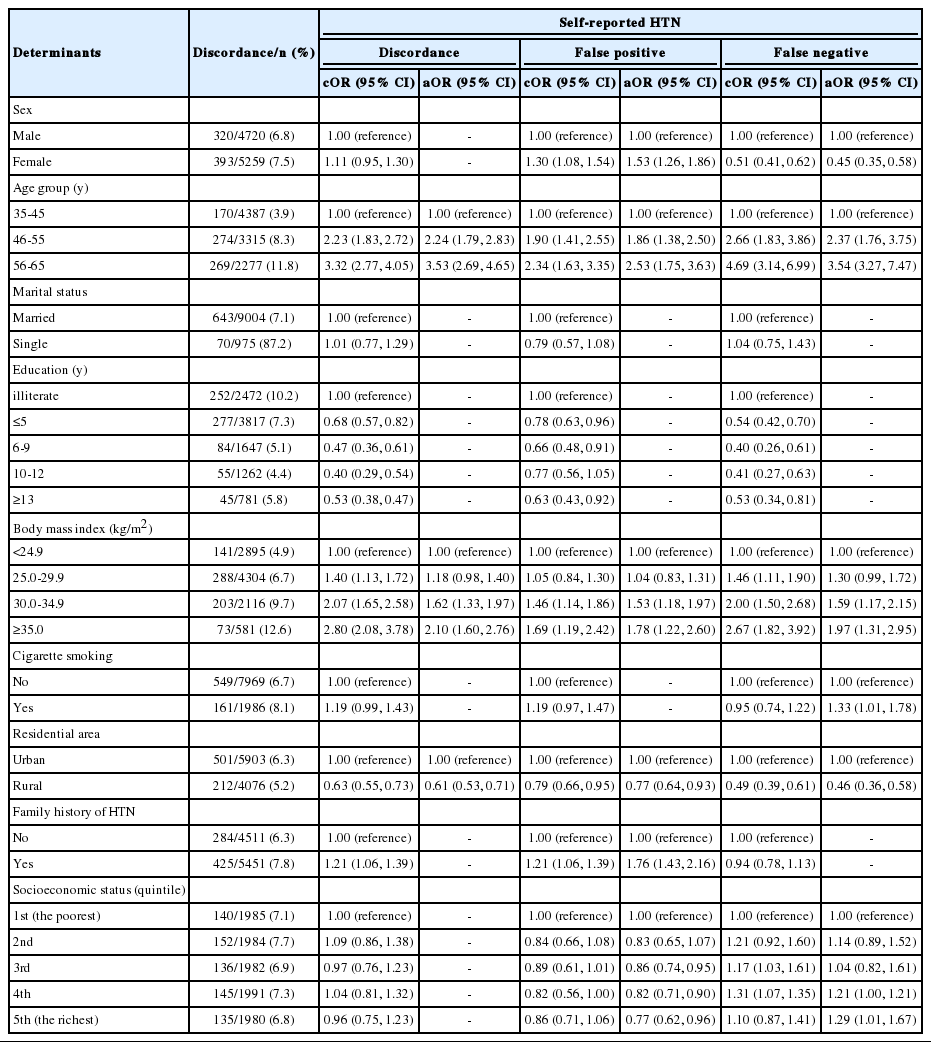
The multivariate assessment of factors explaining the gap (i.e., false positives and false negatives) between subjective (self-reported) and objective (BP measurements and/or treatment history) assessments of HTN suggested that the likelihood of false positives and false negatives increased with age and body mass index (BMI). There was a linear relationship between increasing BMI and the frequency of discordance of self-reported HTN, such that the odds ratio for discordance of self-reported HTN after controlling for confounding variables was 2.10 (95% confidence interval [CI], 1.60 to 2.76) times higher in those with a BMI >35.0 kg/m2 than in those with a BMI <24.9 kg/m2. The odds of false positives were higher and the odds of false negatives were lower in than in males and in those with higher socioeconomic status (Table 3). Interestingly, older age and higher BMI, as well as smoking, increased the odds of both false positives and false negatives of self-reported HTN, even after adjustment for other variables. In addition, living in a rural area decreased the odds of both false positives and false negatives of self-reported HTN. While having a high wealth index decreased the likelihood of false positives for self-reported HTN, it increased the likelihood of false negatives (Table 3).
DISCUSSION
The self-reported prevalence of HTN among 35-65-year-old participants in the RaNCD cohort was 16.5%, while it was 15.7% based on treatment history and/or measurements of BP; these prevalence rates are lower than those reported in other studies for this age group [8,15,16]. In addition, the proportions of those who were aware of their disease and were managing it correctly were higher than has been reported in similar previous studies [8,17-19]. This could have resulted from public awareness campaigns about the dangers of high BP and the importance of controlling it in recent years [19]. In Iran in 2008, approximately 25.0% of Iranians aged 25-64 years had HTN, of whom 34.0% were aware of having elevated BP; 25.0% were taking anti-hypertensive medications, and 24.2% of the treated patients had controlled HTN (males, 25.7%; females, 23.5%) [20].
Generally, self-reported HTN has high sensitivity and specificity, and a moderate kappa and agreement coefficient [21]. In the present study, the sensitivity and specificity of self-reported HTN were 75.5% and 96.4%, respectively. The sensitivity of self-reported HTN varies across countries; it was found to be 73.0% in South Korea (hereafter Korea) [22], 82.4% in Thailand [23], 72.0% and 80.0% in white and black Americans, respectively [24], 83.2% in Spain [25], 73.0% in Russia, 37.7% in China, and 31.4% in South Africa [21]. Previous studies have shown that the quality of provided health services is a reason for differences in the validity of self-reported conditions [21,22]. When the quality of health services improves, the sensitivity of self-reported conditions becomes higher for various diseases [22]. Since respondents’ awareness of the nature of their diseases can affect the accuracy of their self-reporting, it is assumed that intervention programs—including public education campaigns, knowledge dissemination, and the infrastructure of health examination programs—may influence differences across countries in the awareness of diseases and risk factors [22].
With respect to the specificity of self-reporting, representative studies with larger samples have shown that the specificity of self-reporting is higher than its sensitivity, for nearly all chronic conditions [10,11].
Exploring the role of demographic factors in discordance showed that false positive reports were more common in females than in males, but that false negatives were more common in males than in females, which is in line with the findings of other studies [25]. The high false positive rate in females can be attributed to females more frequent use of health services compared to males [26]. Discordance increased with age for both false positives and false negatives. In similar studies, the validity of self-reporting decreased with age for most chronic diseases, such as cancer [27], stroke [28], diabetes, and HTN [29]. Given that the results of the present study and similar previous studies have shown that the specificity of self-reporting is higher than its sensitivity, and the prevalence of chronic diseases increases with aging, the age-related increase in the prevalence of chronic diseases can be considered as a reason for the reduced validity of self-reporting in older individuals.
Our findings showed no association between education and the validity of self-reported HTN. In other studies, education showed different effects on self-reporting for chronic diseases [22,24,29].
One of the unanticipated findings of the study was that the validity of self-reported HTN was higher among rural residents than among urban residents. Since rural areas have less access to quality health services than urban areas, the validity of self-reported HTN was expected to be lower in residents living in rural areas. However, the results were the opposite. This could imply that the health houses that are located across rural areas in Iran are improving local residents’ awareness of HTN and diabetes as part of their mission to provide primary care services [30].
At the univariate level, smoking was associated with higher false positive and negative rates. However, at the multivariate level, no relationship was found between smoking and an increased likelihood of self-reported false positives, but an association was found between smoking and an increased likelihood of false negatives for self-reported HTN. Reports from elsewhere have shown divergent results in this regard. Significant relationships were found in studies conducted in China and Hong Kong [22,31], but no significant relationship was found in Korea [22]. Differences in the proportions of false negatives and false positives in these studies may help explain the discrepancies in their results.
Discordance became more frequent as BMI increased. The role of BMI has not been assessed in most previous studies. The relationship between overweight and the validity of self-reported HTN was only assessed in one study, which showed no relationship between the validity of self-reported HTN and BMI [32]. The relationship observed in this study might have been related to the lower use of health care and health awareness of obese participants [21,33].
The odds of successful HTN control has been reported to be 50-60% with a single medication (monotherapy) and 70-79% with combination therapy [34]. In the present study, nearly 60% of patients used a single medication to control HTN. In similar studies, 50-80% of patients used monotherapy, and 20-30% used combination therapy [8,35-37]. Since using antihypertensive medication reduces the likelihood of stroke by 30-40%, the risk of myocardial infarction by 20-25%, and the risk of heart failure by 50% on average [38], it is essential to educate patients about the proper management and control of HTN.
Limitations and Strengths
All studies conducted to determine the validity of self-reported HTN contain limitations, such as an artificially elevated number of false positive cases due to white coat syndrome. To avoid causing white coat syndrome, HTN was measured twice on each arm of every person, and the mean value of the 4 measurements was recorded as the BP for that individual. It is not possible to generalize the results of this study to the entire population of the PERSIAN cohort because we only examined people in the age range of 35-65 years living in a Western region of Iran. Although public health awareness about chronic conditions such as HTN might be similar throughout Iran, studies regarding this issue need to be replicated at all the sites of the PERSIAN cohort. Despite these limitations, the present study included a large sample size and used high-quality cohort data collected by trained researchers.
To further increase the validity of self-reporting, health programs should be implemented with the goal of improving the general knowledge of the public, especially older people. In the absence of a countrywide HTN control and detection program, self-reporting can be used as an appropriate tool for control and prevention of diseases. Generally, the validity of self-reporting is lower in older and obese (BMI>30.0 kg/m2) people than in young people and those with a normal BMI. Given that those groups are at a higher risk of developing chronic diseases such as HTN and diabetes, health intervention programs and improvements in the general knowledge of the public are essential.
Notes
CONFLICT OF INTEREST
The author hase no conflicts of interest associated with the material presented in this paper.
ACKNOWLEDGEMENTS
RaNCD is part of the PERSIAN national cohort, and we would like to thank Prof. Reza Malekzadeh, the Deputy of Research and Technology at the Ministry of Health and Medical Education of Iran and Director of the PERSIAN cohort, as well as Dr. Hossein Poustchi, the Executive Director of the PERSIAN cohort, for all their support during the design and implementation of the RaNCD cohort.
This study was supported by the Ministry of Health and Medical Education of Iran and Kermanshah University of Medical Sciences (grant No. 92472).