Incidence, Risk Factors, and Prediction of Myocardial Infarction and Stroke in Farmers: A Korean Nationwide Population-based Study
Article information
Abstract
Objectives
This study was conducted to determine the incidence and risk factors of myocardial infarction (MI) and stroke in farmers compared to the general population and to establish 5-year prediction models.
Methods
The farmer cohort and the control cohort were generated using the customized database of the National Health Insurance Service of Korea database and the National Sample Cohort, respectively. The participants were followed from the day of the index general health examination until the events of MI, stroke, or death (up to 5 years).
Results
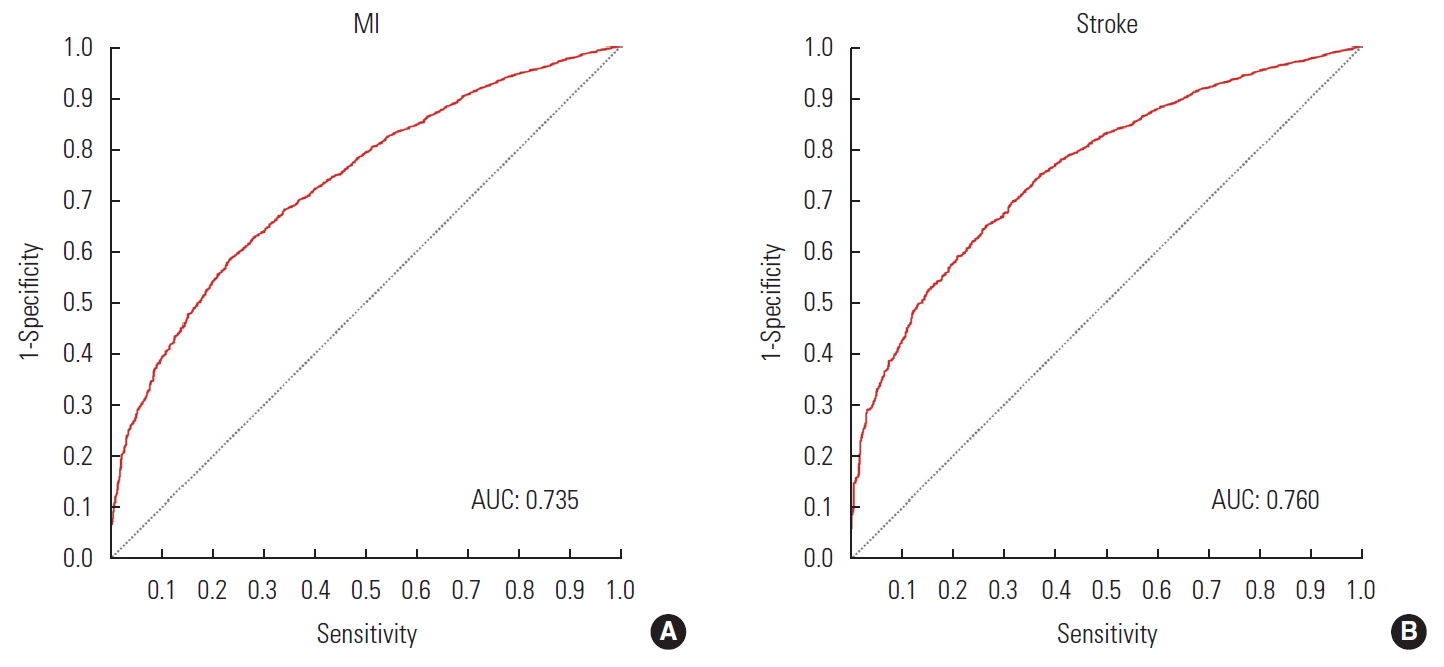
In total, 734 744 participants from the farmer cohort and 238 311 from the control cohort aged between 40 and 70 were included. The age-adjusted incidence of MI was 0.766 and 0.585 per 1000 person-years in the farmer and control cohorts, respectively. That of stroke was 0.559 and 0.321 per 1000 person-years in both cohorts, respectively. In farmers, the risk factors for MI included male sex, age, personal history of hypertension, diabetes, current smoking, creatinine, metabolic syndrome components (blood pressure, triglycerides, and high-density lipoprotein cholesterol). Those for stroke included male sex, age, personal history of hypertension, diabetes, current smoking, high γ-glutamyl transferase, and metabolic syndrome components (blood pressure, triglycerides, and high-density lipoprotein cholesterol). The prediction model showed an area under the receiver operating characteristic curve of 0.735 and 0.760 for MI and stroke, respectively, in the farmer cohort.
Conclusions
Farmers had a higher age-adjusted incidence of MI and stroke. They also showed distinct patterns in cardiovascular risk factors compared to the general population.
INTRODUCTION
Farmers in Korea face high levels of morbidity due to the declining farming population, aging workforce, and high labor intensity [1,2]. Compared to the general population, farmers have a greater risk of not only musculoskeletal diseases related to injury [3,4], but also cardiovascular diseases (CVD) [5,6], respiratory diseases [7,8], and skin diseases [9,10]. Moreover, limited access to healthcare in rural areas is also one of the main causes of negative health outcomes in this population [11,12].
Myocardial infarction (MI) and stroke are among the major causes of death worldwide [13,14]. Due to advances in medical treatments, the rate of complications and death following MI and stroke has substantially declined. However, these events typically cause a heavy medical burden, as they are often accompanied by chronic complications. Therefore, preventative approaches for early interventions by identifying high-risk groups among the population are very important. On the basis of identified risk factors, prediction models of MI and stroke events among the general population have been developed [15,16].
However, farmers receive chronic occupational exposure to physical and chemical factors distinct from those experienced by the general population [17-19]. Thus, patterns of disease in farmers may differ from those in the general population. Nonetheless, research on the health of farmers is limited to small-scale studies, and there is a lack of research on the incidence, risk factors, and prediction models for CVDs in this population using large-scale medical insurance billing information. This study drew data from the National Health Insurance Service of Korea (NHIS) database, analyzed the incidence and risk factors of MI and stroke among farmers compared to the general population, developed a prediction model for the risk of disease in the next 5 years, and validated the prediction model.
METHODS
Data Source and Study Approval
This nationwide population-based cohort study was conducted using the NHIS database [20]. Korea has a single-payer insurance system that covers 99% of the entire population. The NHIS database includes enrollees’ socioeconomic information, healthcare usage information, and diagnosis and treatment information. Information on regular health examinations and lifestyle patterns was extracted from the general health examination database. General health examinations are conducted once every 2 years for all employees, heads of households, and individuals aged 40 and above.
Study Population
The farmer cohort was established based on a customized database of farming households (Figure 1). Farming households were selected among farmers and fishers who were local policyholders of NHIS and who were eligible for reduced insurance contribution premiums on the basis of living in agricultural or fishing communities. The inclusion criteria were as follows: (1) those aged 40 to 89 in late 2010, (2) those who received a general health examination at least once during the indexing period from 2010 and 2011, and (3) those with no history or diagnosis of MI or stroke before the general health examination during the index period. Those who reported a history of these diseases in the survey given as a part of the general health examination or those who used related healthcare services were excluded from the analysis. The index date of each individual was the date of the general health examination during the index period (Figure 2).
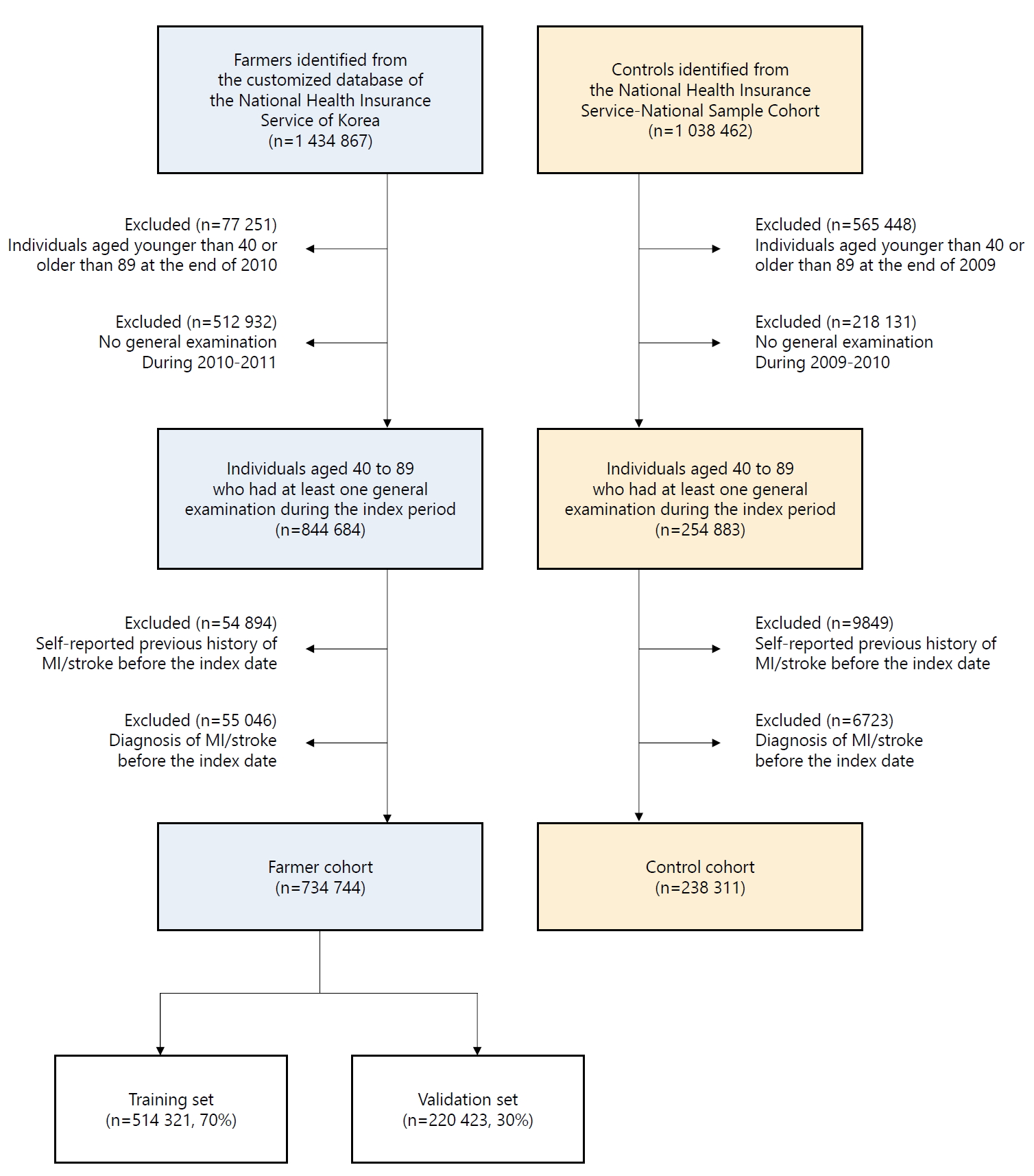
Participant selection flow chart. The National Health Insurance Service was our data source. A total of 734 744 farmers and 238 311 controls were recruited from the customized database and the National Sample Cohort. Of the farmers, 514 321 (70%) were used for training of the prediction model and 220 423 (30%) were used for validation. MI, myocardial infarction.
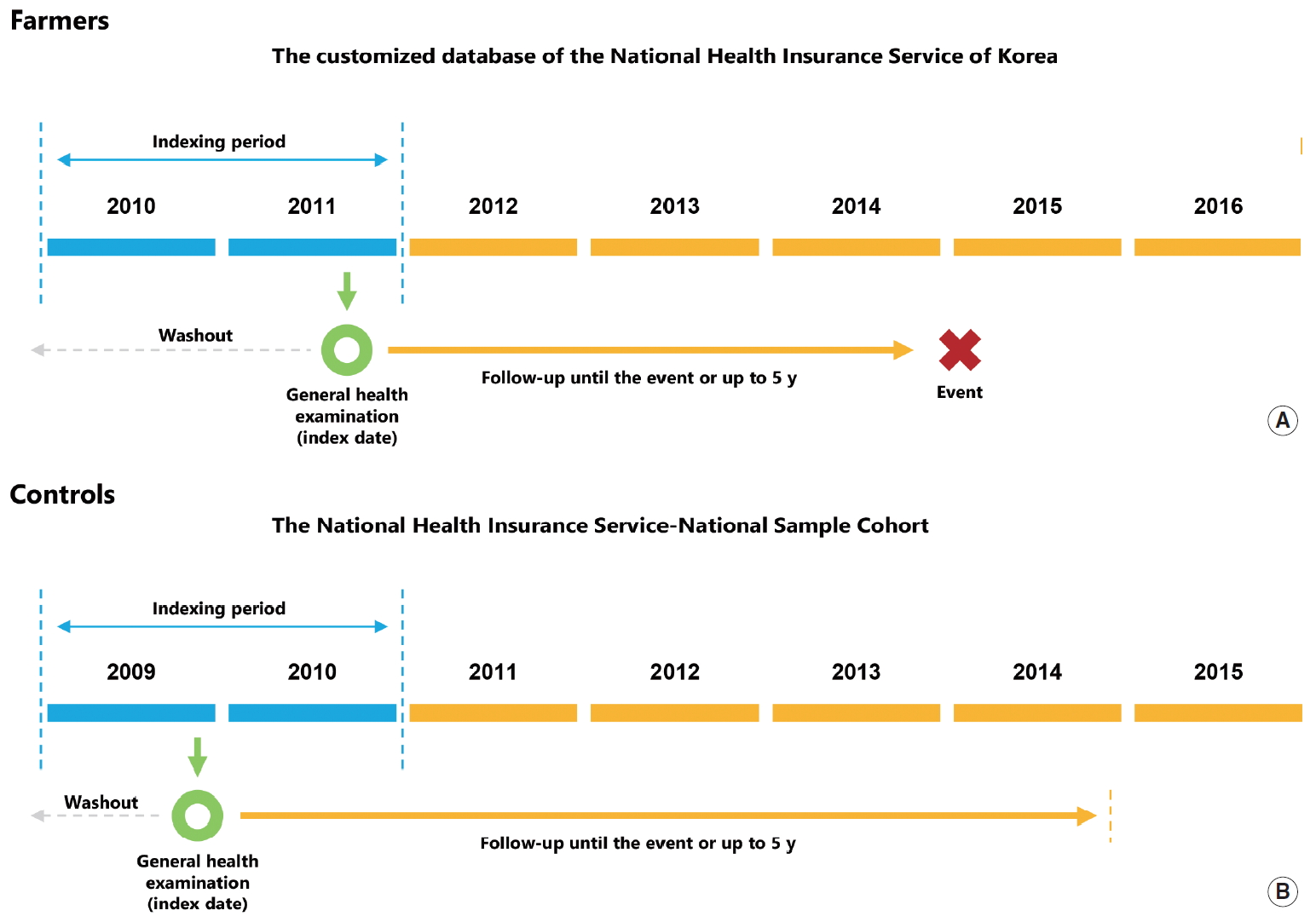
Schematic illustration of study design. Because of data availability, farmers (A) and controls (B) were recruited between 2010-2011 and 2009-2010, respectively. All participants were followed up from the index date (the day when a participant had a general health examination) until an event of interest or 5 years. Any participants with a previous history or diagnosis of myocardial infarction and/or stroke were excluded from the study.
The comparison cohort was the National Health Insurance Service-National Sample Cohort (NHIS-NSC) [21]. This sample cohort is a 2% stratified random sample of the entire population based on sex, age, insurance type, insurance premium quartile, and region. The available data include health service use and the results of general health examinations from 2002 to 2015. Due to data availability, the age in the comparison cohort was calculated based on age figures in late 2009, and the index period ran from 2009 to 2010. In the comparison cohort, similarly to the farmer cohort, those who were aged 40 to 89, those who received general health examinations at least once during the index period, and those without a history of MI and stoke were included in the analytic sample. Individuals in these 2 cohorts were followed from the index date until the event of MI, stroke, or their death (up to 5 years).
Diagnosis of Incident Myocardial Infarction and Stroke
For the diagnosis of MI and stroke, the International Classification of Diseases, 10th revision (ICD-10) operational definitions, which consider imaging results, procedures, and medication prescriptions for examination and treatment, were employed.
An ICD-10 code of I21 (acute transmural MI) was used for the diagnosis of MI. The diagnosis was limited to cases for which the patient was hospitalized at a medical facility and received both tests for biomarkers (troponin T, troponin I, or creatinine kinase-MB) and percutaneous coronary intervention (coronary angiography, percutaneous transluminal coronary angioplasty, percutaneous coronary stent placement, percutaneous coronary atherectomy, percutaneous coronary thrombectomy, aortocoronary bypass graft, or off-pump coronary artery bypass surgery) [22].
Stroke was diagnosed based on ICD-10 codes of I60 (non-traumatic subarachnoid hemorrhage), I61 (non-traumatic intracerebral hemorrhage), I62 (other and unspecified non-traumatic intracranial hemorrhage), I63 (cerebral infarction), or I64 (stroke, not specified as hemorrhage or infarction). This diagnosis was assigned in cases where the patient was hospitalized in a medical facility, underwent the necessary imaging exams for diagnosis (magnetic resonance imaging, computed tomography, or angiography for the cranial area), and received a percutaneous intervention (percutaneous thrombectomy or thrombolysis) or was prescribed related medication (aspirin, cilostazol, clopidogrel, ticlopidine, triflusal, heparin, bemiparin, reviparin, enoxaparin, dalteparin, fondaparinux, nadroparin, parnaparin, rivaroxaban, dabigatran, apixaban, coumadin, sarpogrelate, indobufen, mesoglycan, dipyridamole, or tissue plasminogen activator). Unlike patients with MI, stroke patients receive a percutaneous intervention only when they arrive within a specified time period (the “golden time”) after the stroke occurs. Since percutaneous interventions are therefore only given to a limited number of patients, in order to identify more patients, an operational definition that includes the prescription of medications as conservative treatments is commonly used [23].
Definition of Metabolic Syndrome
According to the criteria of the National Cholesterol Education Program Adult Treatment Panel, metabolic syndrome was defined as the presence of at least 3 of the following 5 factors [24]: (1) waist circumference more than 90 cm in male and 80 cm in female, (2) blood triglyceride levels more than 150 mg/dL or the use of medication for hyperlipidemia, (3) serum high-density lipoprotein cholesterol below 40 mg/dL for male and below 50 mg/dL for female, (4) blood pressure more than 130/85 mmHg or the use of medication for hypertension, and (5) fasting blood sugar levels over 100 mg/dL or the use of medication for diabetes.
Statistical Analysis
In each cohort, for the incidence rate of MI and stroke, estimates for each group, as well as the age-standardized estimates based on the standard age structure in Korea in 2010, were calculated. In order to investigate the independent risk factors of MI and stroke in each cohort, Cox proportional hazards regression using time-to-outcome variables from the start of the follow-up period was conducted. In selecting the variables, the proportional hazards assumption and multicollinearity were tested.
In order to construct the 5-year prediction model for MI and stroke, multivariate logistic regression was used. For the training of the model to fit the data, data from 70% of the participants in the farmer cohort were used. The data from the remaining 30% of the participants in the farmer cohort were used to test the accuracy of the developed model. The main measure to evaluate the performance of the prediction model was the area under receiver operating characteristic curve (AUROC).
All statistical analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). Statistical significance was defined using a threshold of below 5%.
Data and Code Availability
The NHIS provided the data that support the methods and results of this study. Access to the data is possible under the data use agreement for this study in a limited manner and cannot be given publicly. More detailed information about the data can be obtained on the following website: https://nhiss.nhis.or.kr/bd/ab/bdaba013eng.do. All statistical code used in the study is available in the following public repository: http://dx.doi.org/10.17632/frwm44m3vz.1.
Ethics Statement
All data were anonymized to protect individual privacy. This study was approved by the Korean National Institute for Bioethics Policy (NHIS-2018-1-308), and since the study used anonymous data, it was not necessary to receive informed consent from each participant.
RESULTS
Study Population
The farmer cohort comprised 734 744 individuals in the customized NHIS database, and the comparison cohort comprised 238 311 individuals (Figure 1). The demographic characteristics and the general health examination results of these individuals at the index time are summarized in Table 1. The farmers were statistically significantly older than individuals in the comparison cohort (62.82±10.36 vs. 54.31±10.16 years; p<0.001). The proportion of males was significantly higher among farmers than among the general population (76.1 vs. 47.5%; p< 0.001). A history of various chronic diseases, including metabolic syndrome, was more prevalent in farmers than in the general population.
Incidence of Myocardial Infarction and Stroke
The 734 774 individuals in the farmer cohort and the 238 311 individuals in the comparison cohort were followed longitudinally from the index time for up to 5 years.
In the farmer cohort, 3860 incident MIs were recorded over 3 662 916.9 person-years of follow-up (group incidence rate, 1.053/1000 person-years). In the comparison cohort, 630 incident MIs were recorded over 11 898 313.5 person-years of follow-up (group incidence rate, 0.529/1000 person-years). The age-standardized incidence rates based on the 2010 standard population structure were 0.766/1000 person-years in the farmer cohort and 0.585/1000 person-years in the comparisoncohort.
In the farmer cohort, 3162 incident strokes were recorded over 3 665 033.8 person-years of follow-up (group incidence rate, 0.863/1000 person-years). In the comparison cohort, 322 incident strokes were recorded over 1 190 694.9 person-years (group incidence rate, 0.271/1000 person-years). The age-standardized incidence rates based on the 2010 standard population structure were 0.559/1000 person-years in the farmer cohort and 0.321/1000 person-years in the comparison cohort.
Risk Factors for Incident Disease
The independent risk factors of MI and stroke in the farmer cohort and the comparison cohort are summarized in Table 2.
The common risk factors of MI across the two cohorts were male sex, old age, current smoking, a history of diabetes, low serum γ-glutamyl transferase levels, hypertension, high serum triglyceride levels, and low serum high-density lipoprotein cholesterol levels. A history of hypertension was statistically significant in the farmer cohort (hazard ratio [HR], 1.217; 95% confidence interval [CI], 1.114 to 1.329) and not in the comparison cohort (HR, 0.958; 95% CI, 0.771 to 1.191), but the HRs in each cohort were not significantly different.
The common risk factors of stroke in the two cohorts were old age, current smoking, and a history of diabetes. In the farmer cohort, male sex was associated with a slightly higher risk of stroke (HR, 1.295; 95% CI, 1.157 to 1.451), but in the comparison cohort, no effect of sex was observed (HR, 0.941; 95% CI, 0.663 to 1.335). Similarly, a self-reported history and a presence of hypertension were statistically significant risk factors in the farmer cohort (HR, 1.119, 95% CI, 1.016 to 1.232 and HR, 1.393; 95% CI, 1.240 to 1.565, respectively), but not in the comparison cohort (HR, 1.085; 95% CI, 0.797 to 1.479 and HR, 1.315; 95% CI, 0.923 to 1.875, respectively). However, the HRs were not significantly different. High serum γ-glutamyl transferase levels were identified as a risk factor of stroke in the farmer cohort (HR, 1.001; 95% CI, 1.001 to 1.002), but were not significant in the comparison cohort (HR, 1.001; 95% CI, 0.999 to 1.003). Although the HRs were not significantly different, high serum triglyceride levels (HR, 1.127; 95% CI, 1.033 to 1.230) and low serum high-density lipoprotein levels (HR, 1.132; 95% CI, 1.024 to 1.244) were identified as significant risk factors in the farmer cohort, but were not statistically significant in the comparison cohort (HR, 1.027; 0.779 to 1.354 and HR, 1.156; 95% CI, 0.870 to 1.537, respectively).
Five-year Prediction Model in the Farmer Population
In order to predict MI and stroke within 5 years from the date of the general health examination in the farmer cohort, a prediction model for each disease was developed, using 70% (n=514 321) of the data from the farmer cohort (n=734 744) for the development and training of the models, and the remaining 30% (n=220 423) as a validation set. The accuracy of the 5-year prediction models for MI and stroke are presented in Figure 3.
DISCUSSION
This study found that the group incidence rate and age-standardized mortality rate of MI and stroke were substantially higher in the farmer cohort than in the general population. Moreover, the risk factors of these 2 diseases in farmers differed from the known risk factors in the general population.
Previous studies reported that the incidence and prevalence of various health conditions, including musculoskeletal, CVD, and respiratory diseases, were higher in farmers [4-6,8,10]. Factors that contribute to the higher health risk in farmers may include (1) chemical factors such as exposure to gases or harmful chemical substances in pesticides and agricultural machinery; (2) physical factors such as long working hours, high-intensity labor, ergonomic burden, high temperatures, and noise pollution; and (3) psychological factors such as agricultural stress [9,25-29]. Therefore, health examinations and provision of health services for the diagnosis and prediction of diseases in farmers, who are a high-risk population, are imperative. However, health access is actually substantially lower in the farmer population than in other populations, and specialized health examinations and monitoring of major diseases for farmers are limited to the management of some musculoskeletal diseases [11,12].
Compared to the general population, farmers demonstrated a different pattern of risk factors for MI and stroke. One of the main differences was that sex had no significant effect on stroke risk in the general population, but the risk was higher in males than in females in the farmer population. The role of sex in stroke risk has been the topic of ongoing discussions [30,31]. It is known that in subtypes of stroke other than subarachnoid hemorrhage there are no differences according to sex [32]. Higher exposure to occupational risk factors in male farmers than in female farmers might have contributed to the difference in risk associated with sex observed in the 2 cohorts. However, since the data analyzed in this study did not include information on individuals’ intensity and duration of labor or exposure to occupational risk factors, potential mechanisms and explanations can only be suggested to a limited degree.
A history of hypertension was an independent risk factor for MI and stroke among farmers, but not among the general population. Since a higher proportion of farmers were elderly compared to the general population, hypertension may have had a longer disease period in the farmer cohort, contributing to the identification of history of hypertension as a risk factor. It is known that factors such as use of pesticides, long working hours, physical exertion, and agricultural stress cause hemodynamic changes, including hypertension [33-36]. Moreover, lifestyle choices that are more prevalent in farmers than in people in other occupational categories, such as drinking, smoking, and certain eating habits, are important risk factor of hypertension. Therefore, it is possible that hypertension is experienced starting at an earlier age in farmers than in the general population, and the interaction between pesticide exposure and hypertension may have caused the different contribution of a history of hypertension to disease incidence in the 2 cohorts.
The high occupational stress of farmers caused by poor working conditions, environmental and climate conditions, economic problems, uncertainty, and social isolation can influence hypertension. However, the HRs of the independent factors examined were not substantially different between the 2 cohorts, and considering the number of participants, the interpretation of statistical significance requires some caution. Moreover, the data analyzed lacked information on the age at onset of hypertension, length of disease, or exposure to pesticides, so the independent effects of each factor could not be examined in detail. High serum γ-glutamyl transferase levels were also found to significantly increase the risk of MI in farmers, but not in the general population. Although it is difficult to propose an exact mechanism, elevated serum γ-glutamyl transferase levels due to the exposure to pesticides and other agricultural chemicals may contribute to this observed difference [37-39].
The AUROCs of the prediction models for MI or stroke from the time of general health examination up to 5 years among farmers were 0.735 and 0.760, respectively. These figures suggest a moderate fit of the models; in other words, the models did not demonstrate a high predictive accuracy. This study and the prediction models did not use additional survey information on occupational factors that could improve the predictive accuracy of the models among farmers. Therefore, although these models were developed and validated using data from the farming population, there is a limitation to their predictive accuracy.
The main limitation of this study is that data specific to the farming population were not used as analytic variables when the risk factors of MI and stroke were identified and prediction models were built. For example, if variables such as type of crops cultivated, occupational environment, main tasks, labor duration and intensity, length of work, types of pesticides used, amount of pesticides used, the environment where the pesticides were used, and whether appropriate protective gear was used had been analyzed, the risk factors and mechanisms in this population could have been examined more clearly. Another limitation of this study is that all analyses and predictions were based on the underlying health status and lifestyle factors at the time of the general health examination. Health status and lifestyle choices are not fixed in each individual, and in a recent large-scale study, it was reported that adjustments in lifestyle choices can alter the progression of metabolic syndrome and reduce the risk of disease [40].
There may also have been misclassification of the farmer cohort and the general population cohort. The farmer cohort was constructed by extracting households included in the administrative registration data. Therefore, family members who were not farmers could have been included in the farmer cohort. By limiting the study population to individuals aged 40 to 80, we attempted to minimize the possibility of misclassification. Lastly, the NHIS-NSC cohort used to represent the general population was based on the entire population and therefore included a small number of farmers. This misclassification might have led to underestimation of the incidence rate of disease and independent risk factors in farmers compared to the general population.
Despite the above limitations, the strengths of this study are that it calculated the national age-standardized incidence rates of MI and stroke among farmers compared to the general population, which has rarely been studied, and that it investigated the independent risk factors of each disease in the farmer cohort and the general population. Further research that incorporates more detailed survey items and a longer follow-up period is necessary.
Notes
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
FUNDING
This work was carried out with the support of the Cooperative Research Program for Agriculture Science & Technology Development (project No. PJ01250901) and the Rural Development Administration, Republic of Korea.
ACKNOWLEDGEMENTS
None.
Notes
AUTHOR CONTRIBUTIONS
Conceptualization: SL, SBK. Data curation: SL, HSK. Formal analysis: SL. Funding acquisition: SBK. Methodology: SL, HL, HSK, SBK. Project administration: SBK. Visualization: SL. Writing – original draft: SL. Writing – review & editing: SL, HL, HSK, SBK.