The Impact of Household Economic Deterioration Caused by the COVID-19 Pandemic and Socioeconomic Status on Suicidal Behaviors in Adolescents: A Cross-sectional Study Using 2020 Korea Youth Risk Behavior Web-based Survey Data
Article information
Abstract
Objectives
Economic hardship has a serious impact on adolescents’ mental health. The financial impact of the coronavirus disease 2019 (COVID-19) pandemic was more severe for low-income families, and this also impacted adolescents. This study aimed to examine the associations of economic deterioration (ED) caused by the COVID-19 pandemic and low socioeconomic status (SES) with adolescents’ suicidal behaviors.
Methods
This study analyzed data from the 2020 Korea Youth Risk Behavior Web-based Survey, which included 54 948 middle and high school students. Odds ratios (ORs) of suicidal ideation, suicidal planning, and suicide attempts related to ED and SES were calculated using multivariable logistic regression. We calculated relative excess risks due to interaction to assess additive interactions.
Results
The ORs for suicidal ideation, suicidal planning, and suicide attempts related to combined severe ED and low SES were 3.64 (95% confidence interval [CI], 3.13 to 4.23), 3.88 (95% CI, 3.09 to 4.88), and 4.27 (95% CI, 3.21 to 5.69), respectively.
Conclusions
ED and low SES were significantly associated with suicidal behaviors in adolescents. Although no significant additive interaction was found, the ORs related to suicidal ideation, suicidal planning, and suicide attempts were highest among adolescents from low-income families with severe ED. Special attention is needed for this group, considering the increased impact of economic inequality due to the COVID-19 pandemic.
INTRODUCTION
Adolescent suicide is a serious problem. One out of 7 adolescents globally experiences a mental disorder, which accounts for 13% of the disease burden within this age group, and suicide is the fourth leading cause of death worldwide among those aged 15–19 years [1]. In Korea, suicide has been the leading cause of death among adolescents since 2011 [2].
Mental illnesses developed during adolescence also result in a substantial burden on society [3,4]. A systematic review showed that adolescent depression was associated with suicidal behavior and depression in adults [4]. Another study showed that adolescent suicidal ideation with no history of suicide attempts increased the risk of suicidality as an adult, with the risk increasing among those who had suicide attempts [5]. Furthermore, suicide attempts during adolescence are associated with a lower education level and occupational outcomes, as well as negative adulthood mental health [6]. Therefore, interventions to address adolescent mental health are both an important opportunity and a moral obligation for society [3].
Numerous factors including depression, impulsivity, interpersonal conflicts, and financial difficulties are known risk factors for adolescent suicide [7]. Among these risk factors, socioeconomic status (SES) has a particularly significant impact on adolescent mental health through various pathways, including on the individual, family, peer, school, and neighborhood levels [8]. According to the family stress model, which is widely used to explain family-level pathways, economic hardships such as negative financial events make parents feel pressured and disrupt their parenting, which negatively affects the mental health of their children [9].
In addition, low-income families lack the resources to cope with economic difficulties and are prone to income volatility [10]. Therefore, parents of low-income families are more vulnerable to pressure when they experience negative financial events, which is also likely to affect their children. Prime et al. [11] proposed a family resilience framework for the coronavirus disease 2019 (COVID-19) era and considered pre-existing economic hardship to be a major vulnerability.
In terms of mental health in adolescents, studies from various countries have found the COVID-19 pandemic to cause increased depression and anxiety [12,13]. Positive family relationships have been found to be a protective factor against these negative impacts [13,14], and conflict with parents was found to be a risk factor [15]. For some, the pandemic posed an unexpected opportunity to strengthen their family relationships, while it increased the risk of domestic violence and maltreatment for others [14,16].
The COVID-19 pandemic has also been found to intensify pre-existing inequalities in Korea [17,18]. The unemployment rate was higher for non-standard, non-regular workers, and income decline was most concentrated in low-income families [17]. Temporary workers and self-employed workers experienced more short-term work or unpaid leave than regular workers and professional workers [18].
One study that included adolescents in Korea during the COVID-19 pandemic found that the economic status of middle school students’ families affected depression levels due to conflict with parents [19]. Two studies have also examined the economic impact of the COVID-19 pandemic on adolescent suicidal tendencies [20,21]. One found an association between the deterioration of a household’s economic status and the risk of suicide but treated SES as a confounder [20]. The other examined depression and suicidal ideation only and did not consider the additive interaction between the economic impact of the COVID-19 pandemic and SES [21].
Given the negative economic impact the COVID-19 pandemic has had on low-income families in particular [17], it is necessary to examine how economic inequality, which was strengthened by the COVID-19 pandemic, has exacerbated disparities in adolescent mental health. From a public health perspective, assessing the additive interaction is especially important since it would help determine the group for which an intervention would be most effective [22]. However, to our best knowledge, no studies have examined the additive interaction between the impact of economic deterioration (ED) due to the COVID-19 pandemic and low SES on adolescent mental health in Korea. Therefore, this study aimed to examine the associations between ED and low SES on suicidal behaviors in Korean adolescents, focusing particularly on their interaction on an additive scale, which can help when devising effective interventions under limited-resource conditions.
METHODS
Data
The study data were collected from the 2020 Korea Youth Risk Behavior Web-based Survey (KYRBS). The KYRBS is a nationally representative survey of middle and high school students in Korea conducted annually by the Korea Disease Control and Prevention Agency (KDCA) since 2005. The KYRBS aims to examine the health behaviors of Korean adolescents and develop indicators that can provide evidence for evaluating the effects of adolescent health promotion programs and compare adolescent health behaviors across countries. To ensure that the sample is nationally representative, the KYRBS uses a multi-stage stratified clustered sampling design [23]. Its reliability has also been proven [24]. In 2020, the survey was conducted from August to November, with responses from 54 948 middle and high school students.
Variables
Dependent variables
Three types of suicidal behaviors were used as dependent variables. First, suicidal ideation was defined based on an answer of “yes” to the question “For the past 12 months, have you ever seriously thought of suicide?”. Second, answering “yes” to the question “For the past 12 months, have you ever made a specific plan to commit suicide?” was considered to indicate suicidal planning. Lastly, an answer of “yes” to the question “For the past 12 months, have you ever attempted suicide?” was considered to indicate a suicide attempt.
Independent variables
Economic deterioration caused by the COVID-19 pandemic
Participants were asked, “Do you think COVID-19 has made the economic condition of your family more difficult than before?”. There were 4 possible answers (“very much,” “yes,” “no,” and “not at all”).
Family SES
Family SES was assessed using the question “How is the financial condition of your family?”. There were 5 possible answers (“high,” “mid-high,” “middle,” “mid-low,” and “low”). We considered answers of “high” and “mid-high” to indicate “high,” “middle” to indicate “middle,” and “mid-low” and “low” to indicate “low.” Although accurate family income data were not included in the 2020 KYRBS results, the subjective self-reported SES of individuals was found to be reliable in terms of adolescent mental health [25–27]. We also conducted a sensitivity analysis using 2 variables (whether he/she lived with his/her family and whether his/her family received financial assistance from other people or institutions due to economic hardship) as indicators that represented SES.
Covariates
Age, sex, residential district, parental education, and cohabitation with one’s family were included as covariates. Of the 54 948 respondents, data on 139 respondents’ ages were missing. All the respondents answered the question about school grade, however, and these data were used to infer the ages of the small proportion of respondents with missing data on their ages. In addition, since many participants did not answer the question about the education level of their parents, we carried out multiple imputations and transformed it into a dummy variable with 4 distinct categories: college graduates or above, both parents; college graduate or above, mother only; college graduates or above, father only; and other.
Statistical Analysis
First, the general characteristics of the study participants were organized (Table 1). For categorical variables, we used unweighted counts with weighted percentages (%), and weighted means and standard deviations (SDs) were used for age.
Second, we evaluated the associations of both ED and low SES with suicidal behaviors using multivariable logistic regression and presented the odds ratios (ORs) for each exposure combination with 95% confidence intervals (CIs). In addition, we calculated the relative excess risk due to interaction (RERI) to assess the additive interaction [22,28]. If the RERI is greater than 0, it implies a positive additive interaction [22]. The additive interaction was considered to indicate significance if the 95% CI of the RERI did not include 0.
Third, we applied multiple imputations for the education level of both parents and conducted the same analysis. We also conducted a sensitivity analysis using 2 variables (living with one’s family and the experience of financial assistance) as indicators of SES.
All statistical analyses were conducted using R version 4.1.2 (https://www.r-project.org/). To analyze complex survey data, we used the “survey” package (https://cran.r-project.org/web/packages/survey/survey.pdf).
Ethics Statement
We submitted our research proposal to the Seoul National University Institutional Review Board and were approved with an exemption (IRB No. E2203/004-001).
RESULTS
The basic characteristics of the study population according to ED are shown in Table 1. Of the 54 948 participants, 16 839 (30.0%) responded that their family suffered from ED. The proportion of those who experienced suicidal ideation, suicidal planning, and suicide attempts were 9.5%, 2.9%, and 1.6%, respectively, in adolescents from families not affected by the COVID-19 pandemic. All of these figures were higher in the ED group, for which the proportion of those who experienced suicidal ideation, suicidal planning, and suicide attempts were 14.1%, 5.0%, and 3.0%, respectively. Among those with a low SES, 3 times more adolescents were from families that experienced ED caused by the COVID-19 pandemic (24.1%) than were from families that were not economically impacted by the pandemic (7.7%).
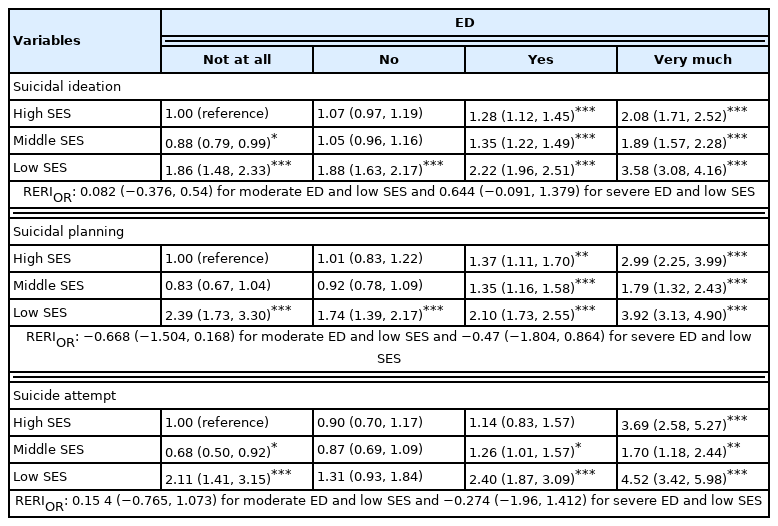
To examine the associations of suicidal behaviors with ED and low SES, multivariable logistic regression was conducted, the results of which are shown in Table 2. Both ED and low SES were found to be significantly associated with suicidal behaviors after adjusting for covariates. The ORs of combined severe ED and low SES were 3.58 (95% CI, 3.08 to 4.16), 3.92 (95% CI, 3.13 to 4.90), and 4.52 (95% CI, 3.42 to 5.98) for suicidal ideation, suicidal planning, and suicide attempts, respectively. The additive interaction between moderate or severe ED and low SES was found not to be significant. The results of the analysis not adjusted for covariates are shown in Supplemental Material 1.
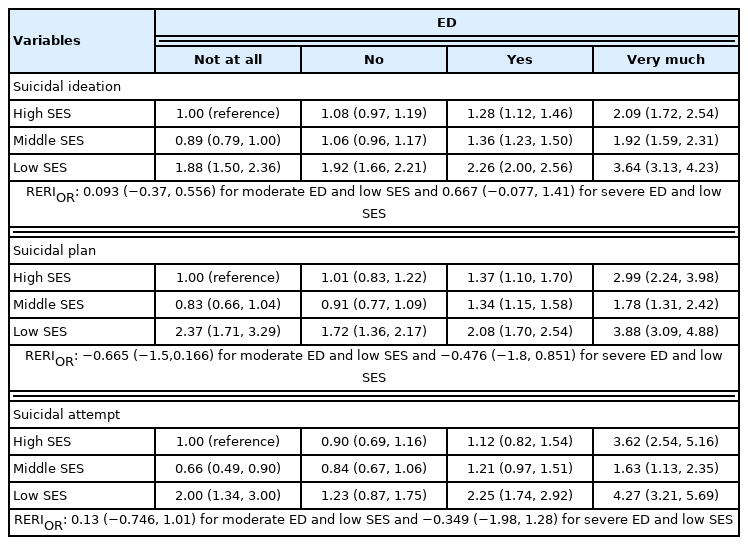
In Table 3, the analysis results using multiple imputations are shown. The ORs of combined moderate ED and low SES were 2.26 (95% CI, 2.00 to 2.56), 2.08 (95% CI, 1.70 to 2.54), and 2.25 (95% CI, 1.74 to 2.92) for suicidal ideation, suicidal planning, and suicide attempts, respectively. For combined severe ED and low SES, the ORs for suicidal ideation, suicidal planning, and suicide attempts were 3.64 (95% CI, 3.13 to 4.23), 3.88 (95% CI, 3.09 to 4.88), and 4.27 (95% CI, 3.21 to 5.69), respectively. No significant additive interaction was found between moderate or severe ED and low SES.
The results of the sensitivity analyses are shown in Supplemental Materials 2–5. We conducted the same analysis, including multiple imputations for the experience of financial assistance (Supplemental Materials 2 and 3) and living with one’s family (Supplemental Materials 4 and 5). Neither model differed significantly from the main model, with the associations between combined severe ED and the variables showing the highest values. The additive interaction was found to be significant for living with one’s family. The additive interaction between the experience of financial assistance and severe ED was also significant for suicidal ideation.
DISCUSSION
This study examined the associations of ED and low SES with suicidal behaviors in Korean adolescents. We also studied the additive interaction between the 2 variables to determine whether the negative impact was concentrated among adolescents from low-income families. Both ED and low SES were found to be significantly associated with the 3 types of suicidal behaviors examined in this study (suicidal ideation, suicidal planning, and suicide attempts). This finding is consistent with the results of previous studies on the association between ED and youth mental health [20,21]. Mental health problems are also widely known to be more common in socioeconomically disadvantaged children, and the negative impact increases as poverty persists over time [29].
The additive interaction between low SES and ED was not found to be significant in the main analysis. A previous study on the effect modification by income spectrum may help to explain this result [10]. ED can have a negative impact on adolescent mental health since it can cause relative deprivation for adolescents from high-income families and induce fear in middle-income families of downward mobility to a low-income bracket [10]. Nonetheless, the ORs for suicidal ideation, suicidal planning, and suicide attempts were highest in relation to combined low SES and severe ED. This tendency was also consistently observed in the sensitivity analysis. Adolescents from low-income families are more likely to recognize the worsening economic situation of their families [30]. Both the direct and indirect effects of poverty on mental health are cumulative [31]. Thus, it is clear that special attention must be given to low-income families, which were greatly affected by the COVID-19 pandemic, given the magnitude of the association found in this study.
For adolescents at the intersection of low SES and severe ED, the OR associated with suicide attempts was the highest among the 3 types of suicidal behaviors. Attempted suicide is the single most meaningful predictor of completed suicide [1] and is negatively associated with occupational and educational performance [6]. After suicide has been attempted once, it is likely to recur [32]. Adolescence is a period during which the surrounding environment has a great influence on brain development, with the effects likely to last a lifetime [3,33]. Therefore, it is best to prevent suicide attempts from occurring in terms of both the moral imperative and the economic cost to society [3].
In times of economic recession, the deterioration of a family’s economic condition and unemployment in a child’s parents have been found to relate to negative mental health outcomes in children [34]. The 1997 Asian financial crisis increased the suicide rates of several East Asian countries including Korea, Japan, and Hong Kong, with unemployment appearing to contribute to some of these associations [35]. Given the tremendous economic impact of the COVID-19 pandemic, its influence on adolescents should also be examined in detail. Youth mental health has already been found to have deteriorated in many countries due to the COVID-19 pandemic [36], and the rate of adolescent psychiatric treatment was found to have increased after the start of the COVID-19 pandemic [37].
The negative effects of the COVID-19 pandemic were not distributed equally, meaning that low-income families saw a more substantial negative impact [17,18]. The decline in income was worst among self-employed and special workers, among which the poverty rate also soared [18]. The COVID-19 pandemic also exposed some of the limitations of Korea’s income security system, which has led to debates on a variety of topics, including compensation for the economic losses experienced by self-employed workers [38]. Like many other countries, the Korean government implemented multiple large-scale supplementary budgets to address the economic impact of the COVID-19 pandemic, but further measures are needed.
In the event of failure to properly intervene to address inequalities deepened by the COVID-19 pandemic, these inequalities will continue into the next generation, strengthening the vicious cycle of poverty and poor mental health [29]. Therefore, special attention should be given to adolescents from vulnerable families. Furthermore, adolescents from low-income families are more likely to be exposed to adverse childhood experiences (ACEs) [39]. In this study, we were unable to determine whether ED led to ACEs, and follow-up studies should be conducted to examine the conditions of economic hardship that increase individuals’ vulnerability to ACEs.
This study had several limitations. First, a cross-sectional design was used, which limits the exploration of causality. Longitudinal studies are needed to further examine causal relationships. Second, we used subjective, self-reported responses to measure SES and ED, meaning that SES could have been influenced by ED, possibly leading to misclassification. However, in the sensitivity analysis examining the effect of living with one’s family and the experience of financial assistance as indicators of SES, no significant differences from the main analysis were found. Third, this study did not examine the mechanism through which ED and low SES affects suicidal behaviors. Further studies are needed to evaluate the pathways by which the economic conditions of parents affect the mental health of their children during the COVID-19 pandemic.
This study is still significant, however, since it was the first to examine the impact of combined ED caused by the COVID-19 pandemic and household SES on Korean adolescents’ suicidal behaviors. Using a single common reference is more informative when examining the effects of 2 variables simultaneously [22]. Although no significant additive interaction was found, the ORs for suicidal ideation, suicidal planning, and suicide attempts were highest among adolescents from low-income families with severe ED. In addition, we analyzed a nationally representative sample, so the results can be applied to all Korean adolescents. The findings of this study can provide important evidence from a public health policy perspective to help identify adolescents in need of special attention.
SUPPLEMENTAL MATERIALS
Supplemental materials are available at https://doi.org/10.3961/jpmph.22.241.
Notes
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
FUNDING
None.
ACKNOWLEDGEMENTS
None.
Notes
AUTHOR CONTRIBUTIONS
Conceptualization: Kang S, Hwang SS. Data curation: Kang S. Formal analysis: Kang S. Funding acquisition: None. Methodology: Kang S, Hwang SS, Jeong Y, Park EH. Visualization: Kang S, Jeong Y, Park EH. Writing – original draft: Kang S. Writing – review & editing: Kang S, Hwang SS, Jeong Y, Park EH.