Predisposing, Enabling, and Reinforcing Factors of COVID-19 Prevention Behavior in Indonesia: A Mixed-methods Study
Article information
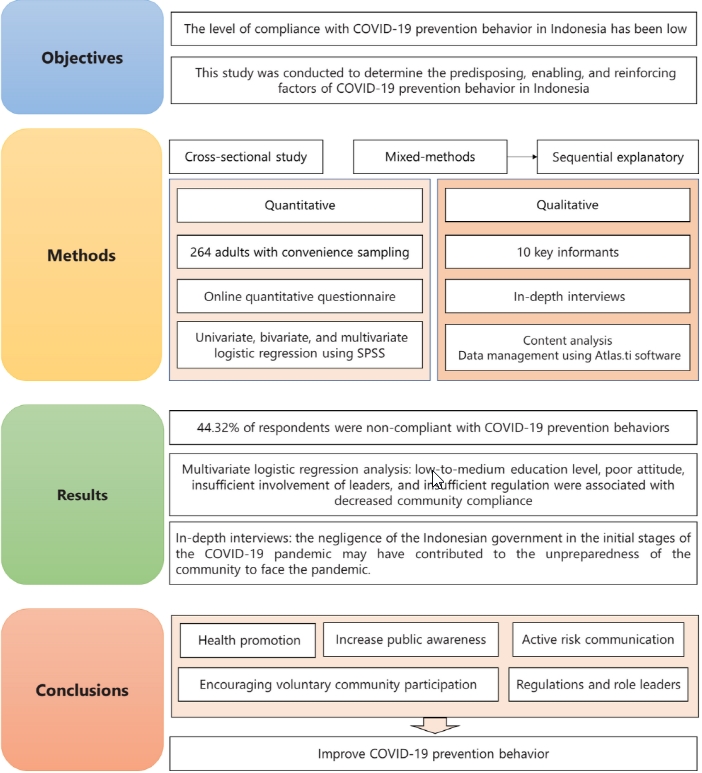
Abstract
Objectives:
To prevent the spread of coronavirus disease 2019 (COVID-19), behaviors such as mask-wearing, social distancing, decreasing mobility, and avoiding crowds have been suggested, especially in high-risk countries such as Indonesia. Unfortunately, the level of compliance with those practices has been low. This study was conducted to determine the predisposing, enabling, and reinforcing factors of COVID-19 prevention behavior in Indonesia.
Methods:
This cross-sectional study used a mixed-methods approach. The participants were 264 adults from 21 provinces in Indonesia recruited through convenience sampling. Data were collected using a Google Form and in-depth interviews. Statistical analysis included univariate, bivariate, and multivariate logistic regression. Furthermore, qualitative data analysis was done through content analysis and qualitative data management using Atlas.ti software.
Results:
Overall, 44.32% of respondents were non-compliant with recommended COVID-19 prevention behaviors. In multivariate logistic regression analysis, low-to-medium education level, poor attitude, insufficient involvement of leaders, and insufficient regulation were also associated with decreased community compliance. Based on in-depth interviews with informants, the negligence of the Indonesian government in the initial stages of the COVID-19 pandemic may have contributed to the unpreparedness of the community to face the pandemic, as people were not aware of the importance of preventive practices.
Conclusions:
Education level is not the only factor influencing community compliance with recommended COVID-19 prevention behaviors. Changing attitudes through health promotion to increase public awareness and encouraging voluntary community participation through active risk communication are necessary. Regulations and role leaders are also required to improve COVID-19 prevention behavior.
Graphical abstract
INTRODUCTION
On February 11, 2020, the World Health Organization announced a new virus named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as the cause of coronavirus disease 2019 (COVID-19) [1]. Preventive actions to reduce the spread of COVID-19 have been taken in Indonesia, starting with large-scale social restrictions [2,3], lifestyle changes [3], and the implementation of health protocols such as mask-wearing, hand-washing, maintaining a social distance, reducing mobility, and avoiding crowds [4]. In 2021, Howard et al. [5] stated that the use of masks was effective in preventing the transmission of COVID-19 only when compliance was high. Regular hand-washing with soap was also recommended as a basic protective measure against COVID-19 [6], while an increase in physical distance has been found to be associated with a reduced risk of COVID-19 transmission [7].
Despite the practice of COVID-19 prevention behaviors in Indonesia, the number of cases increased until its initial peak in July 2021 (at almost 57 000 cases), then rose to a subsequent peak in January 2022 (at approximately 65 000 confirmed cases) [8]. Low community compliance was a potential contributor. Based on the Social Demographic Survey of the Impact of COVID-19, compliance with mask-wearing had not been maximized; as many as 20% of respondents were relatively unlikely to wear masks, only 8 people of 10 people frequently washed their hands with soap, and only 6 respondents of 10 respondents reported using hand sanitizer [9]. Approximately 87% of respondents were aware of the physical distancing policy or the importance of maintaining distance, but only 72% of people had regularly kept their distance in the past week [9]. In comparison, a study in the United Kingdom showed a high willingness to wear masks (range, 84 to 88%) [10], while the compliance with face mask guidelines in the Hong Kong Special Administrative Region was 96.6% [11]. The compliance rates with recommendations regarding more frequent hand-washing ranged from 90% to 92% in Bulgaria, Sweden, Finland, and Romania [12].
In a previous study, researchers examined the social determinants of COVID-19 in Massachusetts and found that lower-income communities were at greater risk of experiencing COVID-19 than higher-income communities. However, that study was ecological, so conclusions could not be drawn regarding individual practices [13]. In previous studies conducted in Indonesia, researchers have also examined knowledge, attitudes, and practices related to COVID-19 [3] and hand hygiene behavior [4]. However, those studies only explored a single type of factor, such as predisposing factors, or a single COVID-19 prevention behavior, such as hand hygiene. Therefore, a comprehensive study on the predisposing, enabling, and reinforcing factors associated with COVID-19 prevention behavior is necessary. This study was conducted to identify those factors influencing COVID-19 prevention behavior in the Indonesian community during the COVID-19 pandemic.
METHODS
Study Design
This cross-sectional study used a mixed-methods approach. A sequential explanatory design was carried out by collecting and analyzing quantitative data, followed by qualitative data collection. The qualitative analysis was intended to strengthen and confirm the findings of the quantitative analysis.
Research Participants
The participants were recruited through an online survey between April and July 2021, using a convenience sampling technique. The inclusion criteria were Indonesian citizens at least 18 years of age who voluntarily provided written informed consent. Due to social distancing, study participants were recruited through announcements posted on social media. The minimum sample size was determined as follows:
Based on a previous study, the population proportion 1 (P1) was 0.857, and the population proportion 2 (P2) was 0.143 [14]. Using a significance level of 0.05 and a power of 95%, the minimum sample size was determined to be 243 participants. The actual sample size of this study was 264, which surpassed the sample adequacy requirement.
The qualitative portion of the study was conducted through in-depth interviews with 10 key informants who had previously been involved in quantitative data collection. The criterion for the informants was an understanding of the policies and programs for preventing COVID-19 in the community or institutions, as seen in roles such as head of a neighborhood, head of a hamlet, or member of a COVID emergency response team. Respondents who met these criteria were then listed and randomly selected as informants for the qualitative research.
Research Variables
The independent variables in this study included predisposing factors (knowledge, attitude toward COVID-19 prevention, education level, and socioeconomic level), enabling factors (COVID-19 prevention infrastructure and social support), and reinforcing factors (COVID-19 regulation, punishment, and the involvement of leaders in COVID-19 prevention). The dependent variable was non-compliance with COVID-19 prevention behaviors. Those behaviors consisted of mask-wearing, ensuring hand hygiene through hand-washing with soap or hand sanitizer, maintaining distance, reducing mobility, and avoiding crowds.
Respondents who answered at least 75% of questions correctly were considered to have good knowledge, while a score of less than 75% was considered to indicate poor knowledge. Elementary, middle, and high school levels of education were classified as low-to-medium. The higher education category encompassed all levels of higher education (associate’s, bachelor’s, master’s, and doctoral). Participants were classified into 3 groups by socioeconomic level according to monthly salary: <168 US dollar (USD), 168-505 USD, and >505 USD. According to data from the Indonesian Central Statistics Agency’s national labor force report released in 2022, the national average monthly salary is 2.89 million Indonesia rupiah (approximately 185 USD) [15]. The income cut-off in this study was set at 168 USD because not all respondents in the study were employees. However, the difference between the national income and the income or allowance used in this study was negligible. The study included 3 levels of social support: unsupported, neutral, and supported. The involvement of leaders, COVID-19 regulation, and punishment were categorized as either insufficient or sufficient. The median was used as the cut-off point because the data for attitude, infrastructure, and COVID prevention behavior were not normally distributed. A score of <32 indicated a poor attitude, while a score of ≥32 indicated a good attitude. Poor and good COVID prevention infrastructure were indicated by scores of <8 and ≥8, respectively, while scores of <32 and ≥32 indicated non-compliance and compliance with recommended COVID-19 prevention behavior, respectively.
Study Instruments
Two instruments used in this study were an online quantitative questionnaire and interview guidelines regarding open-ended questions for qualitative studies. The former instrument is a survey of community behavior during the pandemic conducted by the Indonesian Central Statistics Agency [16]. This questionnaire has been updated to reflect the changing situation in Indonesia. In the previous version of the questionnaire, COVID-19 prevention behavior was limited to 4 components: mask-wearing, hand hygiene, social distancing, and avoiding crowds. Following policy changes in Indonesia, an additional recommendation was introduced for COVID-19 prevention: reduced mobility. The questionnaire used in the present study was added to these 5 COVID-19 prevention components, piloted, and validated. The questionnaire was delivered using a Google Form. In the qualitative portion of the research, openended interview guidelines were used, allowing the respondents to be more flexible in expressing their opinions.
Statistical Analysis
The quantitative data analyses were univariate, bivariate, and multivariate. Univariate analysis was attempted to calculate the frequency distribution of each variable. The chi-square test was used for bivariate analysis, which involved creating a 2×2 table between each independent variable and the dependent variable to calculate the prevalence ratio (PR). In a stepwise backward elimination, all variables with p-values less than 0.25 were included. A multivariate logistic regression model was constructed by adjusting for all previously identified covariates from the stepwise backward analysis. A p-value <0.05 was considered to indicate statistical significance. The outcomes of the regression analysis were presented as adjusted PRs with 95% confidence intervals. For the statistical analysis of quantitative data, SPSS version 25 (IBM Corp., Armonk, NY, USA) was used.
Qualitative data analysis was conducted using Atlas.ti version 9 (ATLAS.ti Scientific Software Development GmbH), which is a tool for qualitative research content analysis. The results of the in-depth interviews with informants were transcribed into the Atlas.ti program. The data were identified and grouped using a main code (predisposing, enabling, or reinforcing factor) as well as subcategories (infrastructure, punishment, policy, COVID-19, prevention and control team, and their duties and responsibilities).
Ethics Statement
This study underwent ethical review by the Health Research Ethics Commission of the Health Polytechnic of the Ministry of Health of Malang with the number Reg. No: 071/KEPK-POLKESMA/2021.
RESULTS
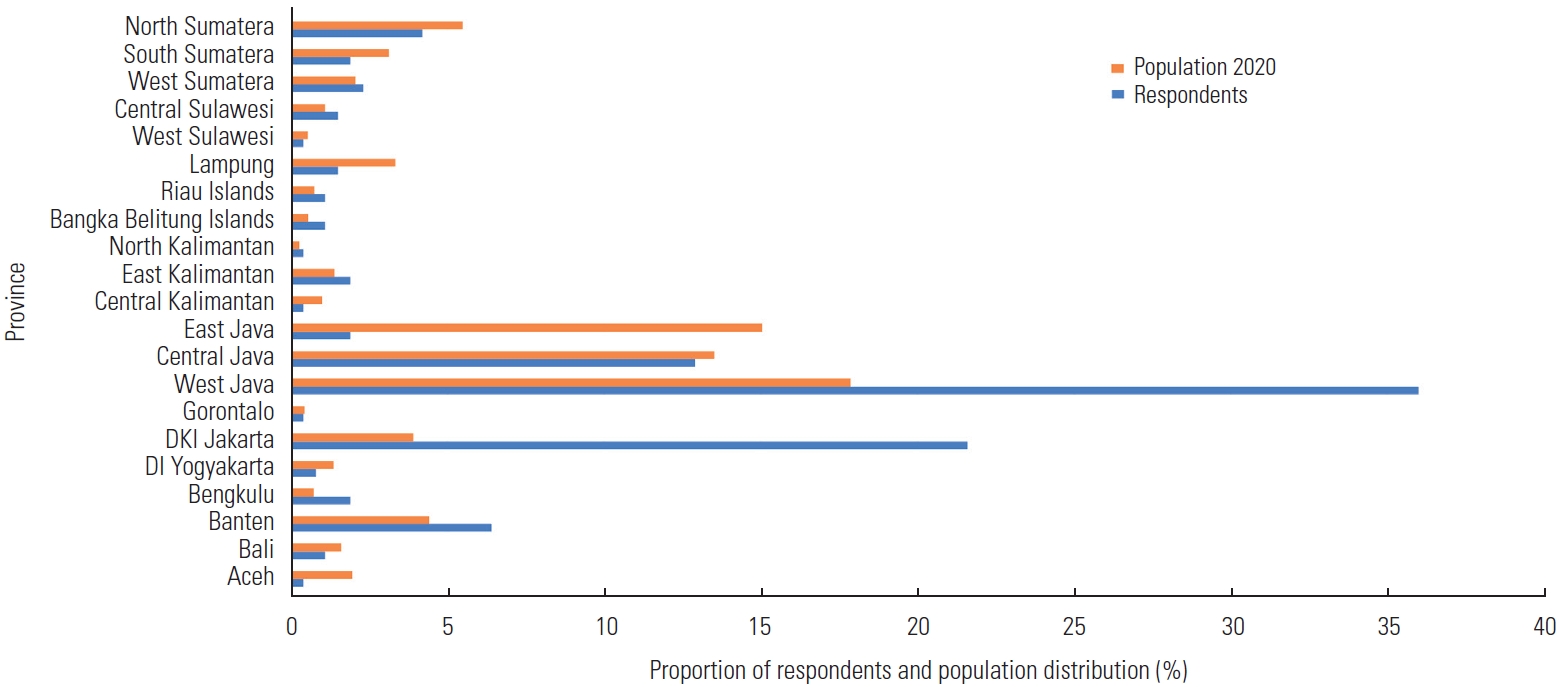
Most participants were from provinces with high rates of COVID-19 cases. The geographical distribution of respondents compared to the population distribution of Indonesia in 2020 is presented in Figure 1. Due to the nature of convenience sampling, the distribution of respondents was not identical to the population distribution. Most respondents were from West Java (36.0%), DKI Jakarta (21.6%), or Central Java (12.9%) (Figure 1).
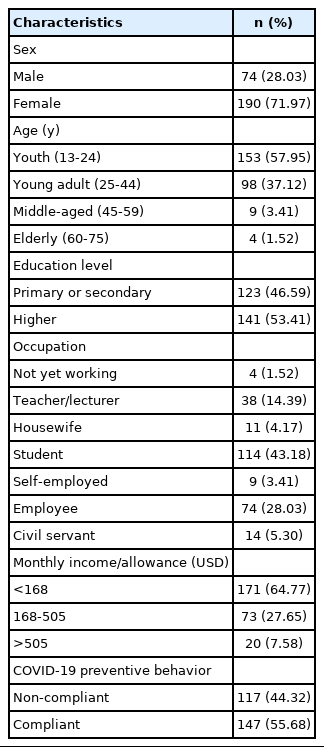
The characteristics of the participants are shown in Table 1. Among the respondents, females (71.97%) predominated over males, and the most common age group was youth (57.95%). The most common reported occupation was college student (43.18%), and most respondents had a low monthly income or allowance (<168 USD; 64.77%).
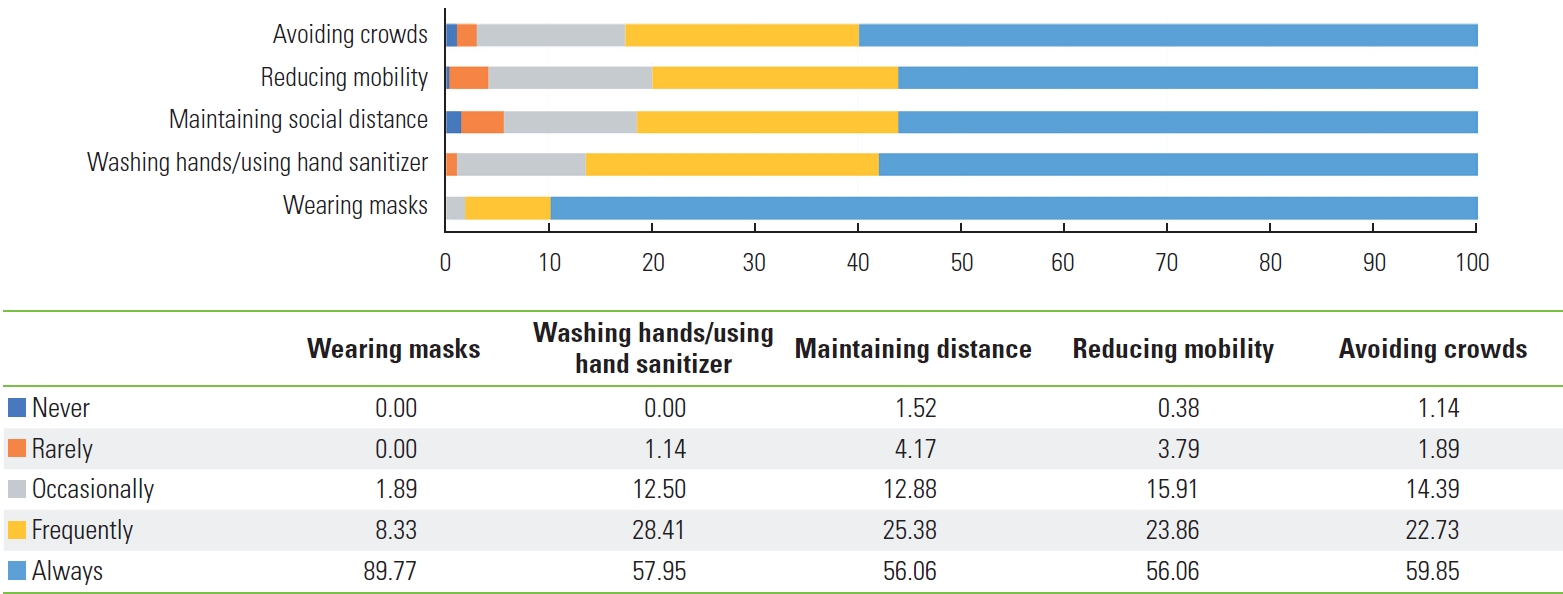
The compliance rates for mask-wearing, hand-washing/using hand sanitizer, maintaining social distance, reducing mobility, and avoiding crowds were 89.77%, 57.95%, 56.06%, 56.06%, and 59.85%, respectively (Figure 2).
Factors associated with non-compliance with COVID-19 prevention behaviors, as determined by the bivariate analysis, are shown in Table 2. Poor attitude, low-to-medium educational level, and middle income were found to be predisposing risk factors for non-compliance. Insufficient infrastructure, inadequate leadership, and insufficient regulation were enabling and reinforcing factors.

Factors associated with non-compliance with COVID-19 prevention behavior in bivariate and multivariate analysis
The results of the multivariate analysis indicated that education level, attitude, leader involvement, and regulation are jointly related to COVID-19 prevention behavior. Respondents with a poor attitude were 25 times more likely to disobey COVID-19 prevention recommendations than those without such an attitude. Insufficient regulation, inadequate involvement of leaders, and low-to-medium education level, respectively, were associated with adjusted PRs of 3.96, 3.67, and 2.14.
Figure 3 shows the results of qualitative data management with the Atlas.ti software. Based on the results of in-depth interviews with informants, predisposing factors related to COVID-19 prevention behavior included the continued presence of many people who did not believe in COVID-19, lacked awareness, lacked knowledge, and/or were indifferent in attitude. An enabling factor for COVID-19 prevention behavior was the availability of infrastructure in the home, office, and public places. Many workplaces provided automatic temperature gauges, hand-washing stations, and touchless elevators. Informants described more reports of positive cases in situations in which the workplace provided social support.
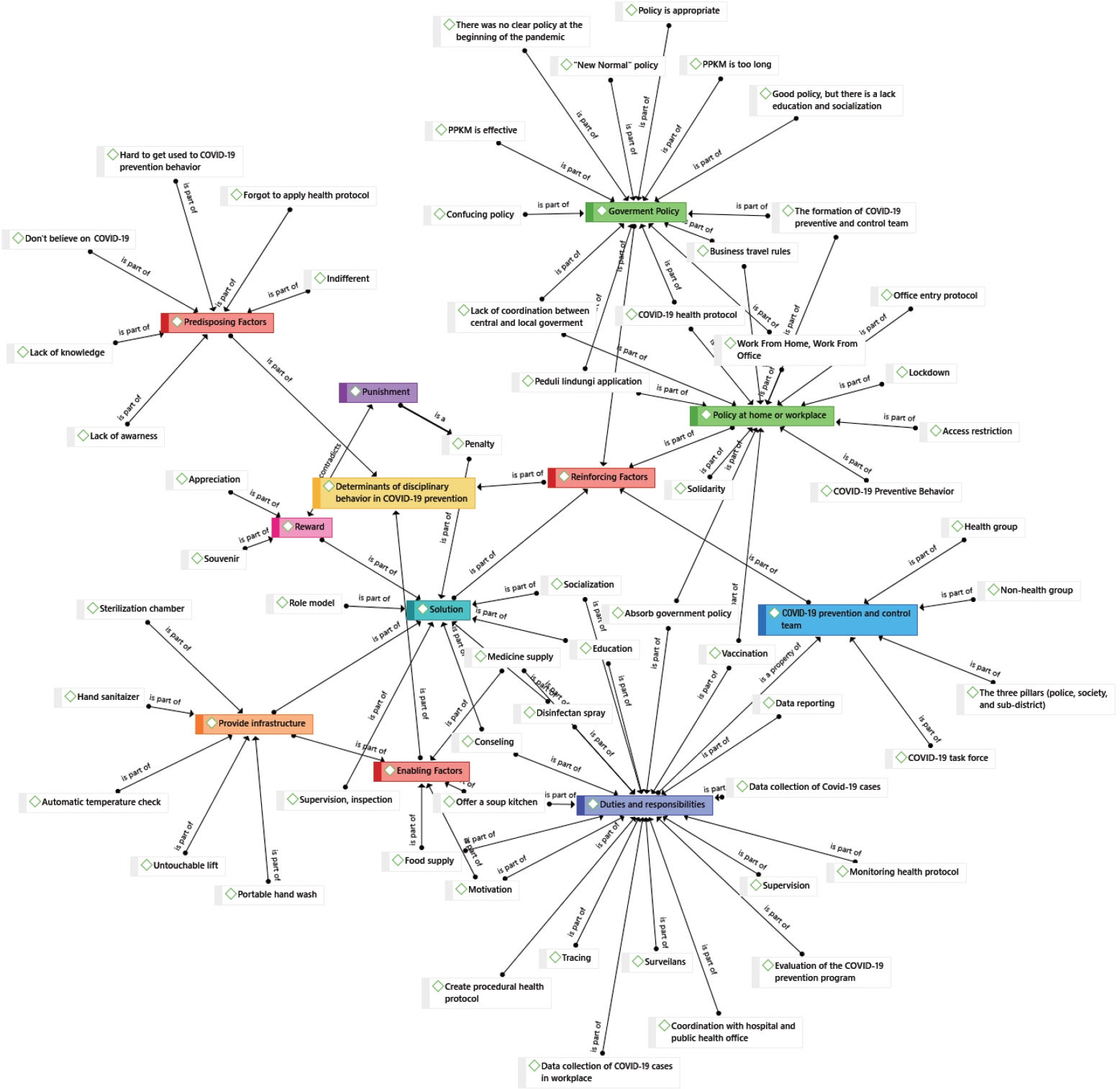
Atlas.ti software for qualitative data management. COVID-19, coronavirus disease 2019; PKKM, Pemberlakuan Pembatasan Kegiatan Masyarakat/Enforcement of Restrictions on Community Activities.
A strong reinforcing factor was the Indonesian government’s policy at the beginning of the pandemic. Overall, the government denied the incidence of COVID-19, causing preventive measures to be enacted too late. In addition, the public witnessed the lack of coordination between the central and regional governments, hindering the lockdown policy early in the pandemic. Over time, many policies have been issued by the Indonesian government to prevent the spread of COVID-19. The Pemberlakuan Pembatasan Kegiatan Masyarakat (PPKM; Enforcement of Restrictions on Community Activities), a COVID management policy in place in Indonesia since the beginning of 2021, has been considered to be appropriate. This conclusion is supported by the decline in COVID-19 cases in September 2021. The Indonesian government has also established the Peduli Lindungi application, a COVID-19 tracking application for digital contact tracing. The government established a COVID-19 task force for each ward and district to cope with the increasing number of confirmed cases. Their tasks were reporting, tracing, and monitoring at the household level and in every workplace.
DISCUSSION
In this study, we elaborated on factors related to compliance with recommended COVID-19 prevention behaviors in Indonesia during the pandemic. Overall, 44.32% of respondents were non-compliant, while the compliance rate with all COVID19 prevention behaviors was 55.68%. In this study, the compliance rates for mask-wearing, hand-washing/using hand sanitizer, maintaining social distance, reducing mobility, and avoiding crowds were 89.77%, 57.95%, 56.06%, 56.06%, and 59.85%, respectively (Figure 2). The results are similar to those of Mukhlis et al. [17] in 2022, who discovered in an Indonesian study that 52.74% of people complied with social distancing standards. The present findings are also consistent with a study conducted in the United Kingdom, where compliance with the use of masks was high (surpassing 75%). In comparison, compliance with hand sanitizer use and social distancing was only around 50% [18].
The predisposing factors for COVID-19 prevention behavior were attitude, education level, and socioeconomic level (Table 2). These factors relate to how people gained information about the virus. In the early pandemic, the government’s negligence, in governing as if COVID-19 would not reach Indonesia, may have led to low awareness among citizens about the existence of the disease. Thus, their attitudes toward complying with preventive recommendations were also poor. This result is consistent with several studies indicating that subjective attitudes and norms significantly impact the adoption of preventive behavior [19,20]. Positive attitudes toward COVID-19 prevention behaviors could reduce the potential risk of the disease [21].
Only those who could access more comprehensive information, such as well-educated people with higher incomes, could make judgments on countermeasures for their families and provide COVID-19 prevention equipment. Additionally, the present findings aligned with a previous study positing that good knowledge does not necessarily determine good behavior; this is because adaptive behavior requires several stages, from awareness-raising to behavior adoption [3]. In this study, most respondents exhibited good knowledge about COVID-19, including its causes, modes of transmission, symptoms, and prevention. However, the association with the dependent variable was insignificant. The findings aligned with a previous study [22]. Income earned during the implementation of social restrictions could influence COVID-19 prevention and stay-at-home behaviors [23]. Undeniably, the implementation of COVID-19 prevention behaviors carries extra expenditures that constitute an additional cost to a household, especially for those with irregular income. The study also noted that a shortage of masks and hand sanitizers occurred due to a monopoly of many irresponsible actors, resulting in a significant increase in prices. Therefore, people in higher socioeconomic levels would have found it easier to access COVID-19 prevention tools.
In this study, poor infrastructure was associated with an increased risk of non-compliance with COVID-19 prevention behaviors. Even before the pandemic, Indonesia faced challenges such as urban density, poor hand-washing habits, poor access to clean drinking water, and limited personal protective equipment [24]. Water and soap can be used to effectively eliminate viruses and bacteria and thus prevent hand-to-hand transmission [25], so poor access to safe water could increase the risk of COVID-19 and other infectious diseases [26]. According to key informants, each household had provided hand-washing facilities in the home. In public places, the installation of simple touchless hand-washing stations had also begun.
Although the multivariate analysis showed that social support was not related to COVID-19 prevention behavior, the results of the qualitative analysis indicated the opposite: that social support was critical to the reporting of COVID-19 cases. People are often reluctant to report positive cases because they fear being shunned by their neighbors and friends if they are found to be positive. Therefore, social support indirectly determines behavior around COVID-19 prevention [27].
The inadequacy of COVID-19 prevention regulations and the insufficient involvement of leaders encourage people to disobey COVID-19 prevention guidelines. The findings of this study are consistent with others showing that the role of leaders influences COVID-19 prevention [28]. Furthermore, leaders must develop the courage to rapidly change course on health policy if necessary to prevent the spread of COVID-19 [29]. When encouraging people to follow public health regulations, as is recommended to slow the spread of SARS-CoV-2, trust in government organizations is crucial [30].
The results of the qualitative data analysis highlight the policies issued by the Indonesian government at the beginning of the COVID-19 pandemic. When the first COVID-19 case was announced in Wuhan, China, the Indonesian government did not enact preventive measures such as restricting access to high-risk countries. Even though border shutdowns could significantly reduce the spread of the virus causing COVID-19 [31], some policymakers were in denial and thought that Indonesia would not experience COVID-19 cases. The qualitative research findings show that the government initially tended to deny the existence of COVID-19, which obstructed prevention efforts. This is consistent with quantitative research showing that a lack of leadership influences COVID-19 prevention behaviors. Attitudes toward political institutions can influence how society processes information. Lack of trust could lead to refusal from the community to comply with future policies, thus causing increased difficulty controlling the disease [32].
Until the first COVID-19 case in Indonesia was announced in March 2020, no proper coordination was occurring between the central and local governments. Thus, the lockdown policy was suboptimal. The timing of the lockdown orders was significantly associated with the spread of COVID-19 after adjusting for various socio-demographic, geographic, and health-related factors [33]. Over time, many policies have been issued by the government to prevent the spread. One example, PPKM, was considered appropriate to combat COVID-19, which was supported by the declining number of positive confirmed cases. Social distancing interventions significantly decrease the rate of COVID-19 by reducing human mobility and thereby preventing large numbers of people from being infected. Community mobility data obtained through cell phones is a potential reference for policymakers [34]. The Peduli Lindungi mobile app, a COVID-19 tracking application, has been officially used for digital contact tracing in Indonesia.
This study provides comprehensive information on several factors (including predisposing, enabling, and reinforcing factors) related to COVID-19 prevention behavior in Indonesia. The mixed-methods design may also have enhanced the reliability and validity, as the findings could complement each other. In this study, we also provide recommendations for improving adherence to COVID-19 prevention recommendations. However, the data collection in this study was conducted using an online platform and was therefore only accessible to those with Internet access. This limited the distribution of respondents. We attempted to approximate the actual proportion of respondents based on province. Separately, this study is limited by its cross-sectional nature. Furthermore, because it involved a mixed-methods approach with a sequential explanatory strategy, in which qualitative analysis was intended to strengthen and confirm the findings of the quantitative analysis, there was a relative paucity of qualitative findings.
In conclusion, 44.32% of participants were found to be non-compliant with recommended COVID-19 prevention behaviors. The predisposing factors related to COVID-19 prevention behaviors are attitude, education, and socioeconomic level. The enabling factor is infrastructure, while reinforcing factors include the role of leaders and regulation. According to the multivariate analysis, attitude, regulation, the role of leaders, and education level are jointly related to COVID-19 prevention behavior. The qualitative portion of the research highlights government policies in dealing with COVID-19. These findings emphasize the urgent need to increase public awareness about COVID-19 by encouraging voluntary community participation through active risk communication and thus facilitate positive changes in behavior. Furthermore, this effort must be supported by COVID-19 prevention regulations, and leaders must be role models in COVID-19 prevention. Finally, the Indonesian government must be more responsive in dealing with the COVID-19 pandemic.
Notes
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
FUNDING
Funding was provided by the Ministry of Research and Technology of the Republic of Indonesia (RISTEK-BRIN).
AUTHOR CONTRIBUTIONS
Conceptualization: Lestari PW. Data curation: Lestari PW, Dewi GK. Funding acquisition: Lestari PW. Writing – original draft: Lestari PW. Writing – review & editing: Lestari PW, Agestika L, Dewi GK.
ACKNOWLEDGEMENTS
We would like to thank everyone who helped with this research, as well as the research participants and the Binawan University research and community service institute.