A Peer-support Mini-counseling Model to Improve Treatment in HIV-positive Pregnant Women in Kupang City, East Nusa Tenggara, Indonesia
Article information
Abstract
Objectives
Low adherence to antiretroviral (ARV) therapy in pregnant women with human immunodeficiency virus (HIV) increases the risk of virus transmission from mother to newborn. Increasing mothers’ knowledge and motivation to access treatment has been identified as a critical factor in prevention. Therefore, this research aimed to explore barriers and enablers in accessing HIV care and treatment services.
Methods
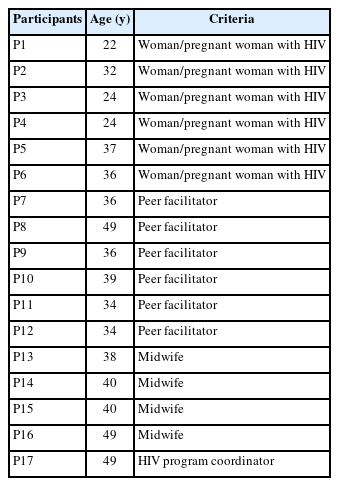
This research was the first phase of a mixed-method analysis conducted in Kupang, a remote city in East Nusa Tenggara Province, Indonesia. Samples were taken by purposive sampling of 17 people interviewed, consisting of 6 mothers with HIV, 5 peer facilitators, and 6 health workers. Data were collected through semi-structured interviews, focus group discussions, observations, and document review. Inductive thematic analysis was also performed. The existing data were grouped into several themes, then relationships and linkages were drawn from each group of informants.
Results
Barriers to accessing care and treatment were lack of knowledge about the benefits of ARV; stigma from within and the surrounding environment; difficulty in accessing services due to distance, time, and cost; completeness of administration; drugs’ side effects; and the quality of health workers and HIV services.
Conclusions
There was a need for a structured and integrated model of peer support to improve ARV uptake and treatment in pregnant women with HIV. This research identified needs including mini-counseling sessions designed to address psychosocial barriers as an integrated approach to support antenatal care that can effectively assist HIV-positive pregnant women in improving treatment adherence.
INTRODUCTION
Indonesia faces a significant human immunodeficiency virus (HIV) epidemic, with an estimated 526 841 people living with the virus in 2022. Nationally, testing coverage among key populations has reached 77%; however, treatment and viral suppression are still lagging, as only 40% of people with HIV are receiving treatment and 16% have achieved viral suppression [1]. The prevalence in the age group over 15 years was 0.3% (key populations), except for Papua and West Papua, at 2.3% in the general population. The National Strategic Plan on HIV and sexually transmitted infections (STIs) 2020-2024 has clearly set targets and focused interventions in line with the global goal of ending acquired immune deficiency syndrome (AIDS) by 2030. The targets are reducing new HIV infections, increasing access to HIV testing and treatment, reducing HIVrelated deaths, and reducing stigma and discrimination. The national HIV and STI prevention and control program is supported by the national and sub-national health budget, as well as international donors and private sectors. Annually, an estimated US$160-180 million is needed to finance this program [2,3].
In Indonesia, the prevalence of HIV infection in pregnant women was estimated at 0.3%; there are more than 5 million pregnant women every year; hence, around 12 000-15 000 babies are born to infected mothers in Indonesia [4]. Relevant HIV and AIDS prevention efforts have been integrated into the national health framework. The program is known as prevention of mother-to-child transmission (PMTCT). Compared to other countries in the region, Indonesia is the only country with an increasing number of new cases in newborns. Integration of HIV and syphilis testing as part of routine antenatal care only started in 2015; this was further expanded to include hepatitis B screening in what later became known as the triple elimination program. Testing for HIV, syphilis, and hepatitis B is provided by the government and can be obtained free of charge. National HIV AIDS Information System data from 2017-2020 showed that the number of HIV tests in pregnant women has increased. The United Nations Children’s Fund (UNICEF) report from 2021 indicated that the increase in those receiving antiretroviral (ARV) treatment did not match the number of tests available. The testing coverage increased 8-fold, from 6% in 2014 to 48% in 2020, while treatment coverage only increased 5-fold, from 6% to 33% in the same period [5-7].
The same situation is also experienced in East Nusa Tenggara, 1 province of the 5 provinces with the lowest coverage of HIV testing and ARV treatment based on the 2018 national evaluation of the PMTCT. Data from the Kupang City Health Office for 2020 indicate that, every year, 6154 pregnant women were tested for HIV, with a prevalence of 0.28-0.30%, according to which there were 15-18 infected pregnant women [2,5]. Furthermore, Ministry of Health data reported that, out of 22 districts and cities in East Nusa Tenggara, only 14 had reported HIV testing and ARV treatment. The coverage in Kupang City reached 70%, but the treatment rate was still very low (at 19%). Therefore, HIV treatment in pregnant women is still a major obstacle for the prevention program.
A literature review showed that many factors influence the likelihood that pregnant women with HIV receive proper ARV treatment. Kalungwe et al. [8] showed that, in Africa, factors related to side effects and financial constraints in accessing food, transportation, and medicines influenced adherence to ARV treatment. Other factors included culture, religion, lack of partner support, stigma, and discrimination.
Lumbantoruan et al. [9] showed that the factors motivating pregnant women to participate in the PMTCT program and adhere to treatment were high-quality post-HIV testing counseling and a belief in the beneficial effects of drugs. Doubts about the benefits of treatment, the existence of partners who forbade treatment, and fears of stigma and discrimination in the family or society were the main obstacles. Ahmed et al. [10] stated that in several developing countries, infected people refused to start ARV treatment to prevent status disclosure and avoid stigma or rejection by partners, family, and society.
Several countries, specifically in Africa, have developed assistance or community empowerment models by involving lay officers, HIV communities (non-governmental organizations), and pregnant women with HIV to strengthen PMTCT programs [11-14]. The results of a trial conducted by UNICEF in 2019 considering the assistance model in 4 cities showed that almost all HIV-positive pregnant women regularly received ARV drugs. Furthermore, about 97% of babies were not infected after viral load testing at 18 months old, according to the standard of early diagnosis or early infant diagnosis [7]. These results demonstrate that with good support, pregnant women can adhere to HIV care and treatment. This has opened up opportunities to study more deeply the challenges and supporting factors encountered from the perspectives of the various parties directly involved in the services. Therefore, in this study, we explored the challenges associated with accessing HIV care and treatment services, as well as the roles of peer facilitators in Kupang City.
METHODS
This research was a qualitative descriptive-thematic inductive analysis [15] conducted in Kupang City, East Nusa Tenggara, Indonesia, from May 2022 to June 2022.
Research Design
This research used a qualitative approach to deeply explore pregnant women’s challenges in accessing HIV services and the role of peer facilitators in providing support. The data were collected from health workers and patients of four public health centers (puskesmas) in the Kupang City area, namely Puskesmas Bakunase, Puskesmas Oesapa, Puskesmas Oepoi, and Puskesmas Naeoni, representing 11 puskesmas in Kupang City. The interview instrument consisted of several open-ended questions developed with a structured sequence. Psychological and social issues related to maintaining adherence to ARV were investigated, along with the respective responsibilities of peer facilitators and service workers.
Research Participants
Qualitative research methods were used to generate detailed descriptions of the experiences of participants living with HIV and providing services related to HIV. Data collection was conducted using in-depth interviews (IDIs) and focus group discussion (FGDs), and all the sessions were audio-recorded. Both IDIs and FGDs were used to triangulate information obtained from the participants. Resource persons included mothers/ women with HIV, health workers and peer facilitators. We interviewed 17 participants, who consisted of 6 pregnant women/women with HIV, 6 peer facilitators, and 5 health workers (midwives and the person in charge of the HIV program at the Community Health Centers). We also conducted 2 FGDs for peer facilitators and pregnant women/women with HIV, with a total of 11 participants. The recruited participants were between 22 years old to 54 years old. The exclusion criteria were pregnant women with non-reactive HIV test results and pregnant women with HIV who refused to take part in the research.
To maintain the confidentiality of the participants, the researchers gave the informant code 01 for pregnant women/ women with HIV, 02 for health workers, and 03 for peer facilitators. A personal code was added with 2 letters from participant’s name that were chosen by the participant. For example, “01-WM01DD” denoted an IDI with pregnant women/women with HIV no.1, where DD is 2 letters from the participant’s name and the person is the first interviewee.
Statistical Analysis
The interviewers in this study were 3 people, consisting of 1 expert in HIV and qualitative research, 1 epidemiologist, and 1 qualitative research expert. All interviewers had experience in conducting qualitative research.
The interviews and FGDs were recorded using a digital audio recorder. The audio recording files were transcribed to directly obtain information on important issues. The interviewer took notes during the interview process. This process is useful for cross-checking information obtained from the transcribed interviews and FGDs with the researchers’ field notes. The transcription of IDIs and FGDs became the source of information for the qualitative data analysis, which was based on the themes that were developed based on the interview guide or FGD.
Data processing was performed based on the interview transcripts and FGDs from the recordings of the interview process. The descriptions or notes obtained were refined and completed as a single written transcript. The analysis was performed by grouping the results based on the available themes. Meanwhile, the grouped themes were interpreted, and conclusions were derived for each topic.
Ethics Statement
This research received ethical approval from the Udayana University Ethics Commission (No. 1152/UN14.2.2.VII.14/LT/2022). The participants gave written consent regarding their willingness to become respondents. Interviews and FGDs were conducted at a convenient time and place agreed upon by the informants, such as in the workroom, the interviewee’s house, and a private meeting room.
RESULTS
Results were obtained by analyzing the information obtained from 17 respondents, who comprised 6 mothers who were PMTCT patients, 6 peer facilitators, and 5 health workers who were midwives and HIV program coordinators, aged 22-36 years, 34-49 years, and 38-49 years, respectively. Table 1 shows the characteristics of the participants.
Stigma Related to HIV/AIDS
Mothers with HIV experienced stigma from the family and community in the neighborhood and health workers who provided health services. The followings are some quotes from respondents who amplified this statement.
“.... But what occurred, ma’am? You are given a sign when you receive a pink book (F: MCH Book). Later, it is for people who wish to procreate. However, there is a red highlight on B20.” (Interview, facilitator)
“…then there was a patient I assisted. She had a severe sexually transmitted infection (STI) and was about to give birth, her husband was in a seriously bad condition and in the ER. The nurses had to insert the medicine vaginally, but she did not want to provide that service; hence, we were asked to help put medicine in her genitals.” (FGD, facilitator)
Difficulty in Accessing Services (Time, Cost, and Distance)
Time constraints, financial constraints, and travel time to and from the hospital all contribute to service inaccessibility.
“...cost constraints...also, because I work, it is sometimes difficult to travel, my husband drops (taxi-bike) people here and there... we do not have time, we are lazy, and we want to take medicine (puskesmas)....” (Interview, pregnant woman with HIV)
“...they do not take medicine because of the husbands’ prohibition. …when the husbands do not give [them] money, where do they want to go...” (FGD, facilitator)
Drug Side Effects
Some of the side effects of taking ARV medications were also noted by several sources, including hair loss, fever, nausea, blackened burn-like areas on the skin, skin numbness, and menstrual disorders.
“…At first, my hair often fell out, but the longer it went on, the more I became immune. Only after taking the drug did my skin become darker.” (Interview, woman with HIV)
“…Taking one pill is very dizzying... but it is safe. Maybe the first time, I will repeat it, take it again... (one-time medicine), and when I feel dizzy, nauseous, vomit... I want to take one...” (Interview, pregnant woman with HIV)
Administrative Requirements to Access Human Immunodeficiency Virus Services
The administrative requirements needed are an ID card (Kartu Tanda Penduduk/KTP), a family card (Kartu Keluarga), and a universal health insurance (BPJS) card. The 3 groups of informants acknowledged that the existence of BPJS was very helpful in obtaining access to free treatment (ARV drugs). However, some patients did not have a BPJS card because they did not have an ID or family card due to their marital status.
“…KTP is also available, but for example, there is only an ID card, but there is no BPJS, hence, they automatically enter as general and paid patients, but most of them here are housewives, farmers, and do not have any money... after giving birth, the child will also disappear, right,” (FGD, facilitator)
Knowledge of Antiretroviral Treatment Benefits
One of the informants stated that their greatest motivation for taking medicine was the hope of being cured. Research has shown that after taking regular medication for six months, viral load tests are no longer be able to detect the virus in the blood. This status is known as “undetectable and un-transmittable.” Apart from that, another motivation was the desire to keep their children healthy and to prove that people with HIV can still work, be productive, and be of benefit to others. The following are some statements from the interviews and FGDs (mothers with HIV and facilitators).
“.. As far as I can tell, the drive to be healthy is the children, even though their husbands do not support them, they comply with taking medication because of the children. Therefore, it is just fine for them to get sick rather than the children….” (FGD, facilitator)
“…because I want to show people who stigmatize me… I was told that I only had 10 months to live. Even if I was still alive, I would not be able to remarry and have another child. That said made me struggle to get up again... because of that, I struggled to give birth again.” (FGD, woman with HIV)
Lack of Staff Training and Limited Knowledge of the Prevention of Mother-to-Child Transmission Program
From the opinions of health workers, the knowledge and skills in handling pregnant patients with HIV were uneven, specifically those with psychological problems.
“…so, I do not have much knowledge and experience. Therefore, I hope there will be training, refreshment... for the PMTCT. To explain to patients, much knowledge is needed.” (Interview, health worker)
“...In my opinion, what we have now is not enough, ma’am, because there is no special leaflet about PMTCT at puskesmas; at least, we only give a standard explanation.…” (Interview, health worker)
Role of Peer Facilitators
Facilitators are very important in helping people with HIV accept their status and access available services. They assist mothers in understanding the virus, help them access treatment services at hospitals, accompany and introduce them to procedures at hospitals, inform partners about their status and invite partners to take HIV tests, assist with BPJS arrangements, and provide motivation to keep enthusiasm for life. The followings are some of the informants’ statements that support the above description.
“Those who consistently give me spirit. Similarly, when I am ill, sometimes medicine is brought by a companion. They also like to come, visit us, ask how things are going, and are always upbeat... Do not worry about what others say, they were even present when I gave birth.” (Interview, health worker)
“…Every time nurses receive updates; they ask us to take care of them. Furthermore, when there is a consultation, we will take them to this polyclinic. We are entrusted to take clients to the polyclinic.” (FGD, facilitator)
“….At the health center, they help to find counters, and the facilitator acts as a health worker, in the hospital. They also know the flow in the hospital; hence, when friends ask questions, the reply is, “oh yes, you use BPJS, it means the process involves going here first and then there” (Interview, health worker)
The challenges in implementing the PMTCT program are grouped from the perspective of pregnant women with HIV, peer facilitators, and health workers, as seen in Figure 1 below.

Key challenges in the PMTCT program from the perspectives of patients with HIV, peer facilitators, and health workers. PMTCT, prevention of mother-to-child transmission; HIV, human immunodeficiency virus; ARV, antiretroviral; IEC, information, education and communication.
The challenges in accessing HIV care and treatment include stigma, difficulties in accessing services related to distance, time, costs and administrative requirements, drug side effects, quality of health workers and services provided, and knowledge about ARV benefits. The point was raised during the focus group discussion that some of the participants had to budget for an additional expenditure (up to Indonesian rupiah [IDR] 50 000 or US$3) to go to the hospital to get treatment since the nearest primary health centers could only conduct testing. Thus, some of the pregnant women may not yet be registered with the national health scheme, meaning that they will be required to pay IDR 50 000 to IDR 75 000 (equivalent to US$3-5) as administration fees to receive ARV drugs, which is the same amount that they need for daily consumption (of a family of 4 household) in Kupang City [16].
Some of these key problems were also identified by two or all groups of participants. The challenges related to skills and knowledge were stated by peer facilitators and health workers. Meanwhile, those concerning the fulfillment of administrative requirements to access free treatment were specified by all groups. Long and complex procedures in accessing hospital services were identified as key challenges by pregnant women with HIV and peer facilitators.
DISCUSSION
Health services for preventing HIV transmission from mothers to children (the PMTCT program) have been implemented at primary and secondary healthcare facilities. Even though the implementation is available at all primary health services in Kupang City, access to treatment services is still low [17]. Challenges can relate to mothers or health services (i.e., human resources and the availability of services). Therefore, peer facilitators play an urgently needed role in helping pregnant women with HIV overcome difficulties.
The results are in line with several previous studies regarding challenges in accessing HIV services [18-21]. Ogueji and Omotoso [22] and Ntsime et al. [23] found 5 challenges in using PMTCT services—namely, stigma, lack of family support, financial problems, time and costs, and poor health service facilities. Onono et al. [24], in a study in western Kenya, reported that the social environment influenced whether mothers with HIV accessed services. Mothers in unfavorable environments were more likely to have babies infected with HIV compared to those living in favorable surroundings.
To further assist HIV-positive mothers, peer facilitators pay regular visits, encourage them to keep taking ARVs, and track their progress. Motivation needs to be routinely given to ensure that they continue to undergo treatment and care according to standards during pregnancy, preventing transmission of the virus. After delivery, peer facilitators support mothers by providing ARV and prophylaxis. Early infant diagnosis is also undertaken at 4-6 weeks to detect infected infants.
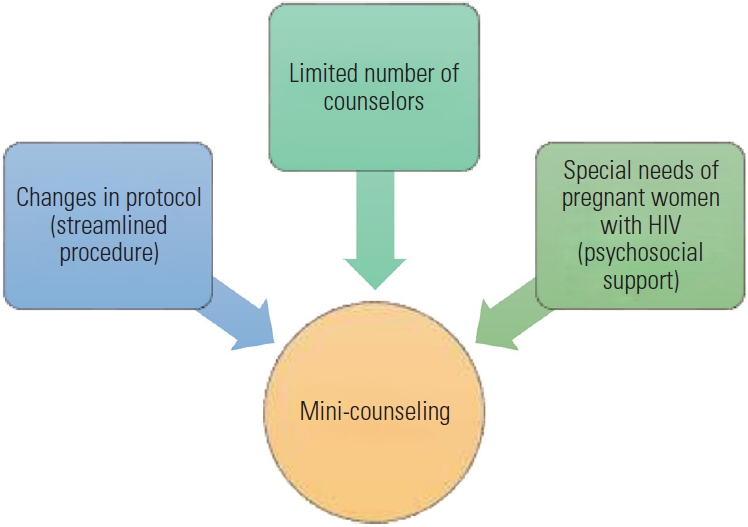
Psychosocial support includes sharing experiences and motivating each other, while emotional support enables mothers to identify their strengths and build positive knowledge about the benefits of ARV treatment. This research identified several psychosocial barriers or issues often experienced, such as resistance to accepting HIV status, fear of disclosing the status to their partners, family, or friends, fear of experiencing the side effects of ARV treatment, and other negative thoughts about the disease due to lack of knowledge (Figure 2). Furthermore, counseling after the diagnosis was considered inadequate, as mothers were only counseled once. The test-and-treat strategy, where treatment is immediately given following diagnosis, was started in 2019. This was conducted without proper counseling sessions. It has negative implications, as pregnant women may not be ready to accept their status, or more time and counseling sessions may be needed to ensure their receptivity, motivation, and commitment to treatment.

Factors influencing individuals’ knowledge, perception, acceptance, and motivation to adhere to human immunodeficiency virus (HIV) treatment.
DiCarlo et al. [25] showed that lay health workers played a critical role in supporting mothers with HIV across a range of behavioral, social, and structural domains of PMTCT services. This included improved communication and contact, health education, peer support, and patient advocacy and assistance. This research identified similar barriers to the uptake and implementation of PMTCT, such as concerns about privacy and stigma, as well as the limitations of the healthcare system, including workers’ attitudes. Another study by Peltzer et al. [26] highlighted the importance of identifying patients with adherence problems and offering additional treatment support. That research used lay health workers who provided structured group adherence to support mothers who were experiencing problems adhering to ARV treatment. Workers, as lay counselors, can enhance knowledge relevant to adherence by aiming to intensify support to treatment with at least 3 group sessions.
Our previous study also showed that HIV-positive pregnant women who did not receive assistance from peer facilitators were 2.96 times more likely not to utilize health services than those who received assistance [23]. Thus, this qualitative research showed the need for more counseling sessions as part of the peer support model and integrating with the antenatal care schedule. It emphasized the importance of mentoring to assist mothers with HIV to maintain adherence to treatment [27-30]. Peer facilitators’ assistance should be structured more systematically and comprehensively, addressing the psychosocial barriers identified and designed to fit the needs and conditions of pregnant women with HIV. The strategy for reducing these barriers should include the provision of assistance by peer counselors through mini-counseling embedded as part of antenatal care visits. It is necessary to provide health education ensuring that pregnant women fully understand the risk of HIV transmission from mother to child and the importance of ARV treatment to prevent vertical transmission. In addition, motivational support given by the peer group and support from partners, family, and the environment are needed to help pregnant women with HIV adhere to treatment [31]. These processes can be conducted through mini-counseling in which peer facilitators act as lay counselors. The mini-counseling sessions will discuss internal and external factors hindering mothers from accessing services, personal strengths and social support, motivation to continue taking ARV, and self-appreciation for success in overcoming difficulties (Figure 3). The activity should also be integrated into HIV-related care and treatment programs conducted by health services. This shows a clear division of roles, and synergistic coordination can be conducted to meet the needs of pregnant women. Therefore, the goals of the PMTCT program to improve the quality of life of HIV mothers and have healthy children can be achieved [32].
Notes
DATA AVAILABILITY
The data that support the findings of this study are available from the corresponding author, AC, upon reasonable request.
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
FUNDING
This research received funding from UNICEF Indonesia.
AUTHOR CONTRIBUTIONS
Conceptualization: Camellia A, Swandari P, Rahma G. Data curation: Camellia A, Swandari P, Rahma G. Formal analysis: Camellia A, Swandari P, Rahma G, Merati TP. Funding acquisition: Camellia A. Methodology: Camellia A, Rahma G, Merati TP, Bakta IM, Duarsa DP. Project administration: Camellia A, Merati TP. Visualization: Camellia A, Rahma G. Writing – original draft: Camellia A, Swandari P, Rahma G. Writing – review & editing: Camellia A, Swandari P, Rahma G, Merati TP, Bakta IM, Duarsa DP.
ACKNOWLEDGEMENTS
This research is part of a mixed-method analysis to develop a model of community support to improve the uptake of antiretroviral therapy in pregnant women with HIV and part of a doctoral dissertation program in Public Health, Faculty of Medicine, Udayana University, Denpasar. The authors are grateful to the respondents, UNICEF Kupang, the Indonesian Midwives Association (IBI) Kupang, Kupang City Health Office and the Flobamora Foundation, the Indonesian Positive Women Association (IPPI) Kupang who supported this research, and UNICEF, which provided research funding.
Facts and opinions presented in this article are solely the personal statements of the authors and do not represent the affiliated organization.