Sleep Quality and Poor Sleep-related Factors Among Healthcare Workers During the COVID-19 Pandemic in Vietnam
Article information
Abstract
Objectives
The coronavirus disease 2019 (COVID-19) pandemic has increased the workload of healthcare workers (HCWs), impacting their health. This study aimed to assess sleep quality using the Pittsburgh Sleep Quality Index (PSQI) and identify factors associated with poor sleep among HCWs in Vietnam during the COVID-19 pandemic.
Methods
In this cross-sectional study, 1000 frontline HCWs were recruited from various healthcare facilities in Vietnam between October 2021 and November 2021. Data were collected using a 3-part self-administered questionnaire, which covered demographics, sleep quality, and factors related to poor sleep. Poor sleep quality was defined as a total PSQI score of 5 or higher.
Results
Participants’ mean age was 33.20±6.81 years (range, 20.0–61.0), and 63.0% were women. The median work experience was 8.54±6.30 years. Approximately 6.3% had chronic comorbidities, such as hypertension and diabetes mellitus. About 59.5% were directly responsible for patient care and treatment, while 7.1% worked in tracing and sampling. A total of 73.8% reported poor sleep quality. Multivariate logistic regression revealed significant associations between poor sleep quality and the presence of chronic comorbidities (odds ratio [OR], 2.34; 95% confidence interval [CI], 1.17 to 5.24), being a frontline HCW directly involved in patient care and treatment (OR, 1.59; 95% CI, 1.16 to 2.16), increased working hours (OR, 1.84; 95% CI,1.37 to 2.48), and a higher frequency of encountering critically ill and dying patients (OR, 1.42; 95% CI, 1.03 to 1.95).
Conclusions
The high prevalence of poor sleep among HCWs in Vietnam during the COVID-19 pandemic was similar to that in other countries. Working conditions should be adjusted to improve sleep quality among this population.
INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic has had a significant impact on countries around the world, including Vietnam. At the time this study was conducted (October to November 2021), Vietnam had not yet achieved widespread vaccination and was grappling with the fourth and most severe wave of the outbreak. During this fourth wave, Vietnam saw a substantial increase in confirmed COVID-19 cases, with over 1 232 852 new cases reported and 25 252 deaths [1]. This surge in cases placed a heavy burden on the healthcare system and healthcare workers (HCWs) who were on the frontlines of combating the pandemic.
The HCWs in the COVID-19 pandemic, involved in the COVID-19 pandemic, including doctors, nurses, and laboratory technicians, are professionals whose duties related to human health often involve long working hours and night shifts [2,3]. During the pandemic, HCWs have reported caring for a significantly larger number of patients than usual, with some indicating that they cared for up to 4 times their typical patient load over an extended period [4]. This has placed immense strain on healthcare systems, resulting in increased workloads and a decline in the quality of care. As the pandemic persists, HCWs must also attend to patients with various other health conditions, further adding to their already heavy workload. Consequently, several indirect effects have emerged among HCWs, such as heightened stress, anxiety, and sleep-related issues.
During the COVID-19 pandemic, HCWs have increasingly experienced sleep-related problems, such as sleep disorders that affect sleep quality. Some studies have indicated that the prevalence of sleep disorders ranges from 43.9% to 78.8% [5–7]. A study conducted in Norway found that changes in work schedules during the pandemic were associated with poorer sleep quality, decreased sleep duration, and higher turnover intention among nurses. Specifically, an increase in quick returns (i.e., 11 hours or less between 2 consecutive shifts) and long workdays (>8 hours) were associated with worse sleep quality and higher turnover intention [8]. Factors contributing to reduced sleep quality include prolonged working hours, excessive workload in limited work conditions, shortage of human resources, lack of supporting machinery, inadequate personal protective equipment, and sleep deprivation [9–13].
A decline in sleep quality can result in physical issues, such as fatigue and exhaustion, as well as psychological problems, including increased irritability and lack of concentration. These issues can impair communication and coordination among HCWs [7,14,15]. As a result, it is crucial to examine sleep quality and its associated factors among HCWs in various locations to mitigate the consequences of sleep disorders and medical errors [16]. Currently, studies on sleep quality among HCWs in Vietnam during the COVID-19 pandemic are quite limited and small in scale. Therefore, it is critical to investigate the quality of sleep and its related factors among HCWs in different locations to reduce its consequences in sleep disorders and medical errors. Presently, studies in Vietnam on sleep quality in HCWs during the COVID-19 pandemic are fairly limited and on a small scale [17]. Therefore, a large-scale study to assess the sleep quality of HCWs is necessary. Consequently, we conducted this research to evaluate sleep status during the pandemic among HCWs in Vietnam, and we anticipate that our findings will help provide valuable evidence to improve the physical and mental health of HCWs and enhance healthcare performance.
METHODS
Study Design and Sampling
We carried out a cross-sectional study utilizing an online questionnaire from October 2021 to November 2021. Throughout this time frame, an average of 7821 cases were documented daily [18]. Data were gathered from 1000 HCWs involved in the COVID-19 pandemic across 3 regions of Vietnam (southern, central, and northern Vietnam).
Data Collection and Measurements
HCWs were randomly chosen based on a list maintained by the provincial health department. Subsequently, a link to the questionnaire was sent to each individual’s provided email address. The structured questionnaire aimed to gather information on personal characteristics, work-related attributes, alterations in work situations before and during the pandemic, and sleep quality.
Independent variables
The socioeconomic data collected included age in years, sex, living area, current occupation (physician, nurse, or other), and the presence of chronic comorbidities (yes or no).
Participants were categorized according to their work environment into frontline healthcare workers (FLHCWs) and non-frontline healthcare workers (NFLHCWs). FLHCWs are considered to be at the highest risk for work-related exposure to severe acute respiratory syndrome coronavirus 2, the virus that causes COVID-19, due to their on-site work duties that involve being in close proximity (<2 meters) to the public or coworkers [19]. NFLHCWs, in contrast, are defined as individuals who are not directly involved in patient care but may still be potentially exposed to infectious agents while working in a healthcare setting [19]. The work position was classified into 3 categories: direct care and treatment, tracing and sampling, and logistics and administration. Changes in work situations before and during the pandemic were based on individuals’ self-reported data regarding their work days per week and rest time during work shifts, as compared to their pre-COVID-19 schedules. The classifications included an increase or no increase in the amount of time spent working (either in days or hours).
Dependent variables
Sleep quality was assessed using the standardized Pittsburgh Sleep Quality Index (PSQI) [20]. The PSQI is a self-report questionnaire that evaluates sleep quality over a 1-month period. This tool consists of 19 items across 7 components, with a total score range of 0 to 21. The PSQI has been translated and validated for the Vietnamese population [21]. A total PSQI score of ≥5 indicates poor sleep quality, while a score below 5 is classified as good sleep quality [20].
Statistical Analysis
The data were analyzed using SPSS version 11.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were employed to summarize participants’ socio-demographic factors. For continuous variables, the arithmetic mean and standard deviation were reported, while counts and percentages were reported for categorical variables. The independent sample t-test was utilized to compare 2 groups for continuous variables, and the chi-square test was used for categorical variables. A multivariable logistic regression model was analyzed to identify factors associated with sleep quality. A p-value of <0.05 was set as the significance level.
Ethics Statement
This study underwent review and approval by the Medical Ethics Committee at the Institute of Public Health in Ho Chi Minh City, Vietnam (No. H202/041).
RESULTS
A total of 1000 HCWs participated in the survey. Among them, 37.7% were doctors, 40.3% were nurses, and 22.0% belonged to other occupational groups, such as laboratory technicians, pharmacists, and public health officers. The mean age of the participants was 33.20±6.81 (range, 20.0–61.0), with a majority (63.0%) being females. The median work experience was 8.54±6.30 years. Furthermore, 6.3% (63 out of 1000 HCWs) had chronic comorbidities, such as hypertension and diabetes mellitus (Table 1).
In terms of work characteristics, 56.1% of HCWs experienced an increase in daily working hours, and 75.3% reported an increase in work days per week compared to pre-COVID-19 levels. Nearly 72.9% indicated a decrease in rest time during work shifts compared to before the pandemic. Additionally, 59.4% of HCWs reported an increased frequency of encountering critically ill patients and higher mortality rates. As many as 65.5% felt their anxiety about their health had increased compared to before the COVID-19 pandemic (Table 1).
Regarding sleep status, 73.8% of participants exhibited poor sleep quality based on the PSQI scale (Table 1), with an average score of 7.37±3.71 for all participants. FLHCWs, who directly care for and treat patients, had a mean score of 7.75±3.82, while NFLHCWs, who perform tasks such as performing swabs for COVID-19 cases and logistics work, had a mean score of 6.82±3.46 (Table 2).
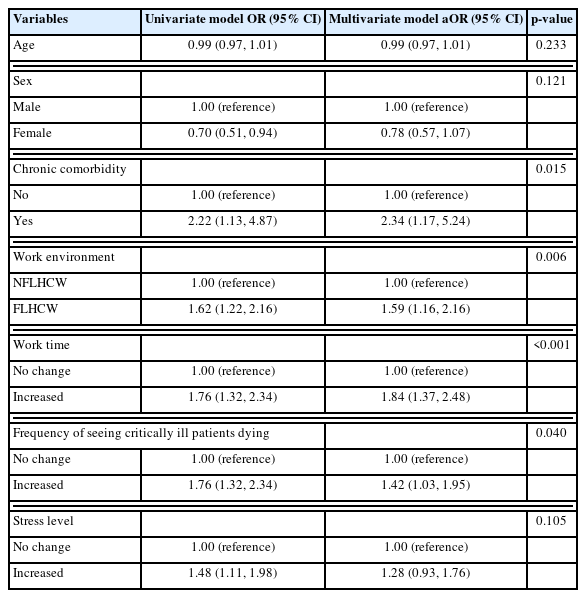
Results from the multivariate logistic regression analysis revealed that the presence of chronic comorbidity (odds ratio [OR], 2.34; 95% CI, 1.17 to 5.24), working in an FLHCW position (OR, 1.59; 95% CI, 1.16 to 2.16), increased working hours (OR, 1.84; 95% CI, 1.37 to 2.48), and a higher frequency of encountering critically ill and dying patients (OR, 1.42; 95% CI, 1.03 to 1.95) were all significantly associated with poor sleep quality among HCWs (Table 3).
DISCUSSION
Our findings regarding poor sleep quality, as measured by the PSQI scale, were consistent with other studies conducted on similar research participants in Kuwait (78.8%) and Iraq (68.3%) [3,5]. In contrast, Jahrami et al. [22] reported that poor sleep quality was observed in 75–76% of both FLHCWs and NFLHCWs. In our study, we identified several factors associated with poor sleep quality among HCWs through multivariate logistic regression. These factors included chronic comorbidity, being an FLHCW, increased working hours, and a higher frequency of encountering critically ill or dying patients.
HCWs with chronic comorbidities, such as diabetes mellitus and hypertension, were found to have a higher risk of poor sleep quality compared to those without chronic comorbidities. Patients with chronic diseases, particularly diabetes mellitus, experienced lower sleep quality than the general population due to issues with blood sugar regulation, which can lead to further complications and diminished sleep quality [23]. Motahedi et al. [5] study also demonstrated that comorbidity was associated with poor sleep quality. In contrast, Liu et al. [15] revealed that HCWs with chronic pain comorbidity were more likely to have poor sleep quality. Furthermore, it is worth noting that individuals with non-communicable diseases may be at a higher risk of experiencing worsened conditions if infected with COVID-19, which could lead to increased anxiety about their health and negatively impact their sleep [24].
Working as an FLHCW was a risk factor for poor sleep quality. Several studies have reported similar findings, with the highest levels of poor sleep quality observed among FLHCWs [5,9]. This can be attributed to the fact that FLHCWs often experience increased work-related stress disorders, sleep deprivation, and the unique challenges of night shift duties, as well as having to rapidly adapt to tasks based on patient needs or work demands, all of which can contribute to poor sleep quality [24]. Furthermore, FLHCWs face a higher risk of infection in COVID-19 treatment areas, have direct contact with COVID-19 patients, and may experience frustration and discrimination, which can cause anxiety and negatively impact sleep quality [25].
In terms of work time, our results were consistent with other studies, which found that HCWs with extended working hours, rotating shifts, and on-call hospital duties were more susceptible to poor sleep quality [26], or that HCWs with longer working hours each week experienced worse sleep quality compared to those who worked regular hours [5,15]. During the fourth wave of the COVID-19 pandemic, the rapid increase in cases and deaths, coupled with an overwhelming workload with limited resources and the need for constant updates to treatment protocols in response to the ever-changing epidemic situation, led to increased working hours for HCWs. Consequently, they had to work for extended periods with little time for rest and recovery, resulting in stress, prolonged fatigue, and poor sleep quality [12,13]. This also contributed to increased stress, fatigue, burnout, and reduced sleep quality among HCWs [5, 11,27,28].
Nearly 60% of HCWs reported witnessing a higher number of critically ill patients and deaths during the COVID-19 pandemic compared to before the pandemic. This observation aligns with the COVID-19 situation in Vietnam, where there was a rapid increase in community cases, leading to a surge in hospital admissions [29]. In addition to the rise in case numbers, HCWs faced an unprecedented increase in the severity of patients’ conditions and mortality rates, particularly in Ho Chi Minh City, where the growing number of severe cases quickly overwhelmed intensive care unit capacity [30]. Our study results indicate that HCWs who frequently encountered critically ill or dying patients were at a higher risk of experiencing poorer sleep quality compared to their counterparts (Table 3). This elevated risk may be attributed to the psychological impact of witnessing numerous brutal and unexpected deaths, which can lead to post-traumatic stress and acute stress [12,31]. These factors have been associated with reduced sleep quality [12,32].
This cross-sectional study, which examines sleep quality among HCWs in Vietnam during the COVID-19 pandemic, has several limitations. One notable limitation is the reliance on self-reported data, which may be subject to recall bias and social desirability bias, potentially affecting the accuracy of the results. Moreover, the study’s cross-sectional design hinders the establishment of causality between variables. Another limitation is the potential for selection bias, as the study employed an online questionnaire that may have excluded HCWs without Internet access or those unwilling to participate. Additionally, the study’s geographic scope is confined to only 3 regions of Vietnam, which may restrict the generalizability of the findings to other parts of the country or other countries facing distinct pandemic-related challenges. Lastly, the study did not account for potential confounding factors, such as personal lifestyle factors or the effects of shift work, that may have influenced the sleep quality of HCWs.
ACKNOWLEDGEMENTS
We would like to acknowledge WHO Vietnam for financial and technical support during the study. In addition, thank the Institute of Public Health staff members in Ho Chi Minh City, Vietnam for their organizational and logistical support from the first days of this study until the end.
Notes
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
AUTHOR CONTRIBUTIONS
Conceptualization: Nguyen NPT, Nguyen HPA, Le VT, Dinh TV, Dang CV, Ho TH, Quynh HHN, Phan T. Data curation: Nguyen NPT, Phan MT, Phan T. Formal analysis: Phan MT, Khoa Dang CK, Nguyen VT, Nguyen MT. Methodology: Nguyen NPT, Le VT, Nguyen HPA, Dinh TV, Phan T. Project administration: Dang CV, Ho TH, Le VT. Writing – original draft: Nguyen HPA, Nguyen NPT, Phan T, Dang BT, Le MT, Dinh TV, Nguyen VT, Phan MT, Ho TH, Nguyen MT, Khoa Dang C. Writing – review & editing: Le VT, Quynh HHN, Tran BT, Phan VT, Dang CV.
FUNDING
None.