Mediating Effect of Cognitive Function on the Relationship Between Geriatric Oral Health and Quality of Life Among Korean Seniors
Article information
Abstract
Objectives
Previous studies have found that the oral health of seniors can affect their physical nutrition and quality of life (QoL). Additionally, poor oral health can lead to the development of dementia, which is associated with decreased cognitive function. This study aimed to examine the impact of geriatric oral health (GOH) on the QoL of Korean seniors and the mediating effects of cognitive function.
Methods
We used data from the seventh Korean Longitudinal Study of Aging conducted in 2018. In total, 4049 seniors were included in our study. We analyzed the impact of GOH on QoL according to 5 mediating domains of cognitive function and control variables. To examine each path of mediating effects, bootstrapping with 5000 iterations was performed with 95% confidence intervals.
Results
Our findings revealed that good GOH had a positive effect on the QoL of seniors. Also, better GOH corresponded to a higher degree of cognitive function within all 5 domains: orientation, memory registration, attention/calculation, memory recall, and language and visuospatial ability. In addition, 3 domains of the 5 domains (attention/calculation, memory recall, and language and visuospatial ability) had significant mediating effects on the relationship between GOH and QoL.
Conclusions
This study suggests that adequate management of GOH is crucial for promoting a better QoL and a high degree of cognitive function among seniors. To prevent cognitive impairment, such as dementia, future studies should take a more targeted approach by examining data according to each cognitive domain and various socio-demographic factors.
INTRODUCTION
The proportion of individuals aged 65 years and older in Korea reached 15.7% (approximately 8 125 000 people) in 2020. Oral health problems such as periodontal disease are some of the most commonly diagnosed conditions among seniors [1]. Geriatric oral health (GOH) is closely related to nutritional intake and interpersonal relationships, both of which affect the quality of life (QoL) [2,3]. In addition, several variables related to chewing ability, such as the occlusal force of the posterior teeth, tooth loss, and the use of dentures, also correlate with cognitive decline and the risk of dementia [4-6]. Cognitive decline causes depression and social isolation in seniors, which, like GOH, affect their QoL [7].
Therefore, oral hygiene and cognitive health promotion programs are essential for improving seniors’ QoL [8]. Previous studies have used the Geriatric Oral Health Assessment Index (GOHAI) to identify the relationship between GOH and QoL [9,10]. However, findings on the effects of cognitive decline caused by GOH on QoL were inconclusive. Further, there are multiple domains of cognitive function, including orientation, memory, and concentration, for which diagnosis and treatment methods may vary depending on the level of deterioration within each domain. Nonetheless, no studies have analyzed each domain individually. Thus, this study aimed to comprehensively examine the effect of GOH on QoL and the mediating effect of cognitive function on their relationships to gather data supporting the development of an active GOH program.
METHODS
Data
Data from the seventh wave of the Korean Longitudinal Study of Aging (KLoSA) in 2018 were used to examine the effect of GOH on QoL and the mediating effect of cognitive function in seniors aged 65 years and older. The Korea Aging Research Panel Survey, a representative geriatric panel survey in Korea, was used to collect data on the demographic characteristics and health status of Korean seniors. This study included 4049 subjects aged 65 years and older from the seventh KLoSA for whom data were available on oral health, cognitive function, and QoL.
Independent variables
We used the GOHAI to assess oral health, which was the independent variable in this study. The GOHAI is an instrument that includes a 12-item questionnaire and is answered using a 6-point scale (1, always; 2, very often; 3, often; 4, sometimes; 5, seldom and 6, never). A higher GOHAI score indicates a higher QoL related to oral health [11,12]. The Cronbach’s α value for all items related to oral health was 0.860.
Dependent variables
The dependent variable in this study was QoL, which was measured using the subjects’ answers to a 5-item life satisfaction questionnaire from the seventh KLoSA. Each item assessed the respondents’ health status, economic status, relationships with their spouses, relationships with their children, and overall QoL. Total possible scores ranged from 0 to 100 and were calculated in 10-point increments, and a higher score indicated a higher degree of life satisfaction. Life satisfaction is the most critical indicator of an individual’s subjective QoL. Thus, life satisfaction and subjective QoL have been used interchangeably in previous studies [13]. We used the average score for the 5-item life satisfaction questionnaire from the seventh KLoSA as a proxy for QoL to comprehensively evaluate the physical, mental, and socioeconomic effects of oral health and cognitive function on QoL. The Cronbach’s α value for all items was 0.844.
Mediating variables
In this study, scores for each of the 5 domains of cognitive function (orientation of time and place, memory registration, attention/calculation, memory recall, and language and visuospatial ability) were measured using the Korean Mini-Mental State Examination (K-MMSE) [14,15]. The K-MMSE [16] is a 30-point questionnaire that is widely used in clinical and research settings to measure cognitive decline and dementia [17]. The total possible scores for each domain are 10 points for orientation, 3 points for memory registration, 5 points for attention/calculation, 3 points for memory recall, and 9 points for visuospatial ability. A higher score indicates a higher degree of cognitive function.
Control variables
The control variables for this study were gender, age, education level, household income, and area of residence. For gender, 0 and 1 were assigned as dummy variables for men and women, respectively, and age was considered a continuous variable. For education level, dummy variables of 1, 2, 3, and 4 were assigned for “elementary school or lower,” “middle school,” “high school,” and “undergraduate or higher,” respectively. Household income was considered a continuous variable, but the responses were log-transformed to conform to normality. For residential districts, dummy variables of 0 and 1 were assigned to dong districts, which are the administrative units that contain urban neighborhoods in Korea, and eup-myeon districts, which are the administrative units that contain rural towns in Korea, respectively.
Statistical Analysis
We confirmed the effects of GOH on QoL primarily by examining the mediating effect of cognitive function. A mediation effect model can take the regression analysis approach or the counterfactual approach. The regression analysis approach includes a traditional statistical model proposed by Baron and Kenny [18] that mainly uses a path diagram to graphically represent the regression equation derived from the structural relationship between the variables. Baron and Kenny proposed a 3-step approach. Step 1 shows how the independent variable X affects the dependent variable Y (path: X→Y). Step 2 tests the path X→M to examine the relationship between the independent variable X and the mediator M. Step 3 involves conducting multiple regression analysis to demonstrate how X and M affect Y simultaneously (path: X→Y, M→Y).
The counterfactual model, proposed by Pearl [19] and VanderWeele and Vansteelandt [20], includes an integrated framework for causal inference and can analyze linear as well as non-linear and non-parametric structural equation models. This model is divided into the controlled direct effect, natural direct effect (NDE), natural indirect effect (NIE), and the total effect of NDE+NIE. Using the counterfactual model, an analysis of the interaction effects between the variables and the unmeasured confounding factors that are difficult to consider in the traditional model can be conducted.
In this study, we used regression analysis approach due to its advantages related to exploratory model trimming and theory building. SPSS version 25.0 (IBM Corp., Armonk, NY, USA) was used for data processing and descriptive statistics. In addition, SPSS PROCESS Macro model 4, developed by Hayes [21], was used to confirm the effects of GOH and cognitive function on QoL and verify the multiple mediation effects of cognitive function subcategories. The PROCESS macro website (http://www.processmacro.org/) provides a free, downloadable file containing this model. Bootstrapping with 5000 iterations was conducted with 95% confidence intervals (CIs) to analyze each mediating effect.
Ethics Statement
In this study, we used KLoSA which is an open access source of secondary data. This data is available to anyone after logging in on the Korea Enployment Information Service website (https://survey.keis.or.kr/klosa/klosadownload/List.jsp). The data guarantees anonymity by using personal unique numbers to prevent exposure of personal information through personal identification. Therefore, it is possible to exempt from institutional review board approval and additional written consent since the risk of personal information leakage is very low.
RESULTS
Demographic and Socioeconomic Characteristics
A total of 4049 subjects were included in the present study, and their demographic characteristics are shown in Table 1. There were 1693 (41.8%) men and 2356 (58.2%) women, and the average age was 75.55 years (standard deviation [SD], 7.10). More than half of the subjects (n=2207, 54.5%), were elementary school graduates or under, and the annual average household income was approximately 22.1 million Korean won (SD, 22.8). A total of 2864 people (70.7%) resided in a dong district, whereas 1185 people (29.3%) resided in a eup-myeon district, with those who resided in a dong district exceeding the percentage of those who resided in a eup-myeon district by more than double. The average GOHAI score was 4.05 (SD, 0.72) out of 6, and the average QoL score was 58.89 (SD, 14.73) out of 100. The average scores for the domains of cognitive function were as follows: 8.94 (SD, 1.83) for orientation, 2.36 (SD, 0.91) for memory registration, 3.28 (SD, 1.84) for attention/calculation, 1.69 (SD, 1.07) for memory recall, and 7.35 (SD, 2.03) for language and visuospatial ability.
Model Testing
We used a total of 6 models to verify the effect of GOH on QoL and the mediating effects of the cognitive domains. In models 1 to 5, the effect of GOH on the cognitive domains was examined. In model 6, the effect of GOH and cognitive function on QoL was tested.
Table 2 shows the results of the analysis of the effects of GOH on each cognitive function domain. The results were statistically significantly high for all parameters: orientation (coefficient=0.393, p<0.001), memory registration (coefficient=0.199, p<0.001), attention and calculation (coefficient=0.549, p<0.001), memory recall (coefficient=0.227, p<0.001), and language and visuospatial ability (coefficient=0.507, p<0.001). In other words, better oral health corresponded to a higher score for all 5 domains of cognitive function. Goodness-of-fit testing was undertaken for models 1 to 5 (p<0.001), and the effect size for each model was 17.4%, 16.4%, 25.1%, 18.1%, and 25.0%, respectively. Based on these results, the related effect sizes (R2) for model 3 (attention and calculation) and model 5 (language and visuospatial) were the highest, at approximately 25% (model 3: R2=0.251; model 5: R2=0.250). Scores for the 5 subcategories were significantly lower for the control variables, especially among females, older seniors, and subjects with a low education level. Orientation scores were significantly lower among subjects with a higher household income. In addition, scores for memory registration and language and visuospatial ability were lower among subjects who lived in dong administrative units than among those who lived in eup-myeon administrative units.
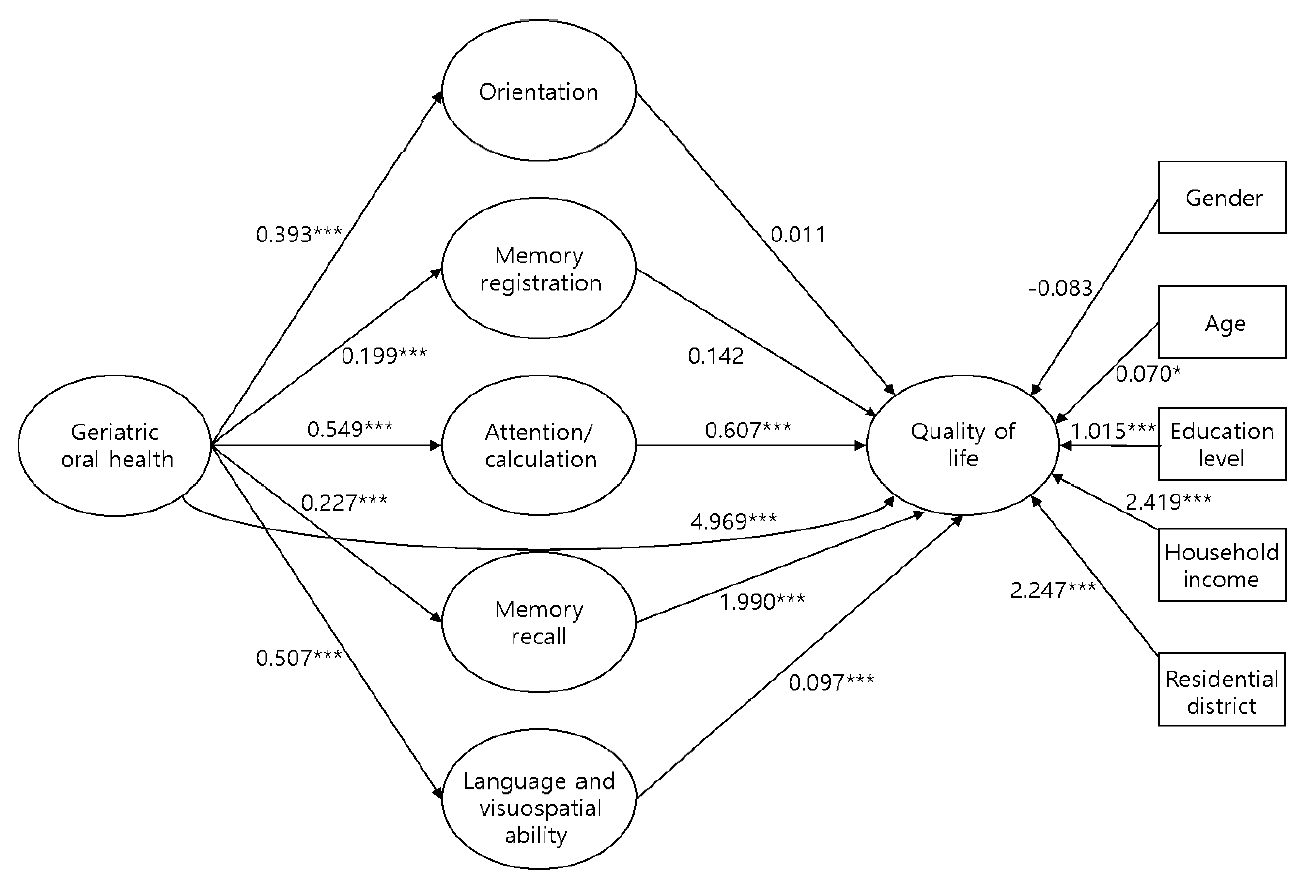
Table 3 shows the results for model 6, in which the effect of GOH and the cognitive function subcategories on QoL were examined. The effect size for the dependent variable (QoL) was 26.9% (R2=0.269), and the model fit the data well (F=134.823, p<0.001). The analysis indicated that better GOH (coefficient=4.969, p<0.001) corresponded to a higher QoL, and the 3 cognitive function subcategories of attention/calculation (coefficient=0.607, p<0.001), memory recall (coefficient=1.990, p<0.001), and language and visuospatial ability (coefficient=0.907, p<0.001) had statistically significant effects on QoL. QoL tended to be lower among women, older seniors, subjects with a low educational level, subjects with a low household income, and subjects who lived in eup-myeon districts. These results were statistically significant for variables except for gender (Figure 1).
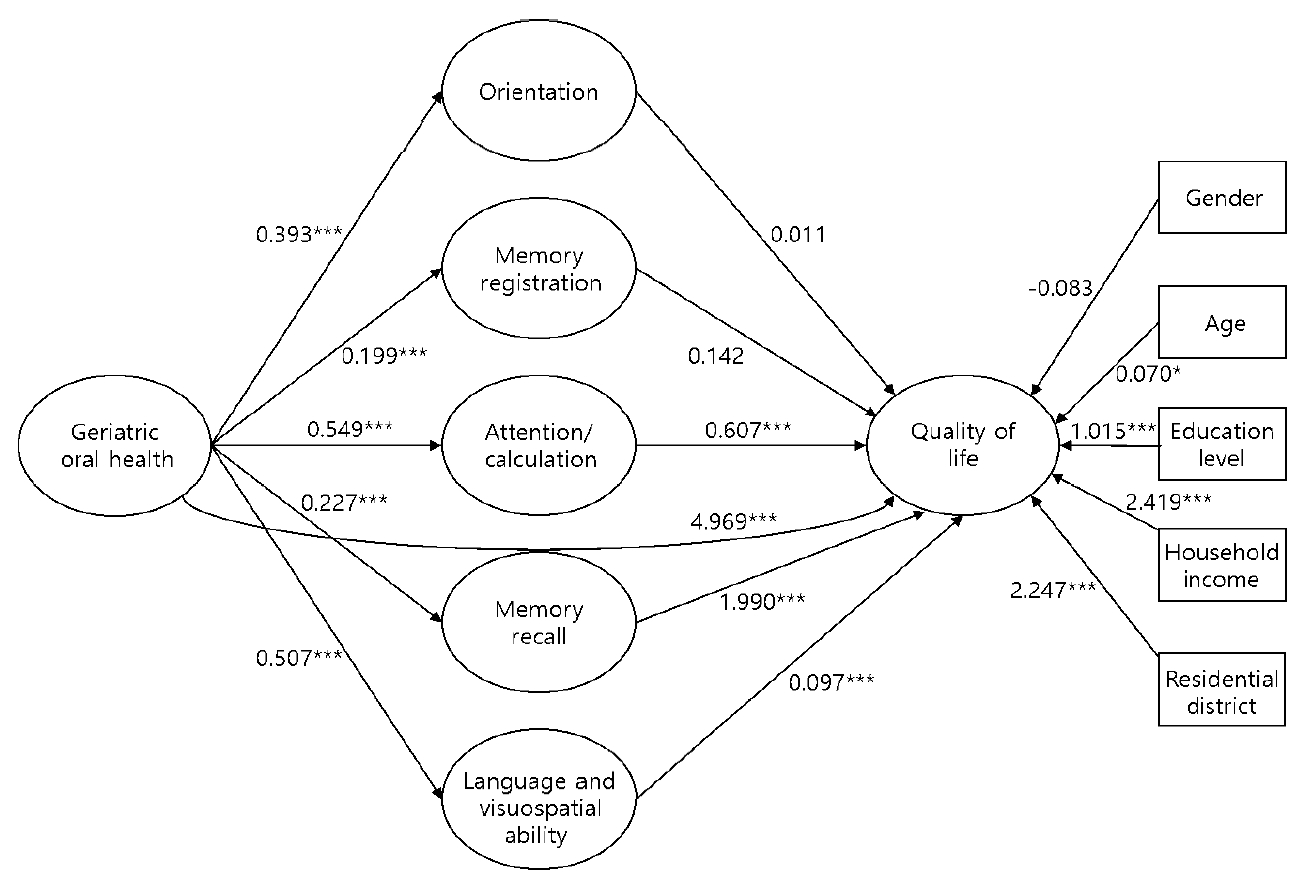
Mediating effect model of cognitive function on the relationship between geriatric oral health and quality of life.
***p<0.001.
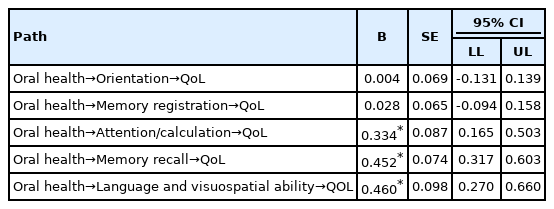
Table 4 shows each of the 5 cognitive function subcategories arranged as parameters to verify the mediating effect of cognitive function on the relationship between GOH and QoL. The results suggest that the paths (oral health→attention/calculation→QoL), (oral health→memory recall→QoL), (oral health→language and visuospatial ability→QoL) were statistically significant since their 95% CIs didn’t contain values of 0. Meanwhile, the paths (oral health→orientation→QoL) and (oral health→memory registration→QoL) were not statistically significant since their 95% CIs contained values of 0.
DISCUSSION
This study aimed to examine the effect of GOH on QOL and the mediating effect of cognitive function. Our findings show that GOH affects every subcategory of cognitive function. These results correspond to the results of previous studies in which poor oral health was found to lead to reduced chewing ability, which in turn affected cognitive function and brain activity related to memory and learning due to reduced blood flow in the brain [4-6]. Our results also reveal that GOH influences QOL. Previous studies have demonstrated that poor oral health can cause problems when consuming food and compromise systemic health, leading to health issues such as malnutrition, diabetes, and cardiovascular disorders. Poor oral health also can change the pronunciation and appearance of seniors which negatively affects interpersonal relationships [22,23]. In addition, three subcategories (attention/calculation, memory recall, language and visuospatial ability) were found to affect QOL along with GOH. Memory recall is a crucial area for determining cognitive decline, and a diagnosis of cognitive decline varies depending on the impairment of single or multiple domains [24]. Given that concentration, memory, and vocabulary are the main subcategories that adversely affect instrumental activities of daily living and participation in social activities, the diminished function of these areas may lower self-efficacy and self-esteem, causing social isolation, depression, and lower QOL [25]. Therefore, the statistically significant results for three subcategories of cognitive function support the findings of previous studies. The control variables (gender, age, education level, household income, residential districts) showed varying degrees of statistical significance related to cognitive function. Findings in the past also demonstrated that the degree of cognitive function differed according to the demographic characteristics, suggesting the need for education/training programs tailored with specific demographic profiles [25]. Lastly, gender, age, marital status, education level, and household income were found to statistically significantly affect geriatric QOL, which confirmed previous results [7].
We suggest the following policy recommendations based on our study finidngs. First, the promotion of oral examinations, including routine scaling, is essential for preventing primary disorders that affect the QOL of seniors, such as periodontal disease and dry mouth. Second, the National Dementia Care Center and local dental clinics should collaborate to expand support related to the national oral health project and medical coverage for older patients with mild cognitive impairment and a high risk of dementia [26]. Third, it is vital to implement targeted pharmaceutical and non-pharmaceutical interventions according to the demographic characteristics of the individual and the patterns of cognitive decline for each domain of a cognitive function. Treatments, including music, exercise, behavioral therapy, occupational therapy, recall exercises, communication, and cognitive stimulation therapy, can be used in reference to the domain of cognitive function being addressed [27]. While women appeared to have a higher degree of cognitive decline and impaired QOL than men, their orientation, memory registration, memory recall, and language and visuospatial ability were found to improve significantly after social interaction [28]. Thus, health and welfare services combine diverse efforts to address the needs of all seniors according to their physical, mental, and socioeconomic conditions are necessary.
There are several limitations in this study. First, due to the nature of utilizing cross-sectional data, a causal relationship cannot be inferred. Future studies should use longitudinal data to assess the relationships between GOH, QOL, and cognitive function. Second, the study subjects were likely limited to cognitively independent seniors since proxy surveys were not administered when the KLoSA was conducted. Future research should include subjects with severe cognitive impairment and classify them according to their risk of dementia. Third, due to small sample size, large-scale cohort data needs to be utilized to generalize the findings to elderly population of South Korea. Fourth, since the K-MMSE is a screening tool rather than a diagnostic tool, various cognitive function measurement tools should be used in the future to determine the effect size of the domains of cognitive function. Despite these limitations, our study identified the mediating effect of all domains of cognitive function on GOH and QOL, underlying the importance of adequate management of GOH for promoting a btter QOL among the elderly population [29-32].
SUPPLEMENTAL MATERIALS
Korean version is available at https://doi.org/10.3961/jpmph.21.536.
Notes
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
FUNDING
None.
ACKNOWLEDGEMENTS
None.
Notes
AUTHOR CONTRIBUTIONS
Conceptualization: Chang EJ, Jeong KH. Data curation: Chang EJ, Woo HJ. Formal analysis: Chang EJ, Woo HJ. Funding acquisition: None. Methodology: Jeong KH. Project administration: Woo HJ. Visualization: Chang EJ. Writing – original draft: Chang EJ. Writing – review & editing: Woo HJ, Jeong KH.