Behavioral Predictors Associated With COVID-19 Vaccination and Infection Among Men Who Have Sex With Men in Korea
Article information
Abstract
Objectives:
This study investigated the impact of socioeconomic factors and sexual orientation-related attributes on the rates of coronavirus disease 2019 (COVID-19) vaccination and infection among men who have sex with men (MSM).
Methods:
A web-based survey, supported by the National Research Foundation of Korea, was conducted among paying members of the leading online portal for the lesbian, gay, bisexual, transgender, or queer and questioning (LGBTQ+) community in Korea. The study participants were MSM living in Korea (n=942). COVID-19 vaccination and infection were considered dependent variables, while sexual orientation-related characteristics and adherence to non-pharmacological intervention (NPI) practices served as primary independent variables. To ensure analytical precision, nested logistic regression analyses were employed. These were further refined by dividing respondents into 4 categories based on sexual orientation and disclosure (or “coming-out”) status.
Results:
Among MSM, no definitive association was found between COVID-19 vaccination status and factors such as socioeconomic or sexual orientation-related attributes (with the latter including human immunodeficiency virus [HIV] status, sexual orientation, and disclosure experience). However, key determinants influencing COVID-19 infection were identified. Notably, people living with HIV (PLWH) exhibited a statistically significant predisposition towards COVID-19 infection. Furthermore, greater adherence to NPI practices among MSM corresponded to a lower likelihood of COVID-19 infection.
Conclusions:
This study underscores the high susceptibility to COVID-19 among PLWH within the LGBTQ+ community relative to their healthy MSM counterparts. Consequently, it is crucial to advocate for tailored preventive strategies, including robust NPIs, to protect these at-risk groups. Such measures are essential in reducing the disparities that may emerge in a post–COVID-19 environment.
INTRODUCTION
As of July 28, 2023, a total of 692 178 105 people had contracted coronavirus disease 2019 (COVID-19) globally, and 6 903 051 had died [1]. In 2021, major industrialized nations initiated vaccination campaigns with the goal of achieving herd immunity. However, immunization rates have varied due to factors such as vaccine availability, distribution logistics, and the level of public acceptance [2]. Developed countries, including the United States, the United Kingdom, Canada, and certain European nations, have reported high rates of vaccination [3]. Nevertheless, the world continues to grapple with vaccine inequality. Low-income and middle-income countries have faced delays in vaccine access due to resource limitations and supply issues [4]. As the virus has spread in these vulnerable regions, concerns have arisen. Even within developed countries, disparities in vaccination rates impact racial minorities, socioeconomically disadvantaged groups, and residents of remote areas [5-7]. These disparities can be attributed to factors such as healthcare system structure, vaccine access, and digital literacy levels. In some developed countries, younger demographic groups have exhibited lower vaccination rates than their older counterparts [8]. As initial vaccination campaigns prioritized the elderly and those with underlying health conditions, this strategy required younger populations to wait. However, the disparity in pandemic vaccination rates within countries—as opposed to between countries— remains an under-researched area, particularly regarding social minorities.
In Korea, where reports suggest a substantial presence of homophobia, empirical data concerning COVID-19 vaccination and infection rates among sexual minorities remain elusive. This scarcity of data stems from the difficulty in determining the total number of sexual minorities, a figure that serves as the denominator in such studies. Of Korea’s approximately 51 million inhabitants, around 32 million have contracted COVID-19, with 35 216 deaths. The vaccination coverage rate, defined as requiring at least 2 doses, stands at 87.11% [9]. However, knowledge remains limited about vaccination penetration, COVID-19 incidence, and mortality within the Korean lesbian, gay, bisexual, transgender, or queer and questioning (LGBTQ+) community. This study explores the socioeconomic factors and specific characteristics of men who have sex with men (MSM), as well as how these elements influence exposure to and vaccination against COVID-19.
Individual-level socioeconomic factors can substantially influence vaccination tendencies. Age is a particularly notable determinant of COVID-19 vaccination propensity. The strategy of prioritizing the elderly in vaccination campaigns is justified by their heightened vulnerability to severe consequences from the virus, and it results in higher vaccination rates among this demographic [10]. Additionally, educational attainment profoundly shapes personal health decisions, including vaccine uptake. Existing research reveals a positive correlation between higher education levels and improved vaccine accessibility [11]. This relationship arises from the likelihood that well-educated individuals can access credible health data, understand the benefits of vaccination, and consequently make informed health decisions. Additionally, economic disparities are reflected in vaccination rates, with economically marginalized groups potentially facing challenges in accessing vaccination sites, scheduling appointments, and obtaining time off for vaccination [12].
Certain characteristics inherent to specific populations, such as those within the LGBTQ+ community, can also impact vaccination rates. Factors such as human immunodeficiency virus (HIV) status, sexual orientation, and the disclosure of sexual orientation can play key roles. People living with HIV (PLWH) may face obstacles to COVID-19 vaccination due to existing health conditions and potential interactions with antiretroviral regimens [13]. Moreover, LGBTQ+ individuals might grapple with barriers to healthcare access stemming from societal prejudice, stigma, and discrimination, potentially reducing vaccination uptake [14]. The decision to disclose one’s sexual orientation, or “come out,” is influenced by myriad societal, cultural, and familial factors, which can in turn shape healthcare choices [15]. The concept of intersectionality clarifies how overlapping vulnerabilities within minority groups result in marked disparities [16]. For example, those who disclose their sexual orientation may face intensified prejudice [17].
Fundamentally, COVID-19 vaccination is a strategic health initiative designed to curb the spread of the virus. Therefore, it is crucial to evaluate how the previously mentioned individual and group characteristics influence the relationship between vaccination and infection rates. However, non-pharmacological interventions (NPIs) also play a critical role in controlling the spread, particularly during prolonged pandemics [18]. NPIs, which are distinct from pharmacological measures such as vaccination, include strategies designed to protect individuals and communities from infection [19]. These include practices such as hand hygiene, mask-wearing, ensuring proper ventilation, social distancing, and quarantine measures. Consequently, it becomes essential to investigate the adherence of sexual minorities with NPIs in relation to their vaccination and infection rates. This study was conducted to explore how the distinct socioeconomic and sexual orientation-related characteristics of MSM affect their experiences with COVID-19.
METHODS
Datasets
The participants in this study were paying members of Ivan City (https://ivancity.com/bbs/login.php), Korea’s largest online portal for the LGBTQ+ community. “Ivan” is a slang term used by LGBT individuals in Korea to distinguish themselves from “ilvan” (heterosexual people), or the mainstream society. Ivan City has been operated by LGBT KOREA since 1999, and approximately 95% of its members are MSM. In collaboration with the Ivan City management team, 10 000 user IDs were randomly selected, representing approximately 5% of active accounts. A link to a web survey was provided by Hankook Research, a commissioned research institute, and 1000 responses were received, equating to 10% of the selected IDs. All data collected by Hankook Research were de-identified to ensure the privacy of the respondents. In the web survey, respondents were excluded through a double confirmation procedure if they (1) were female, (2) were under 19 years old or over 60 years old, or (3) had no experience of sexual contact. The survey was conducted from July 22, 2022 to July 29, 2022. Interested respondents participated in the online survey by clicking on an external link provided by Hankook Research. The self-administered questionnaire took approximately 20 minutes to complete. Respondents were compensated with coupons worth 5000 Korean won (approximately 3.8 US dollars [USD]) credited to their Ivan City accounts, without the need to provide identifying information such as mobile phone numbers. A total of 942 people responded to the final survey.
Measures
Dependent variables
In this study, the dependent variables included COVID-19 vaccination and infection status. First, COVID-19 vaccination status was determined based on whether the respondent had completed the second round of Korea’s 2021 vaccination program, which depended on the prevailing quarantine situation. Specifically, respondents who had not been vaccinated or had received only 1 dose were categorized as unvaccinated (0), while those who had received 2 or more doses (including booster shots) were classified as vaccinated (1). However, this applied only to the AstraZeneca, Pfizer, Moderna, or other vaccines that met the standards of the Korea Disease Control and Prevention Agency. For those who received the Janssen vaccine, a single dose was considered sufficient for a status of “vaccinated.” Other vaccines were not available in Korea at the time. Next, COVID-19 infection status was determined based on 2022 results (specifically, polymerase chain reaction-positive determination made at a medical institution or public health center). This was done to prevent reverse causation; notably, the number of COVID-19 infections was very small from 2020 to 2021. In the model involving COVID-19 infection as a dependent variable, COVID-19 vaccination status was included as an independent variable.
Independent variables
Sexual orientation-related characteristics and NPIs
First, we measured variables related to sexual orientation, such as sexual orientation itself, disclosure status, and HIV status [20]. The question regarding HIV infection was “Have you been diagnosed with HIV?” Responses included “yes” (1) and “no” (0). In accordance with previous studies [17], we further categorized MSM respondents based on their disclosure (or “coming-out”) status and sexual orientation. If a respondent had not come out, the former measure was classified as “no” (0) while if the individual had come out, whether voluntarily or involuntarily, it was classified as “yes” (1). Sexual orientation referred to an individual’s self-reported perception of attraction, with “homosexual” receiving a response of (1) and “bisexual” receiving a response of (2). Using this method, we classified the latent group and conducted detailed regression analyses.
Adherence to NPIs was then measured using 5 questions [18]. We asked respondents whether they had practiced the following disease prevention measures during the COVID-19 pandemic: “avoiding contact with people who have contagious diseases,” “washing hands or using hand sanitizer,” “avoiding touching the eyes, nose, and mouth,” “refraining from going out during an epidemic,” “avoiding places of frequent contact with people,” and “wearing a face mask.” The responses were categorized as follows: “not practiced at all,” “practiced infrequently,” “practiced regularly,” “practiced as much as possible,” and “practiced without fail.” To reduce the number of study variables (NPIs) and identify the internal variance structure among these variables, we conducted a principal component analysis (PCA). The PCA factors that were used to construct the information barrier index were those exhibiting eigenvalues greater than 1.00 and factor loadings exceeding 0.40.
Covariates
The model was adjusted to account for respondent age, educational attainment, and equivalized annual household income, as these were identified as potential confounding variables.
Statistical Analysis
First, a descriptive statistical analysis was conducted on the general characteristics of the male sexual minorities who participated in the survey. These attributes included socioeconomic status, sexual orientation-related characteristics, and factors associated with COVID-19. Second, following the execution of factor analysis on the NPIs, the factor loading values were incorporated into the regression model. Third, nested regression analyses were implemented to determine the predictive factors influencing COVID-19 vaccination and infection among MSM. All statistical analyses were performed using Stata version 14.0 (Stata Corp., College Station, TX, USA).
Ethics Statement
The sampling and recruitment procedures adhered to the research ethics guidelines of the National Research Foundation of Korea. These procedures received approval from the Institutional Review Board (IRB) of Dongduk Women’s University (DDWU2206-02). To protect the participants, informed consent was secured before the survey was conducted. A market research firm, Hankook Research, was responsible for data collection for the study. Survey responses were received after written informed consent was obtained from each of the 942 respondents. The entire data collection process was reviewed and approved by the IRB of Dongduk Women’s University.
RESULTS
General Characteristics of Respondents
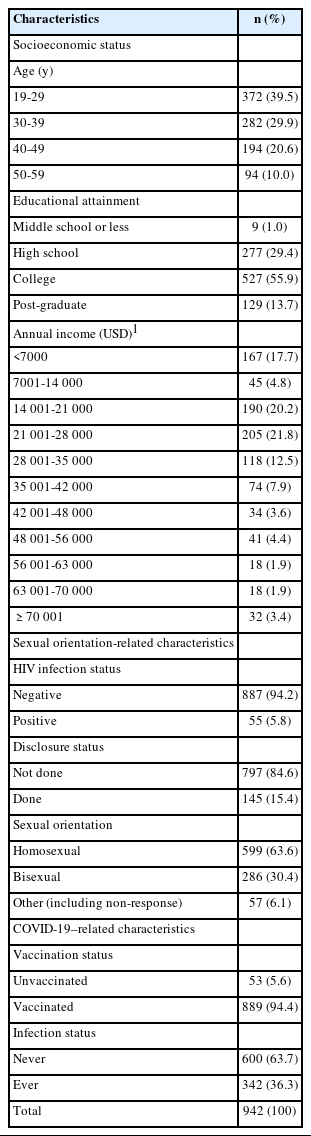
Table 1 presents the general characteristics of the 942 respondents. In terms of socioeconomic characteristics, individuals aged 19 years to 29 years comprised 39.5% of the study population. Regarding educational attainment, the majority were university graduates, at 55.9%. The most common annual income bracket was 21 001 USD to 28 000 USD, accounting for 21.8% of the study population. For sexual orientation-related characteristics, 5.8% of the respondents were HIV-positive, and 15.4% of respondents had come out. Concerning sexual orientation, 63.6% of the respondents reported that they identified as gay. Regarding COVID-19–related factors, 94.4% of the respondents had been vaccinated, and 36.3% of the respondents had contracted COVID-19.
Results of the Factor and Reliability Analysis of Non-pharmacological Interventions Practice
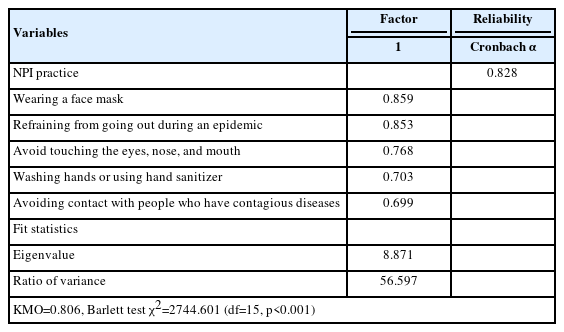
Table 2 presents the results of the factor and reliability analysis of the respondents’ NPI practices. The factor analysis of indicators, which were measured using 5 items related to NPI practices, resulted in the extraction of 1 factor. The eigenvalue was 8.871, and the variance ratio was 56.597. The Cronbach alpha value for the reliability of the 5 items was 0.828.
Nested Regression Analyses of Coronavirus Disease 2019 Vaccination Determinants According to Sexual Orientation and Disclosure Status
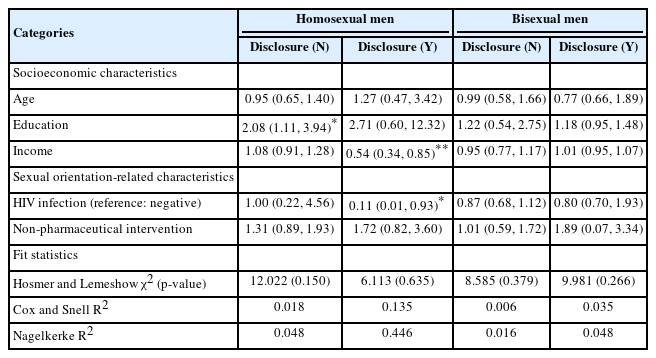
Table 3 presents the results of nested regression analyses on the determinants of COVID-19 vaccination, considering sexual orientation and disclosure status. For MSM who had not come out, the likelihood of vaccination increased with higher educational attainment (odds ratio, 2.08; 95% confidence interval [CI], 1.11 to 3.94). Among MSM who had come out, those with higher incomes were 0.54 times less likely to have been vaccinated than those with comparatively low incomes (95% CI, 0.34 to 0.85). Furthermore, vaccination was 0.11 times less likely in the HIV-positive group compared to the HIV-negative group (95% CI, 0.01 to 0.93). In contrast, no statistically significant predictors of vaccination were identified for bisexual individuals who had not come out, nor were significant determinants found for bisexual individuals who had come out. Consequently, no specific trends or patterns were discernible in this study’s model regarding COVID-19 vaccination. Therefore, no consistent association was found between the COVID-19 vaccination of MSM and characteristics related to socioeconomic status or sexual orientation (namely sexual orientation itself, HIV infection, and disclosure status).
Nested Regression Analyses of Determinants of Coronavirus Disease 2019 Infection According to Sexual Orientation and Disclosure Status
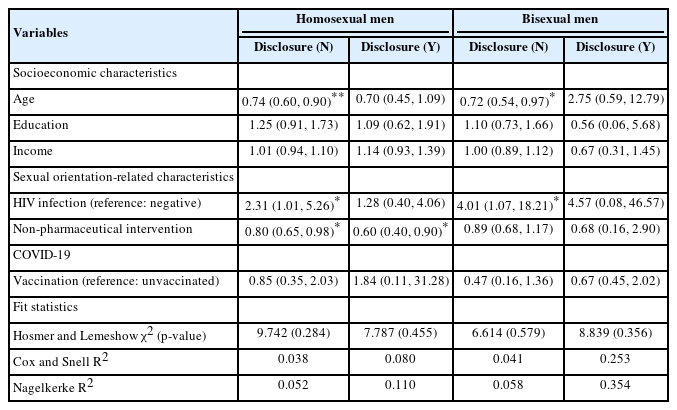
Table 4 presents the results of nested regression analyses on the determinants of COVID-19 infection, segmented by sexual orientation and disclosure status. Among MSM who had not come out, older individuals were 0.74 times less likely to contract COVID-19 (95% CI, 0.60 to 0.90). Furthermore, the probability of being infected with COVID-19 was 0.80 times lower (95% CI, 0.65 to 0.98) when NPIs were practiced. However, for HIV-positive respondents, the likelihood of contracting COVID-19 was 2.31 times higher than for the HIV-negative group (95% CI, 1.01 to 5.26). Among MSM who had come out, the more they adhered to NPIs, the less likely they were to contract COVID-19 (95% CI, 0.40 to 0.90). In contrast, among bisexual individuals who had not come out, older respondents were 0.72 times less likely to have been infected with COVID-19 (95% CI, 0.54 to 0.97). Additionally, the HIV-positive group was 4.01 times more likely to contract COVID-19 than the HIV-negative respondents (95% CI, 1.07 to 18.21). Among bisexual individuals who had come out, no statistically significant factors were identified that could predict COVID-19 infection. Overall, among MSM and bisexual individuals who had not come out, the HIV-positive group was significantly more likely to contract COVID-19. Among MSM, the likelihood of contracting COVID-19 was significantly lower when NPIs were practiced, regardless of sexual orientation disclosure status.
DISCUSSION
Disasters, including the consequences of COVID-19, invariably exert pronounced effects on vulnerable populations [21-23]. However, the literature includes a noticeable lack of targeted empirical studies exploring the experiences of specific minority groups throughout the pandemic. The present investigation explored the interplay between socioeconomic and sexual orientation determinants unique to MSM in the context of COVID-19 vaccination and infection. Vaccine hesitancy may be especially pronounced in communities affected by societal stigma, while individuals with HIV may display increased vulnerability to COVID-19 due to the compromised state of their immune systems. The key findings of this study are detailed as follows.
First, no discernible correlation was observed between the examined socioeconomic or sexual orientation attributes (with the latter including sexual orientation, disclosure of sexual orientation, and HIV status) of MSM and their rates of COVID-19 vaccination or infection. Often, socioeconomically marginalized communities are relegated to subpar living conditions, which restricts access to healthcare, increases infection risk, and reduces adherence to treatment regimens [24,25]. However, factors such as age, educational attainment, and income did not show predictable correlations with vaccination or infection rates among our respondents. Moreover, vaccination did not appear to confer immunity against COVID-19 infection among vaccinated respondents. It may be hasty to infer vaccine inefficacy from these real-world data, and clinical studies have underscored the high efficacy of the Pfizer-BioNTech, Moderna, and AstraZeneca vaccines in preventing symptomatic COVID-19 [26-28]. Nonetheless, it is crucial to recognize that no vaccine guarantees complete immunity. Empirical evidence has consistently shown that vaccines are effective in substantially reducing the risk of severe symptoms, hospitalizations, and deaths, even in the context of emerging virus variants [29].
Second, HIV status emerged as a significant determinant of susceptibility to COVID-19 infection. HIV has a detrimental impact on CD4 T cells, weakening the robustness of the immune system over time [30]. As a result, immunocompromised individuals naturally exhibit an increased vulnerability to new pathogens. However, the role of HIV in modulating susceptibility to severe acute respiratory syndrome coronavirus 2 has not yet been definitively determined. Initial data from Europe did not indicate an unusual prevalence of COVID-19 among PLWH [31]. However, subsequent extensive studies, particularly one from South Africa, identified a substantially increased risk of COVID-19–related mortality among PLWH, suggesting potential vulnerabilities [32]. This research implies that HIV may increase susceptibility to COVID-19, particularly among MSM who have not disclosed their sexual orientation. Hence, closeted segments of the LGBTQ+ community may exhibit relatively high susceptibility to concomitant transmission of both HIV and COVID-19.
Finally, a clear inverse relationship was observed between the practice of NPIs by MSM and their likelihood of contracting COVID-19. These findings underscore the potential critical importance of NPIs, possibly even surpassing pharmacological interventions such as vaccines, during public health crises [33]. For example, research conducted by Stanford University confirmed that mandatory mask-wearing led to a noticeable decrease in the daily growth rate of COVID-19 cases [34]. Furthermore, an evaluation by Imperial College London showed that countries advocating for social distancing experienced reduced virus transmission [35]. Interestingly, this study did not find a statistically significant correlation between adherence to NPIs and COVID-19 infection among bisexual men. Consequently, additional research is needed to understand the changes in relational dynamics within the LGBTQ+ community during the pandemic. It is plausible that measures such as physical distancing and mask-wearing have prompted modifications in sexual behaviors. This observation is consistent with another finding from the study, which emphasized that older, non-disclosed sexual minorities exhibited lower chances of COVID-19 infection. Across wider demographics, increasing age is typically correlated with heightened vulnerability to COVID-19.
This research, while insightful, has some limitations. First, the use of cross-sectional data means that the possibility of reverse causation cannot be dismissed outright. However, the design of the study did ensure temporal precedence between the independent variable, identified as the cause, and the dependent variable, interpreted as the effect. For context, Korea began its government-sponsored vaccination campaign in the spring of 2021, with the second vaccine dose being administered to willing participants by the fall of the same year. Given that the model incorporated data on COVID-19 infections from 2022 as the dependent variable, the probability of reverse causality between vaccination and subsequent infection is minimal. Second, due to ethical considerations inherent to the research process, the study did not access information from participants’ medical histories, specifically concerning pre-exposure prophylaxis and antiretroviral therapy utilization. Consequently, the model did not fully encapsulate the multifaceted determinants beyond the realm of behavioral science that may influence COVID-19 vaccination and infection trajectories. Finally, the potential exists for a latent confounding variable to influence the dependent variable. Given that this research is based in the field of behavioral medicine, it is inherently difficult to incorporate all potential determinants of individual decision-making into the model. Therefore, a clear need exists to refine and develop a more nuanced model that elucidates the dynamics of vaccination and disease susceptibility among MSM in future studies.
This study meticulously examined the interplay between socioeconomic factors and sexual orientation-related characteristics, specifically among MSM, regarding how these factors influence their COVID-19 vaccination and infection rates. During the COVID-19 pandemic, the LGBTQ+ community in Korea faced substantial barriers to HIV testing at medical facilities. This situation was exacerbated by an increase in societal stigma, fueled in part by widespread fears related to COVID-19. Furthermore, from an immunological perspective, having a positive HIV status seemingly increases vulnerability to COVID-19. Therefore, it is crucial to adopt an intersectional approach to unravel the layers of inequality that the pandemic has amplified, ensuring that we not only understand but also learn valuable lessons from these disparities.
Notes
Conflict of Interest
The author has no conflicts of interest associated with the material presented in this paper.
Funding
This work was supported by the National Research Foundation of Korea Grant, funded by the Korean government (NRF-2022R1F1A1062998).
Author Contributions
All work was done by MJ.
Acknowledgements
None.