Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 55(4); 2022 > Article
-
Original Article
Increase in Potential Low-value Magnetic Resonance Imaging Utilization Due to Out-of-pocket Payment Reduction Across Income Groups in Korea: An Experimental Vignette Study -
Yukyung Shin1
 , Ji-Su Lee1
, Ji-Su Lee1 , Young Kyung Do1,2
, Young Kyung Do1,2
-
Journal of Preventive Medicine and Public Health 2022;55(4):389-397.
DOI: https://doi.org/10.3961/jpmph.22.208
Published online: July 11, 2022
1Department of Health Policy and Management, Seoul National University College of Medicine, Seoul, Korea
2Institute of Health Policy and Management, Seoul National University Medical Research Center, Seoul, Korea
- Corresponding author: Young Kyung Do, Department of Health Policy and Management, Seoul National University College of Medicine, 103 Daehak-ro, Jongno-gu, Seoul 03080, Korea, E-mail: ykdo89@snu.ac.kr
Copyright © 2022 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- This study examined the effect of out-of-pocket (OOP) payment reduction on the potential utilization of low-value magnetic resonance imaging (MRI) across income groups.
-
Methods
- We conducted an experimental vignette survey using a proportional quota-based sample of individuals in Korea (n=1229). In two hypothetical vignettes, participants were asked whether they would be willing to use MRI if they had uncomplicated headache and non-specific low back pain, each before and after OOP payment reduction. To account for the possible role of physician inducement, half of the participants were initially presented with vignettes that included a physician recommendation for low-value care. The predicted probability, slope index of inequality (SII), and relative index of inequality (RII) were calculated using logistic regression.
-
Results
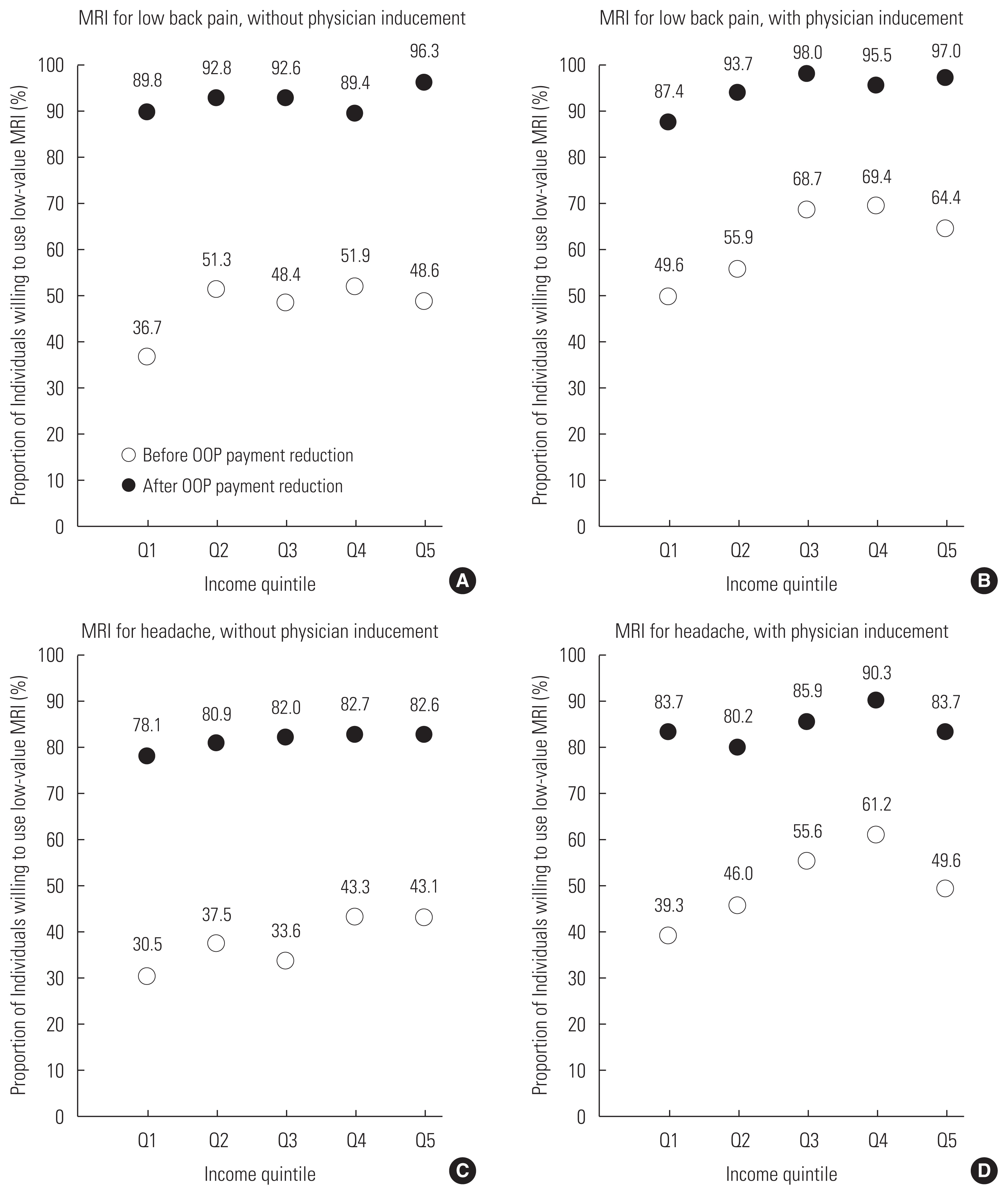
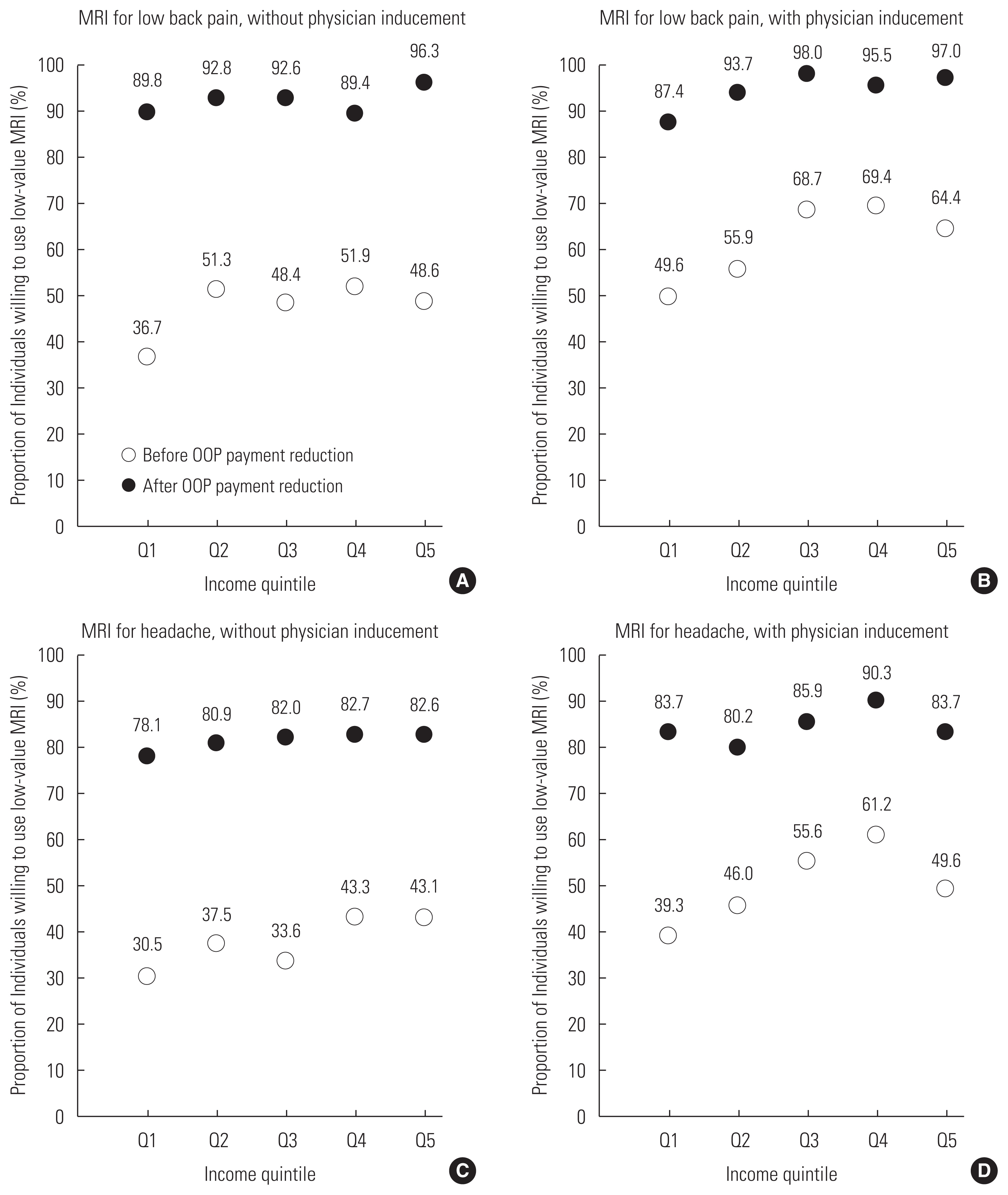
- Before OOP payment reduction, the lowest income quintile was least likely to use low-value MRI regardless of physician inducement (36.7–49.6% for low back pain; 30.5–39.3% for headache). After OOP payment reduction, almost all individuals in each income quintile were willing to use low-value MRI (89.8–98.0% for low back pain; 78.1–90.3% for headache). Absolute and relative inequalities concerning potential low-value MRI utilization decreased after OOP payments were reduced, even without physician inducement (SII: from 8.15 to 5.37%, RII: from 1.20 to 1.06 for low back pain; SII: from 6.99 to 0.83%, RII: from 1.20 to 1.01 for headache).
-
Conclusions
- OOP payment reduction for MRI has the potential to increase low-value care utilization among all income groups while decreasing inequality in low-value care utilization.
- High out-of-pocket (OOP) payment due to services not covered by the Korean National Health Insurance (NHI) raises equity issues since low-income individuals often forgo these services due to their inability to pay [1,2]. Low-income individuals are less likely to use non-covered services compared to high-income individuals in Korea [3,4]. Under the slogan “a nation without hospital bill worries,” the Korean government expanded the scope of insurance coverage to ensure equal financial access to health care and prevent catastrophic health care expenditures. Medical procedures such as brain magnetic resonance imaging (MRI) have had a higher proportion of their costs covered by the NHI since 2018. Between 2017 and 2020, the number of brain MRI scans received by headache patients that were reimbursed by the NHI increased from about 8000 scans to 80 000 scans [5]. Concerns have been raised over excessive MRI utilization by patients with uncomplicated headache and the increased financial burden on the NHI. Although the annual fiscal expenditure of policy implementation was initially expected to total 164 billion Korean won (KRW), the actual expenditure turned out to be 285 billion KRW [6]. The Korean government responded to this issue by raising the threshold for brain MRI coverage in 2020. With the expansion of coverage for spine MRI set for 2022, concerns linger over the issue of MRI overuse due to OOP payment reduction. However, little is known about the effects of OOP payment reduction on low-value care utilization across income groups in Korea.
- Low-value care refers to health care services for which evidence supporting their effectiveness is insufficient or the cost of the service substantially outweighs its benefits [7]. Increased low-value care utilization could lead to incidental findings that result in little additional health benefits, higher health care spending, and an increased risk of complications following additional treatment [8,9]. Although there is a large body of literature examining the effect of cost-sharing on health care utilization, there is little evidence regarding the role of OOP payment reductions on low-value MRI utilization across income groups [10,11]. Several studies provide empirical evidence supporting the claim that increased OOP payment reduces low-value care utilization [12–14]. However, the results seem to depend on specific types of care and the specific clinical context. For example, a previous study found cost-sharing to have no discernable effect on low-value MRI utilization related to headaches and low back pain during emergency room visits in the United States [14]. In addition, these studies did not reveal whether the effect of reduced OOP payment varied according to income. Moreover, this effect could depend on the specific cultural context. While previous studies have provided ample evidence on the effect of OOP payment reductions on increased equity related to health care utilization in Korea, there is little empirical evidence supporting the effect of OOP payment reduction on low-value MRI utilization across income groups [15–19].
- To investigate the effect of OOP payment reduction on low-value MRI utilization across income groups in Korea, researchers could measure the actual rates of low-value care utilization before and after the benefit expansion policy based on health insurance claims data. However, this approach raises methodological issues of causal inference, operationalization, and data availability. Differences in MRI utilization rates among the Korean population before and after policy implementation based on observational data could be confounded by external factors coinciding with the policy implementation. Direct measurements also rely heavily on operational definitions of low-value care, and low-value care that is inconvenient to operationalize is typically excluded from these measurements [20,21]. Lastly, claims data provided by the NHI do not include information on previously non-covered services. Although such information may be available in the databases of individual hospitals, results based on these data would not be generalizable.
- Our study attempted to overcome these challenges by conducting an experimental vignette survey of a representative sample of the Korean population. This method allowed us to define a hypothetical situation in which low-value MRI was undertaken, such as an MRI scan for uncomplicated headache or non-specific low back pain, with fewer restrictions on data availability. Vignettes also allowed us to simulate clinical encounters featuring physician inducement of low-value MRI. Considering the role of physician inducement in the increase in low-value MRI utilization is especially relevant in Korea since the fee-for-service system incentivizes physicians to recommend high-margin services like MRI to patients [22]. Using this methodology, this study aimed to examine the effect of OOP payment reduction on potential low-value MRI utilization across income groups in Korea.
INTRODUCTION
- Participant Characteristics
- An online survey was completed by individuals in Korea from December 24, 2020, to January 5, 2021. The survey used proportional quota sampling to ensure the representativeness of our sample with respect to the population of Korea [23]. We set quotas based on gender, age group (19–29, 30–39, 40–49, 50–59, 60–69 years), and area of residence (17 provinces), based on the resident registration population standards announced by the Ministry of Public Administration and Security in November 2020 (Table S1 in Supplemental Material 1). The age limit of participants was set at 69 years since we assumed that older individuals may lack access to the internet and experience difficulties understanding the survey questions.
- The study team designed the survey and commissioned a public opinion survey company, Gallup Korea, to conduct the survey. An online survey link was sent to 6122 individuals, and 2275 individuals started the survey, with a net response rate of 37.2%. After excluding participants based on our quota, 1304 total individuals participated in the survey, and the survey was closed after the target number of 1200 participants was reached. A total of 1241 individuals completed the survey, resulting in a net completion rate of 95.2%. Twelve participants who did not provide income information were excluded from the analysis, and data from 1229 participants were used in this study.
- Participant characteristics that could be related to low-value care utilization were self-reported through the survey, including income, gender, age, marital status, education, self-rated health status, and comorbidity status (Table 1). Individuals’ income quintiles were calculated based on equivalized income to account for differences in household size. The equivalized monthly income was calculated by dividing the monthly household income by the square root of the number of household members [24].
- Experimental Vignette Design
- We used an experimental vignette design that presented multiple vignettes (within-person design) to two different groups of participants (between-person design) (Supplemental Material 2). This design allowed the researchers to test causal hypotheses regarding the effect of reducing OOP payment on potential low-value care utilization by including factors that are relevant to low-value care, OOP payment reduction, and physician inducement while excluding external factors that might confound the results [25]. The participants were presented with hypothetical scenarios in which they had non-specific low back pain or uncomplicated headache. In the scenario, a physician provided information on the assumed diagnosis, clinical prognosis, further plans, and the OOP payment required to use MRI (spine or brain). The participants were then asked whether they would be willing to use MRI. This vignette was referred to as “before OOP payment reduction.” Those who were unwilling to use MRI were asked if they would use MRI if their OOP payment was reduced. This vignette was referred to as “after OOP payment reduction.” The price of MRI was reduced from 400 000 KRW to 0 KRW through private insurance for low back pain and 600 000 KRW to 100 000 KRW through public insurance for headache. We simulated the reduced price of MRI through private insurance for low back pain to enhance the reality of the situation since the benefit expansion policy had not yet been implemented for spine MRI in 2020 or 2021.
- All scenarios reflected clinical situations in which MRI utilization was considered to be low-value. We referenced Choosing Wisely’s Institute for Clinical and Economic Review Baseline Reports to construct these scenarios [26,27]. To simulate situations in which low-value spine MRI occurs, the vignettes described cases of non-specific low back pain that included, for example, clinical examinations that indicated lumbar sprain or disc herniation, a lack of any progressive neurologic deficit, and treatment plans that included physical therapy and follow-up consultations. For low-value brain MRI, the vignettes described cases of uncomplicated headache, including, for example, clinical examinations indicating uncomplicated headache, improved symptoms through pain medication, persistent headache without sudden onset, headache with moderate severity, and a lack of neurological symptoms indicating a secondary cause.
- To assess the influence of physician inducement on the effect of OOP payment reduction, half of the participants were assigned vignettes in which the physician did not necessarily recommend an MRI scan (n=615). The other half were assigned vignettes in which the physician recommended an MRI scan for further evaluation (n=614). Vignettes in which the physician did not recommend MRI were referred to as “without physician inducement,” and vignettes in which the physician did recommend MRI were referred to as “with physician inducement.”
- Statistical Analysis
- For each vignette, we calculated the proportion of individuals willing to use low-value MRI across income quintiles. Due to the existence of categorical confounders, we used logistic regression and marginal standardization to predict the probabilities of potential low-value MRI utilization for each income quintile [28]. Adjustments were made for gender, age group, marital status, education, self-rated health status, and comorbidity status. Finally, we calculated the slope index of inequality (SII) and relative index of inequality (RII) to assess the income differential related to potential low-value MRI utilization. The adjusted risk difference and adjusted risk ratio between the lowest income quintile and the highest income quintile were estimated using logistic regression, each corresponding to SII and RII, respectively [29,30]. When the log-binomial method fails to converge, logistic regression is a robust method for estimating relative risks and their confidence intervals [31]. Confidence intervals were estimated using the delta method. All statistical analysis was conducted using Stata version 17.0 (StataCorp., College Station, TX, USA).
- Ethics Statement
- This study was approved by the Institutional Review Board of Seoul National University Hospital (IRB No. C-2011-190-1178).
METHODS
- Before OOP payment reduction, the lowest income quintile had the lowest proportion of individuals willing to use low-value MRI (Figure 1). Without physician inducement, only 36.7% (for low back pain) and 30.5% (for headache) of the lowest income quintile preferred to use low-value MRI, compared to 48.6% (for low back pain) and 43.1% (for headache) of the highest income quintile. With physician inducement, potential utilization of low-value MRI became more prevalent, although the lowest income quintile still showed the lowest proportion. Of those in the lowest income quintile, only 49.6% (for low back pain) and 39.3% (for headache) preferred to use low-value MRI with physician inducement, compared to 64.4% (for low back pain) and 49.6% (for headache) of those in the highest income quintile.
- Whether OOP payment reductions would increase low-value MRI utilization did not depend on physician inducement. Almost all individuals in every income quintile reported that they would be willing to use low-value MRI after OOP payment reduction even without physician inducement, ranging from 89.8–96.3% for low back pain and 78.1–82.7% for headache. With physician inducement, OOP payment reduction increased potential low-value MRI utilization for all income groups, ranging from 87.4–98.0% for low back pain and 80.2–90.3% for headache.
- The pattern of predicted probabilities based on logistic regression was consistent with the pattern of unadjusted proportions of potential low-value MRI utilization (Table 2). Those in the lowest income quintile were generally least likely to use low-value MRI before OOP payment reduction, although 95% confidence intervals partially overlapped with those of other income quintiles. With physician inducement, potential low-value MRI utilization was lower for Q1 than Q4 (0.502 vs. 0.646 for low back pain, p<0.05; 0.388 vs. 0.614 for headache, p<0.05). After OOP payment reduction, the difference in potential low-value MRI utilization between Q1 and Q4 was no longer statistically significant even with physician inducement (0.877 vs. 0.971 for low back pain; 0.826 vs. 0.906 for headache).
- Absolute and relative inequalities of potential low-value MRI utilization decreased in magnitude after OOP payment reduction, with or without physician inducement (Table 3). The degree of inequality was greater when there was physician inducement. Without physician inducement, the SII decreased from 8.15% to 5.37% for low back pain and 6.99% to 0.83% for headache, while the RII decreased from 1.20 to 1.06 for low back pain and 1.20 to 1.01 for headache. With physician inducement, the degree to which inequality decreased was larger, with the SII decreasing from 14.40% to 9.42% for low back pain and 10.59% to 1.22% for headache, and the RII decreasing from 1.29 to 1.11 for low back pain and 1.27 to 1.01 for headache.
RESULTS
- Through an experimental vignette survey, this study provided empirical evidence that OOP payment reduction has the potential to increase low-value MRI utilization across all income groups in Korea. While the proportion of potential low-value MRI utilization was lower than 50% in most income groups before OOP payment reduction, a majority of individuals (78.1–98.0%) were willing to use low-value MRI after the price barrier was alleviated. The effect of OOP payment reduction on the change in potential low-value MRI utilization was more prominent among those in low-income groups due to their lower baseline utilization before OOP payment reduction. This resulted in a decrease in both absolute and relative inequality related to potential low-value MRI utilization.
- These findings suggest that low-value MRI utilization after the implementation of the benefit expansion policy poses a real challenge. In response to criticisms over the potential overuse of low-value brain MRI after the implementation of the benefit expansion policy, Korea’s Ministry of Health explained that the 10-fold increase in brain MRI utilization among headache patients was due to the increase in beneficiaries with symptoms that indicate structural brain disease [5]. Our results should in no way be construed to provide an evaluation of the benefit expansion policy in its entirety since we did not measure the change in high-value MRI utilization nor all of the policy’s consequences comprehensively. The benefit expansion policy could be a necessary step toward universal health coverage as it provides more patients with secondary headache access to high-value MRI regardless of their ability to pay. However, our results do suggest that the benefit expansion policy should be coupled with additional policy measures to reduce low-value care across all income groups. Low-value MRI utilization indicates wasteful spending since these diagnostic procedures are unlikely to change the patients’ treatment management or improve their health outcomes [26,27]. Among those covered by Medicare in the United States, neuroimaging for uncomplicated headache was estimated to cost 146 million US dollar (USD) to 211 million USD, while back imaging for patients with non-specific low back pain was estimated to cost 82 million USD to 226 million USD [20]. Although the financial burden posed by low-value care utilization has not been measured in Korea, the near-ceiling effect of OOP payment reduction on potential low-value MRI utilization revealed by our study indicates that the magnitude of wasteful spending could be substantial. Further studies are required to identify the actual cost of low-value MRI in Korea.
- It can be argued that low-value MRI is not reimbursed by the NHI in principle and that the actual increase in low-value care utilization is therefore unlikely to have occurred after the implementation of the benefit expansion policy. Explicit rationing criteria in Korea state that only patients with secondary headache are eligible for reimbursement. Nevertheless, actual application of the rationing criteria depends on each clinical encounter and thus provides room for discretion. Physicians can exercise autonomy due to the subjective nature of the evaluation criteria, such as the duration and character of the patient’s headache and neurological signs observed through examination. Various factors can influence the results of evaluations carried out by physicians. Physicians could be incentivized to expand the margin of eligibility, whether based on financial motives or uncertainty concerning a patient’s condition [32]. Even if physicians initially conclude that MRI is unnecessary, they could be pressured into offering MRI due to patient demand [33,34]. Thus, the existence of explicit rationing criteria is unlikely to be a major source of discrepancy between our results and reality.
- The greater difficulty of reducing low-value MRI utilization through cost-sharing among high-income groups than among low-income groups indicated by our results is also notable. The government announced measures to prevent overuse by introducing a “selective reimbursement” criterion for brain MRI in 2020. Individuals who are suspected of brain disease but do not satisfy base criteria are eligible for reimbursement with a cost-sharing of 80%. According to our study, the effect of cost-sharing is likely to reduce low-value MRI utilization differently across income groups. Although all income groups were less willing to use low-value MRI with higher prices, we observed a pro-rich income gradient of potential low-value MRI utilization before OOP payment reduction, especially with physician inducement. This suggests that individuals with higher incomes are less sensitive to financial constraints imposed by a selective reimbursement policy.
- Our analysis has some limitations. First, respondents’ self-reported willingness to use low-value MRI in our study may differ from their actual willingness and consequent utilization in the clinical environment. Experimental vignette methods are often criticized for showing possible outcomes without necessarily validating the outcomes outside of the experimental environment [25]. Second, measurement errors concerning income data obtained through a survey could further compromise the validity of our results concerning income differences due to cognitive difficulties related to income reporting, the biases of individuals, and random error [35]. Third, the proportional quota sampling used in our study may have not been sufficient to ensure the representativeness of our data since only individuals from panels registered by the survey company were given access to the survey. Further research based on claims data that measures actual income and low-value care utilization rates across the entire population could strengthen the conclusions of this study. Although identifying low-value care utilization based on the current administrative database of the National Health Insurance Service is challenging due to the limited scope of the data, future access to electronic medical records of individual hospitals could enable a more extensive assessment of the value of care being provided.
- Despite these limitations, this is the first study to investigate the relationship between OOP payment reduction and potential low-value MRI utilization across income groups in plausible clinical settings in Korea. Additional policy measures should be undertaken to achieve the dual goal of ensuring financial access to health care services for the poor and reducing wasteful health care utilization and expenditures.
DISCUSSION
SUPPLEMENTAL MATERIALS
-
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
-
FUNDING
This work was funded by the Health Insurance Review and Assessment Service (HIRA) (No. 20210414F59-00).
Notes
ACKNOWLEDGEMENTS
-
AUTHOR CONTRIBUTIONS
Conceptualization: Lee JS, Do YK. Data curation: Lee JS. Formal analysis: Shin Y. Funding acquisition: Do YK. Methodology: Shin Y, Lee JS, Do YK. Writing – original draft: Shin Y. Writing – review & editing: Shin Y, Lee JS, Do YK.
Notes
- 1. OECD. OECD reviews of public health: Korea: a healthier tomorrow; 2020 [cited 2022 Apr 27]. Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/oecd-reviews-of-public-health-korea_be2b7063-en
- 2. Park Y, Park EC. Household out-of-pocket payments and trend in Korea. Health Policy Manag 2019;29(3):374-378. (Korean)
- 3. Lee WY, Shaw I. The impact of out-of-pocket payments on health care inequity: the case of national health insurance in South Korea. Int J Environ Res Public Health 2014;11(7):7304-7318ArticlePubMedPMC
- 4. Jones RS. Health-care reform in Korea. OECD Economics Department Working Papers No. 797. 2010 [cited 2022 Apr 27]. Available from: https://doi.org/10.1787/5kmbhk53x7nt-en Article
- 5. Ministry of Health and Welfare. Benefit expansion of brain MRI does not mean that unnecessary imaging is occurring indiscriminately; 2021 [cited 2022 Apr 27]. Available from: https://www.korea.kr/news/actuallyView.do?newsId=148891860 (Korean)
- 6. Nam I. Press release: fiscal expenditure surges after increase in MRI benefits for brain and cerebrovascular diseases; 2020 [cited 2022 Apr 27]. Available from: https://www.theminjoo.kr/board/view/inspection/341111?st=wrote_post&keyword=%EB%82%A8%EC%9D%B8%EC%88%9C (Korean)
- 7. Colla CH, Mainor AJ, Hargreaves C, Sequist T, Morden N. Interventions aimed at reducing use of low-value health services: a systematic review. Med Care Res Rev 2017;74(5):507-550ArticlePubMedPDF
- 8. Chou R, Fu R, Carrino JA, Deyo RA. Imaging strategies for low-back pain: systematic review and meta-analysis. Lancet 2009;373(9662):463-472ArticlePubMed
- 9. Morris Z, Whiteley WN, Longstreth WT Jr, Weber F, Lee YC, Tsushima Y, et al. Incidental findings on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ 2009;339: b3016ArticlePubMedPMC
- 10. Brook RH, Keeler EB, Lohr KN, Newhouse JP, Ware JE, Rogers WH, et al. The health insurance experiment: a classic RAND study speaks to the current health care reform debate; 2006 [cited 2022 Apr 27]. Available from: https://www.rand.org/pubs/research_briefs/RB9174.html
- 11. Swartz K. Cost-sharing: effects on spending and outcomes. Synth Proj Res Synth Rep 2010;(20):71583PubMed
- 12. Gruber J, Maclean JC, Wright B, Wilkinson E, Volpp KG. The effect of increased cost-sharing on low-value service use. Health Econ 2020;29(10):1180-1201ArticlePubMedPDF
- 13. Shah ND, Naessens JM, Wood DL, Stroebel RJ, Litchy W, Wagie A, et al. Mayo Clinic employees responded to new requirements for cost sharing by reducing possibly unneeded health services use. Health Aff (Millwood) 2011;30(11):2134-2141ArticlePubMed
- 14. Chou SC, Hong AS, Weiner SG, Wharam JF. High-deductible health plans and low-value imaging in the emergency department. Health Serv Res 2021;56(4):709-720ArticlePubMedPMCPDF
- 15. Bae JY. Impacts of health insurance coverage expansion on health care utilization and health status. Korean J Soc Welf Stud 2010;41(2):35-65. (Korean)Article
- 16. Lee YJ. A study on the influences of changes to the co-payment of cancer patients of their uses of medical services. J Korean Public Policy 2009;11(1):3-25. (Korean)
- 17. Kim M, Kwon S. The effect of outpatient cost sharing on health care utilization of the elderly. J Prev Med Public Health 2010;43(6):496-504. (Korean)ArticlePubMed
- 18. Kim E, Kwon S, Xu K. Has income-related inequity in health care utilization and expenditures been improved? Evidence from the Korean National Health and Nutrition Examination Survey of 2005 and 2010. J Prev Med Public Health 2013;46(5):237-248ArticlePubMedPMC
- 19. Kim S, Kwon S. The effect of extension of benefit coverage for cancer patients on health care utilization across different income groups in South Korea. Int J Health Care Finance Econ 2014;14(2):161-177ArticlePubMedPDF
- 20. Schwartz AL, Landon BE, Elshaug AG, Chernew ME, McWilliams JM. Measuring low-value care in Medicare. JAMA Intern Med 2014;174(7):1067-1076ArticlePubMedPMC
- 21. Bhatia RS, Levinson W, Shortt S, Pendrith C, Fric-Shamji E, Kallewaard M, et al. Measuring the effect of Choosing Wisely: an integrated framework to assess campaign impact on low-value care. BMJ Qual Saf 2015;24(8):523-531ArticlePubMed
- 22. Kwon S. Payment system reform for health care providers in Korea. Health Policy Plan 2003;18(1):84-92ArticlePubMed
- 23. Sedgwick P. Proportional quota sampling. BMJ 2012;345: e6336Article
- 24. OECD. Framework for integrated analysis. OECD framework for statistics on the distribution of household income, consumption and wealth; Chpter 8: 2013 [cited 2022 Apr 27]. Available from: https://doi.org/10.1787/9789264194830-11-en Article
- 25. Aguinis H, Bradley KJ. Best practice recommendations for designing and implementing experimental vignette methodology studies. Organ Res Methods 2014;17(4):351-371ArticlePDF
- 26. Reed SJ, Pearson S. Choosing Wisely® recommendation analysis: prioritizing opportunities for reducing inappropriate care: imaging for nonspecific low back pain; 2014 [cited 2022 Apr 27]. Available from: https://www.choosingwisely.org/wp-content/uploads/2015/05/ICER_Low-Back-Pain.pdf
- 27. Reed SJ, Pearson S. Choosing Wisely® recommendation analysis: prioritizing opportunities for reducing inappropriate care: imaging for uncomplicated headache; 2014 [cited 2022 Apr 27]. Available from: https://www.choosingwisely.org/wp-content/uploads/2015/05/ICER_Headache.pdf
- 28. Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol 2014;43(3):962-970ArticlePubMedPMC
- 29. Moreno-Betancur M, Latouche A, Menvielle G, Kunst AE, Rey G. Relative index of inequality and slope index of inequality: a structured regression framework for estimation. Epidemiology 2015;26(4):518-527ArticlePubMed
- 30. Norton EC, Miller MM, Kleinman LC. Computing adjusted risk ratios and risk differences in Stata. Stata J 2013;13(3):492-509ArticlePDF
- 31. Localio AR, Margolis DJ, Berlin JA. Relative risks and confidence intervals were easily computed indirectly from multivariable logistic regression. J Clin Epidemiol 2007;60(9):874-882ArticlePubMed
- 32. Eisenberg JM. Doctors’ decisions and the cost of medical care the reasons for doctors’ practice patterns and ways to change them. Ann Arbor: Health Administration Press; 1986. p. 30-37 p. 61-67
- 33. Sharma S, Traeger AC, Reed B, Hamilton M, O’Connor DA, Hoffmann TC, et al. Clinician and patient beliefs about diagnostic imaging for low back pain: a systematic qualitative evidence synthesis. BMJ Open 2020;10(8):e037820ArticlePubMedPMC
- 34. Jordan JE, Flanders AE. Headache and neuroimaging: why we continue to do it. AJNR Am J Neuroradiol 2020;41(7):1149-1155ArticlePubMedPMC
- 35. Moore JC, Stinson LL, Welniak EJ. Income measurement error in surveys: a review. J Off Stat 2000;16(4):331-362
REFERENCES
Figure & Data
References
Citations

- Socioeconomic inequality in organized and opportunistic screening for colorectal cancer: results from the Korean National Cancer Screening Survey, 2009-2021
Xuan Quy Luu, Kyeongmin Lee, Jae Kwan Jun, Mina Suh, Kui Son Choi
Epidemiology and Health.2023; 45: e2023086. CrossRef
 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite