Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 56(2); 2023 > Article
-
Original Article
The Outcomes of an e-Wellness Program for Lupus Patients in Thailand: A Participatory Action Research Approach -
Nop T. Ratanasiripong1
 , Steven Cahill1
, Steven Cahill1 , Christine Crane1
, Christine Crane1 , Paul Ratanasiripong2
, Paul Ratanasiripong2
-
Journal of Preventive Medicine and Public Health 2023;56(2):154-163.
DOI: https://doi.org/10.3961/jpmph.22.491
Published online: March 9, 2023
1School of Nursing, California State University, Dominguez Hills, Carson, CA, USA
2College of Education, California State University, Long Beach, Long Beach, CA, USA
- Corresponding author: Nop T. Ratanasiripong, School of Nursing, California State University, Dominguez Hills, 1000 East Victoria Street, Carson, CA 90747, USA, E-mail: nratanasiripong@csudh.edu
Copyright © 2023 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- Systemic lupus erythematosus (SLE) or lupus patients usually experience various physical and psychological challenges. Since the coronavirus disease 2019 pandemic, these challenges have become even harsher. Using the participatory action research approach, this study evaluated how an e-wellness program (eWP) impacted SLE-related knowledge and health behaviors, mental health, and quality of life among lupus patients in Thailand.
-
Methods
- A 1-group, pretest-posttest design study was conducted among a purposive sample of lupus patients who were members of Thai SLE Foundation. The 2 main intervention components were: (1) online social support, and (2) lifestyle and stress management workshops. Sixty-eight participants completed all the study requirements, including the Physical and Psychosocial Health Assessment questionnaire.
-
Results
- After being in the eWP for 3 months, participants’ mean score for SLE-related knowledge increased significantly (t=5.3, p< 0.001). The increase in sleep hours was statistically significant (Z=−3.1, p<0.01), with the percentage of participants who slept less than 7 hours decreasing from 52.9% to 29.0%. The percentage of participants reporting sun exposure decreased from 17.7% to 8.8%. The participants also reported significantly lower stress (t(66)= −4.4, p<0.001) and anxiety (t(67)= −2.9, p=0.005). The post-eWP quality of life scores for the pain, planning, intimate relationship, burden to others, emotional health, and fatigue domains also improved significantly (p<0.05).
-
Conclusions
- The overall outcomes showed promising results of improved self-care knowledge, health behaviors, mental health status, and quality of life. It is recommended that the SLE Foundation continues to use the eWP model to help the lupus patient community.
- Lupus (systemic lupus erythematosus, SLE) is a chronic autoimmune disease that causes inflammation in the body. The risk of developing lupus is elevated in young women between the ages of 15 and 44, those with a family history of an autoimmune disease, and people of certain ethnicities [1]. Lupus symptoms vary depending on what organs the autoimmune disorder strikes, but the most common symptoms include painful joints, severe fatigue, skin rash, chest pain, and nephritis [1]. Lupus patients also have nearly a two-fold higher risk of developing resistant high blood pressure than the general population, which subsequently increases the risk of stroke and heart attack [2].
- Worldwide, Black populations have the highest incidence of lupus, followed by Asians, Hispanics, and Caucasians [3]. However, Asians have a higher likelihood of developing lupus nephritis and kidney damage, which are observed in up to 52% of Asians with lupus compared to 13–14% of individuals with lupus in other racial groups [4]. Within Asia, the lupus prevalence varies between 26.5 to 103 per 100 000 individuals [5]. The survival rates for lupus patients in many parts of Asia are lower than in North America and Europe, which is likely attributed to negative socioeconomic factors [6]. In Thailand, a study found that lupus patients with lung inflammation had a greater risk of opportunistic tuberculosis (TB) infection due to the use of immunosuppressive treatments and a higher prevalence of TB in the country [7].
- Several studies have found that lupus symptoms negatively impact patients’ lives, including physical functions, daily activities, mental health, and quality of life. A cross-sectional study of 104 lupus patients found that increased disease activity, fatigue, psychological morbidity, and poor body image were associated with a lower quality of life [8]. A web-based study found that poor mental health, poor physical health, and lower education level were associated with decreased quality of life in lupus patients [9]. A survey of 344 lupus patients found that perceived stress and poor social support were correlated with a lower quality of life, while positive support reduced stress [10]. A study of 140 Thai patients with lupus nephritis found that factors associated with kidney damage included longer disease duration, increased depression, additional disease activities, and poorer self-management [11]. In Thailand, a cross-sectional study found that 15.7% of lupus patients reported moderate to extremely severe depression levels, and 29.4% also reported moderate to extremely severe stress levels. Better lupus-related quality of life was associated with fewer lupus symptoms, lower levels of stress, anxiety, and depression, higher education, and higher income [12].
- The challenges identified by lupus patients in a qualitative study included feelings of shame regarding their appearance in public because of hair loss or side effects from medications, fear of complications in pregnancy, and frustrations regarding family members’ and doctors’ poor understanding of their feelings which, in turn, may exacerbate their sense of isolation [13]. Additionally, the coronavirus disease 2019 (COVID-19) pandemic has troubled lupus patients even more. Since lupus patients have a higher hospitalization rate if they are infected by COVID-19 [14], they may experience more isolation and anxiety due to postponing their medical appointments and avoiding contact with others.
- To prevent flare-ups or the exacerbation of lupus symptoms, a combination of medication treatments (e.g., antimalarials, glucocorticoids, and immunosuppressive agents) [15,16] and lifestyle changes (e.g., adherence to the medication regime, diet, sun exposure limitation, and stress management) should be used [17,18]. Furthermore, physical exercise and psychological interventions have been shown to improve symptoms of fatigue, depression, pain, and quality of life among lupus patients [17,19]. A qualitative study also suggested modifiable factors to enhance lupus patients’ well-being, including improved patient-provider relationship, social support, disease awareness, positive thinking, and stress reduction. Social media or other forms of electronic interaction also showed some promise for filling the human interaction component [13]. Additionally, self-management strategies that produced favorable results included a low-salt diet, rest, exercise, stress reduction, managing medications, health communication, reduction of sun exposure, smoking cessation, and the use of coping skills [11]. Nonetheless, the literature on interventions for lupus patients in Thailand is scarce. One study conducted in 2011 found that, after the provision of health information and a health game about self-care behaviors, Thai adolescent lupus patients had better self-care behaviors [20]. However, the study did not evaluate whether the intervention impacted mental health or quality of life.
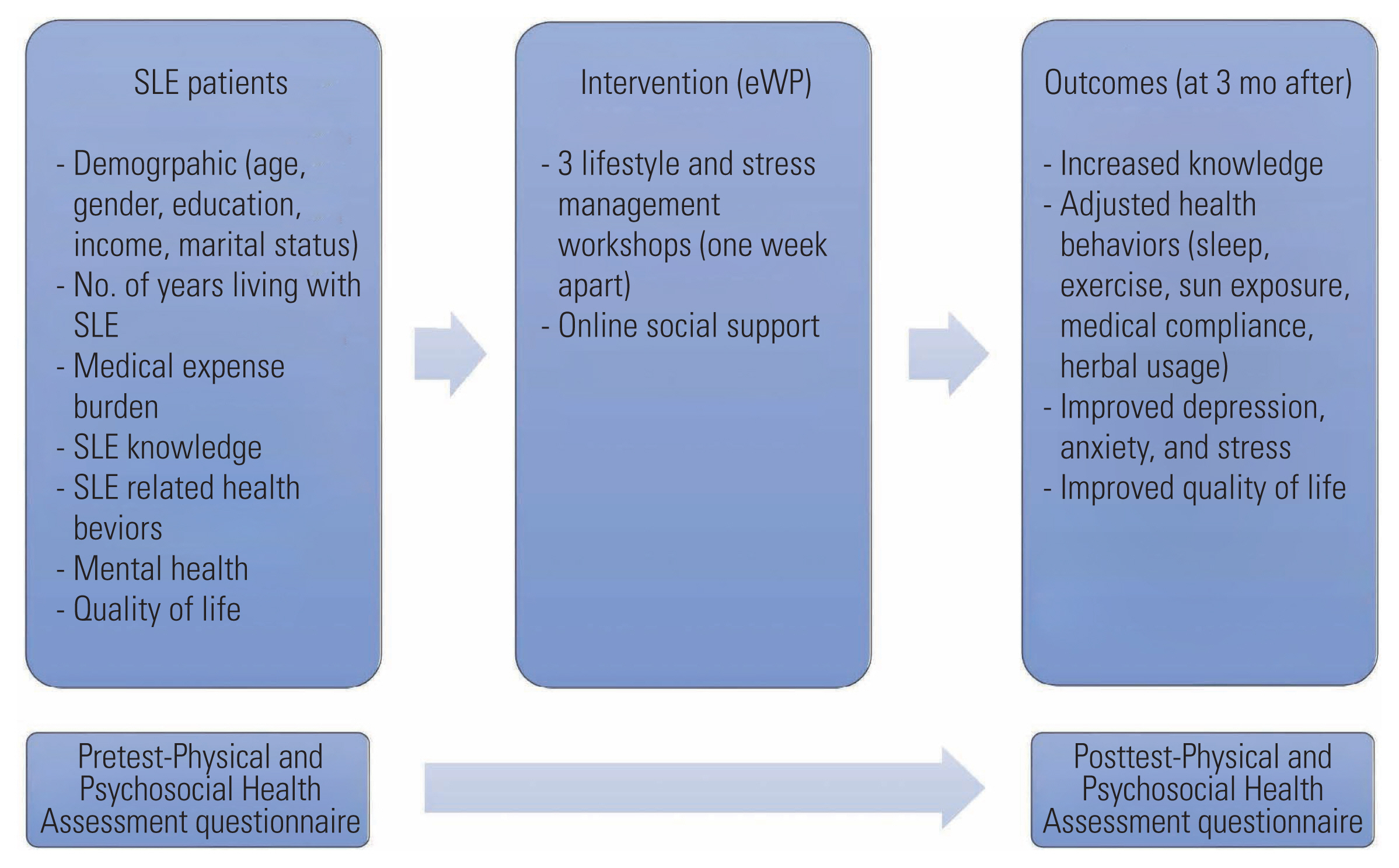
- Participatory action research (PAR) is based on the concepts of reflection, data collection, action, and evaluation to improve health and reduce health inequities by involving people who will improve their own health [21]. In consultation with the SLE Foundation, the largest lupus patient community in Thailand, an e-wellness program (eWP) was created to help support SLE patients during the COVID-19 pandemic, when social distancing was mandatory. Collaborative efforts between the researchers and the foundation leaders were formed with the research question, “What is the impact of the eWP on patients in the Thai SLE community?”. Using the PAR approach, this study aimed to evaluate whether the eWP impacted SLE-related knowledge and health behaviors, mental health, and quality of life among lupus patients in Thailand. The study’s conceptual framework is shown in Figure 1.
INTRODUCTION
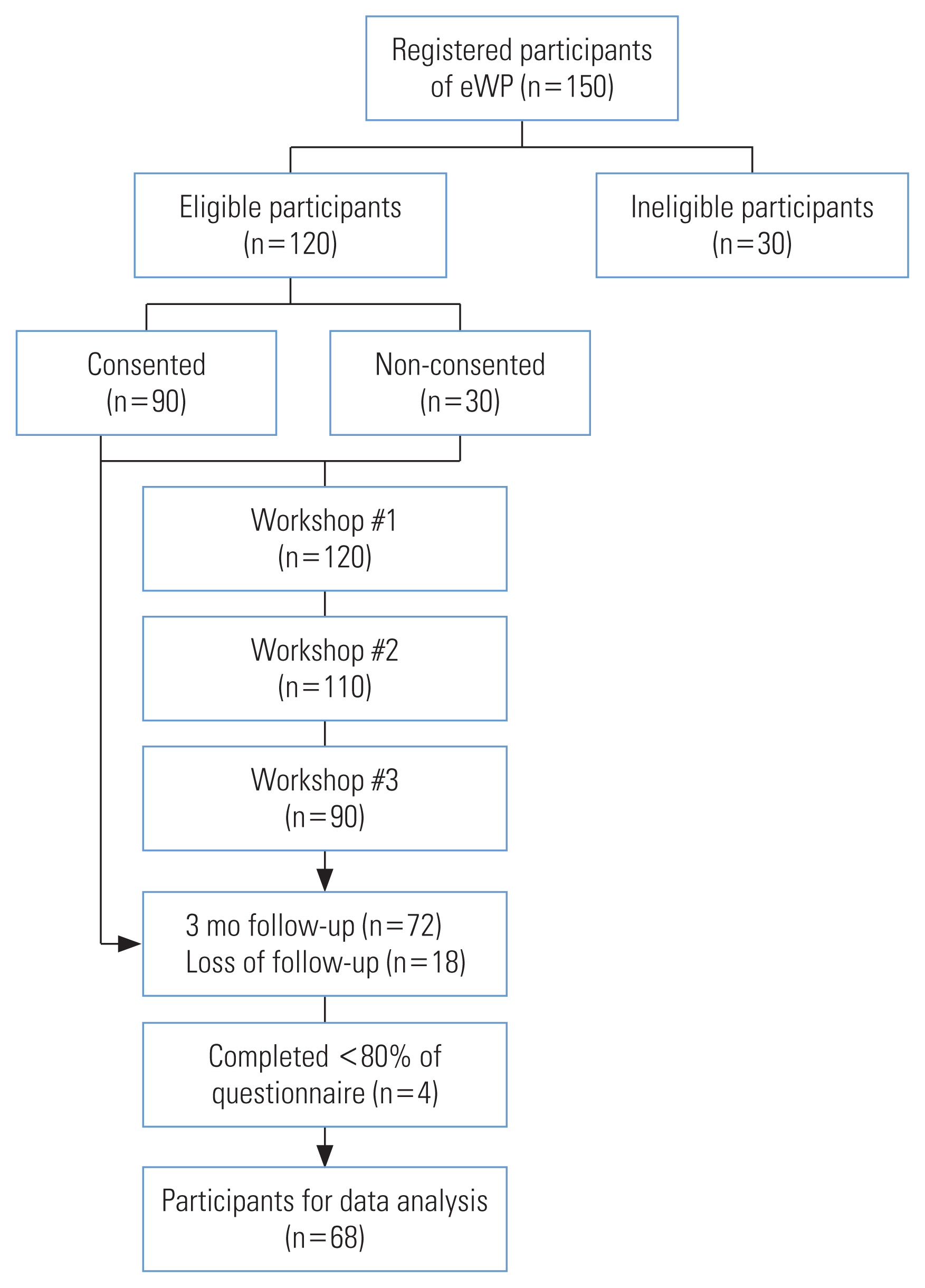
- This 1-group, pretest-posttest design study was conducted from June to October 2021. Using G*Power 3.1 [22], an a priori sample size was calculated for the 2-tailed, paired t-test using an effect size of 0.3, alpha of 0.05, and power of 0.8; it was calculated that 90 participants would be needed. Since an effect size from previous SLE-related intervention studies was not found, d=0.3 was used because the effect sizes in the social sciences are typically smaller than 0.3 [23].
- Study Participants and Setting
- There were 150 people registered with the eWP after the invitation was posted on the Thai SLE Foundation Facebook page. Purposive sampling was used to select registrants who met the inclusion criteria (i.e., at least 18 years old, able to read and write Thai, and having been diagnosed with lupus by a physician). Registrants were excluded from the study if they had a severe mental illness (lupus psychosis) or disabilities preventing them from completing the questionnaire.
- Procedure and Measurements
- Ninety out of the 120 qualified registrants consented to participate and completed the Physical and Psychosocial Health Assessment (PPHA) questionnaire via Alchemer (a survey vendor). The rest preferred to attend the eWP without participating in the study. The PPHA questionnaire consisted of:
Demographic and health history, including 7 questions on age, gender, education, income, relationship status, medical expense burden, and initial date of diagnosis.
SLE-related knowledge and behaviors, with questions developed based on a literature review. Face validation was conducted with 10 lupus patients. Content validation was done by two rheumatologists. There were 10 SLE-related knowledge and 7 health behavioral questions including daily sleep duration, exercise frequency, exercise duration, sun exposure, medication compliance (forgetting and stopping medications), and the use of herbs.
The Depression, Anxiety, and Stress Scales (DASS-Thai version), which contained three subscales with 7 items each [24]. Participants were asked to rank their feelings within the last week on a scale from 0 (did not apply to me) to 3 (applied to me very much or most of the time). Consistent with previous studies [12,25], Cronbach’s alpha values were good for the depression subscale (0.87), anxiety subscale (0.75), and stress subscale (0.83).
_The Lupus Quality of Life Scale (LupusQoL-Thai version), which contained 34 items measuring 8 domains including physical health, planning, pain, intimate relationship, burden to others, emotional health, body image, and fatigue [26]. The answers were scored on a scale of 0 (always) to 4 (not at all). The transformed score was found by taking each domain’s average score divided by 4 and multiplying by 100. The scores ranged from 0 (worst) to 100 (best). Similar to the previous studies [12,25], Cronbach’s alpha of each domain was good, with a range of 0.71–0.93.
- The 2 main components of the intervention included:
Social support: All registrants were added to an online support group via the Line smartphone application, a popular social media platform in Thailand. The online support group was led and monitored by 2 Thai SLE Foundation leaders who have lived with lupus for at least 10 years.
Lifestyle and stress management: After being trained to use Zoom, the registrants attended three 90-minute weekly online workshops via Zoom. The workshop content was based on findings from previous studies conducted by the researchers [12,25] and input from the SLE Foundation leaders. The week #1 workshop focused on SLE diagnosis and treatments. The week #2 workshop focused on self-management (e.g., diet, exercise, elimination, environment, and hygiene). The week #3 workshop focused on mental health management and resources. The workshops were recorded and posted to the Foundation’s YouTube channel for those who wished to review them later. The number of attendants in each workshop is presented in Figure 2.
- Three months after the last eWP workshop, 72 participants out of 90 participants completed the PPHA questionnaire again (except for the demographic and health history questions) and received a 45 mL tube of sunscreen as a token. The data from 68 participants were used for analysis after excluding 4 with more than 20% missing answers. When using non-parametric tests to check for the differences in demographic characteristics (age, gender, education, income, relationship status), there were no statistically significant differences between those who completed the eWP and those who did not. There were also no differences between those who completed less than 80% of the questionnaire and the rest.
- Statistical Analysis
- SPSS version 28.0 (IBM Corp., Armonk, NY, USA) was utilized for data analysis. Descriptive statistics were used to present the demographic characteristics and the variables of interest. After checking the assumptions (at least 30 pairs and the skewness scores not exceeding +/−1) [27], the paired t-test was used to examine differences between the pre-eWP and post-eWP scores of SLE knowledge, mental health, and quality of life. The Wilcoxon signed-rank test was used to evaluate the significance of differences between pre-eWP and post-eWP health behaviors (ordinal variables).
- Ethics Statement
- This study received approval from California State University, Dominguez Hills Ethics Committee (IRB #21-152). Participants initialed the e-consent form before completing the questionnaire. Participants were informed that they could withdraw from the study at any time.
METHODS
Pretest
Intervention
Post-test
- Demographics
- All participants were women, with an average age of 37.3 years old (standard deviation [SD], 8.7; range, 20–53). Most participants (80.9%) had earned at least a bachelor’s degree. Many participants were in a relationship: married (45.6%) or dating (25.0%). The majority (76.5%) reported that they had either sufficient income or savings, while 23.5% of the participants did not have sufficient income. When asked to rate their burden in terms of SLE-related medical expenses (0=no burden, 10=excessive burden), 67.2% of the participants gave a rating between 0 points and 5 points, while 32.8% of them rated their burden as between 6 points and 10 points (mean±SD, 4.7±2.6). On average, the participants had been diagnosed with SLE for 6.3 years (range, 2 months to 37 years).
- Knowledge
- The percentages of the participants who gave correct answers for each question are shown in Table 1. As indicated in the pre-eWP scores, participants lacked the most knowledge on vaccinations, birth control methods, and pregnancy. Participants’ post-test knowledge improved, except for the vaccination and stress questions. When using the paired t-test to analyze further, there was a significant increase in SLE knowledge after the eWP (8.5±1.1) compared to before the eWP (7.5±1.7; t(67)=5.3; p<0.001).
- Systemic Lupus Erythematosus-related Health Behaviors
- As shown in Table 1, the percentage of the participants who slept less than 7 hr/day decreased from 52.9% to 29.0%. The Wilcoxon signed-rank test indicated that the post-eWP daily sleep duration was significantly higher than the pre-eWP daily sleep duration (Z=−3.1, p=0.002).
- Most participants exercised no more than 3 day/wk before and after the eWP (83.9 and 86.8%, respectively). Although the proportion of participants with a duration of exercise of ≥45 minutes increased from 47.7% to 53.0%, the change was not statistically significant.
- Before the eWP, 17.7% of the participants reported exposure to sunlight between 10:00–16:00 without sunscreen or long-sleeve clothing for more than 3 day/wk. After the eWP, this percentage decreased to 8.8%. However, this change was not statistically significant.
- The percentage of participants forgetting to take medications more than 1 day/wk decreased from 19.1% to 11.8%. This change, however, was not statistically significant. Eight participants reported that they previously stopped taking medications at one point without consulting a doctor. Since they attended the eWP, they had not done so.
- Before the eWP, 6 participants reported using herbs that were not prescribed by a doctor, and 5 of them did not inform the doctor about it. After the eWP, 2 participants reported using herbs without informing a doctor.
- Mental Health
- Before the eWP, based on the DASS recommended cut-off scores for categorizing the severity [24], 11.7% of the participants were potentially at risk of having severe or extremely severe stress levels. Approximately 32.4% of them reported having severe or extremely severe anxiety levels, and 10.3% of them reported having severe or extremely severe depression levels. Overall, the participants reported significantly less stress and anxiety 3 months after the eWP concluded. For depression, while the mean score decreased after the eWP, the change was not statistically significant (Table 2).
- Systemic Lupus Erythematosus-related Quality of Life
- All domains of SLE-related quality of life were impacted (Table 3). Before the eWP, the most impacted domains were intimate relationship, fatigue, burden to others, and body image. After the eWP, each domain score improved except the body image domain. The paired t-test showed that the quality of life domains of pain, planning, intimate relationship, emotional health, and fatigue improved significantly (p<0.05).
RESULTS
Daily sleep duration
Exercise
Sun exposure
Medication compliance
Using herbs
- The study participants were all women, congruent with the previous striking finding of a 9:1 women-to-men ratio of SLE prevalence [1]. While approximately three-quarters of participants reported higher than average education among Thais [28] and had sufficient income, a third of them (32.8%) felt the burden of medical expenses, which subsequently might impact their mental health and treatment compliance.
- Before the eWP, all participants already knew that SLE patients may manifest symptoms and that stress worsens lupus symptoms, but many of them lacked knowledge regarding the impact of pregnancy, birth control options, and vaccinations. Overall, the participants’ knowledge increased significantly after they attended the eWP. Most understood that lupus is an incurable, non-contagious disease that might worsen if they become pregnant. They were also aware that they should not stop taking medications or start taking any herbal medicine or contraceptives without consulting their physician. However, many still did not know that they may not get vaccines at any time they want.
- When examining changes in health behaviors, this study found a significantly increased daily sleep duration after the eWP concluded. While not statistically significant, other desirable changes were also noticed, including a decrease in sun exposure and an increase in treatment compliance. This finding is similar to another study reporting that a health education-based intervention improved lupus patients’ knowledge (e.g., risk factors, signs/symptoms, treatments, complications) and self-care behaviors, such as avoiding risks and medical compliance [29]. For exercise, the study participants reported a decrease in exercise frequency which coincided with another study that reported lower physical activity during the pandemic [30]. A new idea to motivate lupus patients to exercise indoors could be beneficial for this population, as a systematic review supported that an exercise intervention compared to usual care increased quality of life, especially in the physical functioning domain [31].
- Interestingly, despite the COVID-19 pandemic, the mean scores for stress, anxiety, and depression were comparable to the mean scores from a 2019 study [12]. After the eWP, the participants reported decreases in stress, anxiety, and depression scores. This result suggests that lifestyle and stress management workshops might increase patients’ understanding of the disease and provide ideas on how to handle stress (e.g., positive thinking or deep breathing), which in turn improves mental health status. Specifically, using the e-support group might have provided a social network and peer support that the patients needed to deal with this chronic disease [32].
- Consistent with a previous web-based study [12], the participants reported that all SLE-related quality of life domains were diminished, with the intimate relationship, fatigue, burden to others, and body image domains being impacted the most. After the eWP, the domains of pain, planning, intimate relationship, emotional health, and fatigue improved significantly. This outcome is congruent with previous systematic reviews, which reported that diet, exercise intervention, and psychological interventions such as biofeedback with a relaxation technique or psychoeducation helped improve at least 1 domain of quality of life such as pain and fatigue [17,18]. For body image, the domain score might have worsened due to autoimmune-caused skin rashes, especially on the face, disfigured joints, and hair loss. Furthermore, medications such as chemotherapy or steroids might cause weight gain and darken skin color. Until the disease is under control, patients need time to adjust and accept these changes [33]. Long-term follow-up might be more appropriate to see changes in this domain.
- As the study outcomes were discussed with the SLE Foundation leaders to empower the community, the Foundation has established the “Friends Helping Friends” program to elevate the financial burden for patients who cannot afford travel expenses to follow up with their doctors. This program is funded by SLE patients and families in the community. Other recommendations to the Foundation included improving the eWP model by (1) adding more details on vaccinations, pregnancy, and birth control options in the self-care workshops; (2) creating online indoor exercise programs by using volunteer leaders (e.g., a yoga trainer or aerobic dancer); and (3) offering activities to help patients increase their self-image, such as online cosmetic training [34]. In addition, a similar face-to-face wellness program may be offered at major hospitals in Thailand to lupus patients who do not have Internet access.
- This is the first intervention study conducted among adult lupus patients in Thailand. The project also showed how healthcare providers could collaborate with the community of interest to help lupus patients creatively during the COVID-19 pandemic. However, the generalizability is limited to lupus patients who have Internet access. Other study limitations include (1) selection bias, insofar as the program involved individuals with high motivation to improve their health; (2) the Hawthorne effect, according to which the participants might change their behaviors due to being observed, not because of the intervention’s effectiveness [35]; (3) self-reporting bias; (4) attrition bias, which might have occurred if participants withdrew from the study due to a lack of satisfaction with the eWP (although the loss to follow-up rate of 20% was acceptable [36]); and (5) the inability to assume a causal effect due to the lack of a control group. For future research, a randomized controlled trial is advisable. Long-term follow-ups at 6 months and 12 months may also be worth the time and resources.
- In conclusion, the eWP showed promising outcomes of improved SLE-related knowledge and health behaviors, better mental health status, and enhanced quality of life. It also provided an alternative and innovative approach to help SLE patients manage their health. It would be beneficial if healthcare providers work collaboratively with communities such as the SLE Foundation in expanding and offering the eWP to more lupus patients to maximize their quality of life while they try to live with the condition.
DISCUSSION
-
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
-
FUNDING
This study was supported by a Research, Scholarly, and Creative Activity grant from California State University, Dominguez Hills, USA.
-
AUTHOR CONTRIBUTIONS
Conceptualization: Ratanasiripong NT, Ratanasiripong P. Data curation: Ratanasiripong NT. Formal analysis: Ratanasiripong NT. Funding acquisition: Ratanasiripong NT. Methodology: Ratanasiripong NT. Project administration: Ratanasiripong NT, Ratanasiripong P. Visualization: Ratanasiripong NT, Crane C, Ratanasiripong P. Writing – original draft: Ratanasiripong NT, Cahill S, Crane C. Writing – review & editing: Ratanasiripong NT, Cahill S, Crane C, Ratanasiripong P.
Notes
ACKNOWLEDGEMENTS
- 1. Lupus Foundation of America. What is lupus?; [cited 2022 Oct 21]. Available from: https://www.lupus.org/resources/what-is-lupus
- 2. Gandelman JS, Khan OA, Shuey MM, Neal JE, McNeer E, Dickson A, et al. Increased incidence of resistant hypertension in patients with systemic lupus erythematosus: a retrospective cohort study. Arthritis Care Res (Hoboken) 2020;72(4):534-543ArticlePubMedPMCPDF
- 3. Rees F, Doherty M, Grainge MJ, Lanyon P, Zhang W. The worldwide incidence and prevalence of systemic lupus erythematosus: a systematic review of epidemiological studies. Rheumatology (Oxford) 2017;56(11):1945-1961ArticlePubMed
- 4. Drenkard C, Lim SS. Update on lupus epidemiology: advancing health disparities research through the study of minority populations. Curr Opin Rheumatol 2019;31(6):689-696ArticlePubMedPMC
- 5. Barber MR, Drenkard C, Falasinnu T, Hoi A, Mak A, Kow NY, et al. Global epidemiology of systemic lupus erythematosus. Nat Rev Rheumatol 2021;17(9):515-532ArticlePubMedPMCPDF
- 6. Carter EE, Barr SG, Clarke AE. The global burden of SLE: prevalence, health disparities and socioeconomic impact. Nat Rev Rheumatol 2016;12(10):605-620ArticlePubMedPDF
- 7. Palavutitotai N, Buppajarntham T, Katchamart W. Etiologies and outcomes of pleural effusions in patients with systemic lupus erythematosus. J Clin Rheumatol 2014;20(8):418-421ArticlePubMed
- 8. Pereira MG, Duarte S, Ferraz A, Santos M, Fontes L. Quality of life in patients with systemic lupus erythematosus: the mediator role of psychological morbidity and disease activity. Psychol Health Med 2020;25(10):1247-1257ArticlePubMed
- 9. Delis PC. Uncertainty and quality of life in systemic lupus erythematosus: a cross-sectional study. Rehabil Nurs 2019;44(1):2-10ArticlePubMed
- 10. Mazzoni D, Cicognani E. Positive and problematic support, stress and quality of life in patients with systemic lupus erythematosus. Anxiety Stress Coping 2016;29(5):542-551ArticlePubMed
- 11. Lertwongpaopun W, Tilokskulchai F, Sindhu S, Pattaragan A, Chai-Aroon T. Factors associated with kidney damage among Thais with lupus nephritis. Pac Rim Int J Nurs Res Thail 2016;20(4):309-319
- 12. Ratanasiripong NT, Ratanasiripong P. Predictive factors of quality of life among systemic lupus erythematosus patients in Thailand: a web-based cross-sectional study. Qual Life Res 2020;29(9):2415-2423ArticlePubMedPDF
- 13. Case S, Sinnette C, Phillip C, Grosgogeat C, Costenbader KH, Leatherwood C, et al. Patient experiences and strategies for coping with SLE: a qualitative study. Lupus 2021;30(9):1405-1414ArticlePubMedPDF
- 14. Fernandez-Ruiz R, Masson M, Kim MY, Myers B, Haberman RH, Castillo R, et al. Leveraging the United States epicenter to provide insights on COVID-19 in patients with systemic lupus erythematosus. Arthritis Rheumatol 2020;72(12):1971-1980ArticlePubMedPMCPDF
- 15. Tselios K, Gladman DD, Touma Z, Su J, Anderson N, Urowitz MB. Clinical remission and low disease activity outcomes over 10 years in systemic lupus erythematosus. Arthritis Care Res (Hoboken) 2019;71(6):822-828ArticlePubMedPDF
- 16. Tselios K, Gladman DD, Touma Z, Su J, Anderson N, Urowitz MB. Disease course patterns in systemic lupus erythematosus. Lupus 2019;28(1):114-122ArticlePubMedPDF
- 17. Fangtham M, Kasturi S, Bannuru RR, Nash JL, Wang C. Non-pharmacologic therapies for systemic lupus erythematosus. Lupus 2019;28(6):703-712ArticlePubMedPMCPDF
- 18. Chang A, Winquist NW, Wescott AB, Lattie EG, Graham AK. Systematic review of digital and non-digital non-pharmacological interventions that target quality of life and psychological outcomes in adults with systemic lupus erythematosus. Lupus 2021;30(7):1058-1077ArticlePubMedPMCPDF
- 19. da Hora TC, Lima K, Maciel RR. The effect of therapies on the quality of life of patients with systemic lupus erythematosus: a meta-analysis of randomized trials. Adv Rheumatol 2019;59(1):34ArticlePubMedPDF
- 20. Nabundit R, Tangvoraphonkchai J. The effects of innovation in providing health information and health game on self-care behaviors for adolescent SLE patients admitted in hospital. J Nurs Sci Health 2012;35(1):10-17. (Thai)
- 21. Baum F, MacDougall C, Smith D. Participatory action research. J Epidemiol Community Health 2006;60(10):854-857ArticlePubMedPMC
- 22. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39(2):175-191ArticlePubMedPDF
- 23. Ferguson CJ. An effect size primer: a guide for clinicians and researchers. Prof Psychol Res Pract 2009;40(5):532-538Article
- 24. Lovibond SH, Lovibond PF. Manual of the depression anxiety stress scales. 2nd ed. Sydney: Psychology Foundation; 1995. p. 1-42
- 25. Ratanasiripong N, Warawitsaranggoon R, Junda T, Sangchan H, Goo PA, Siripaitoon B, et al. Mental health status and health-related quality of life among systemic lupus erythematosus (SLE) patients in Thailand: a multi-site study. J Med Assoc Thai 2020;103(11):1185-1193Article
- 26. RWS Life Sciences. LupusQoL scale; [cited 2022 Oct 18]. Available from https://lifesciences.rws.com/lupusqol/instrument-information/instrument-scoring
- 27. Plichta SB, Kelvin EA. Munro’s statistical methods for health care research. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2013. p. 130-137
- 28. United States Agency for International Development (USAID). International data & economic analysis. Thailand general education; [cited 2022 Oct 11]. Available from: https://idea.usaid.gov/cd/thailand/education
- 29. Elsayed D, Mesbah S. Effect of health education based intervention on self-care among systemic lupus erythematosus clients. Am J Nurs Res 2018;6(3):105-112Article
- 30. Puccinelli PJ, da Costa TS, Seffrin A, de Lira CA, Vancini RL, Nikolaidis PT, et al. Correction to: reduced level of physical activity during COVID-19 pandemic is associated with depression and anxiety levels: an internet-based survey. BMC Public Health 2021;21(1):613ArticlePubMedPMCPDF
- 31. Lu MC, Koo M. Effects of exercise intervention on health-related quality of life in patients with systemic lupus erythematosus: a systematic review and meta-analysis of controlled trials. Healthcare (Basel) 2021;9(9):1215ArticlePubMedPMC
- 32. Williams EM, Egede L, Faith T, Oates J. Effective self-management interventions for patients with lupus: potential impact of peer mentoring. Am J Med Sci 2017;353(6):580-592ArticlePubMedPMC
- 33. Rodrigues L, Sim-Sim MM, Sousa L, Faria-Schützer DB, Surita FG. Self-concept and body image of people living with lupus: a systematic review. Int J Rheum Dis 2021;24(11):1339-1353ArticlePubMedPDF
- 34. Jolly M, Peters KF, Mikolaitis R, Evans-Raoul K, Block JA. Body image intervention to improve health outcomes in lupus: a pilot study. J Clin Rheumatol 2014;20(8):403-410PubMed
- 35. Polit DF, Beck CT. Nursing research: generating and assessing evidence for nursing practice. 10th ed. Philadelphia: Wolters Kluwer Health; 2017. p. 197
- 36. Hewitt CE, Kumaravel B, Dumville JC, Torgerson DJ; Trial attrition study group. Assessing the impact of attrition in randomized controlled trials. J Clin Epidemiol 2010;63(11):1264-1270ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Positive psychological capital, post-traumatic growth, social support, and quality of life in patients with systemic lupus erythematosus: A cross-sectional study
Lyu Meng, Cui-Rong Gao, Hui-Cai Wang, Raxida Yasin, Rui-Jie Huang, Yu-Xin Zhao, Xiao-Hui Ma, Yuan-Yuan Wen
Lupus.2024; 33(5): 470. CrossRef
 KSPM
KSPM


 PubReader
PubReader ePub Link
ePub Link Cite
Cite