Our research offers an in-depth analysis of the barriers and challenges faced by human immunodeficiency virus (HIV)-positive pregnant women in accessing HIV services and treatment in Kupang City of East Nusa Tenggara Province in Indonesia. The barriers and challenges identified include a lack of understanding of the benefits of antiretroviral (ARV) drugs; difficulties in accessing ARV treatment services due to factors such as distance, time, and cost; incomplete administrative requirements such as a national ID card (Kartu Tanda Penduduk), family card (Kartu Keluarga), or national health insurance (Badan Penyelenggara Jaminan Sosial); drug side effects; and enduring stigma from both within and outside their immediate environment. Furthermore, these women face procedural difficulties during treatment in health services and often lack family support [1]. The importance of psychosocial support in enabling HIV-positive pregnant women to regularly access ARV services and treatment is evident [2]. One form of support that can be provided is the involvement of women living with HIV as peer supporters to assist HIV-positive pregnant women throughout their pregnancy. Our previous research indicated that HIV-positive pregnant women who did not receive help from peer mentors were 2.96 times more likely to face difficulties in accessing ARV treatment services compared to those who did receive assistance [3].
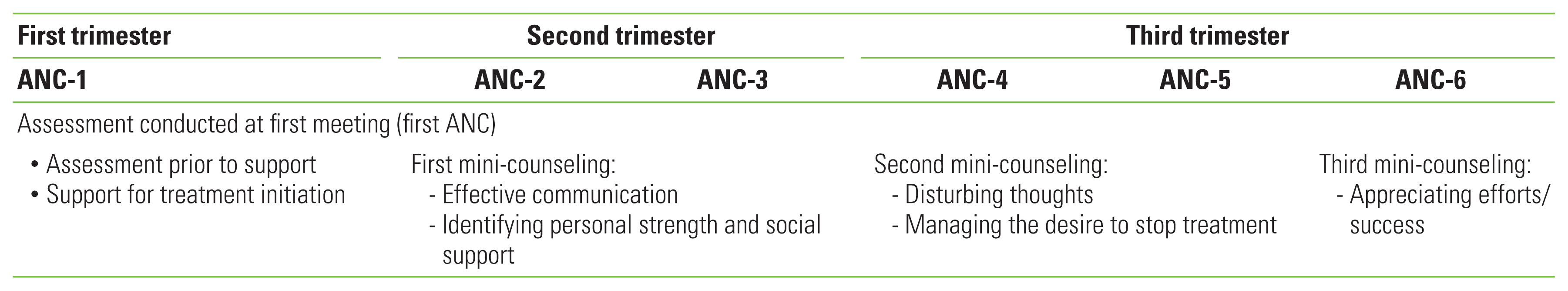
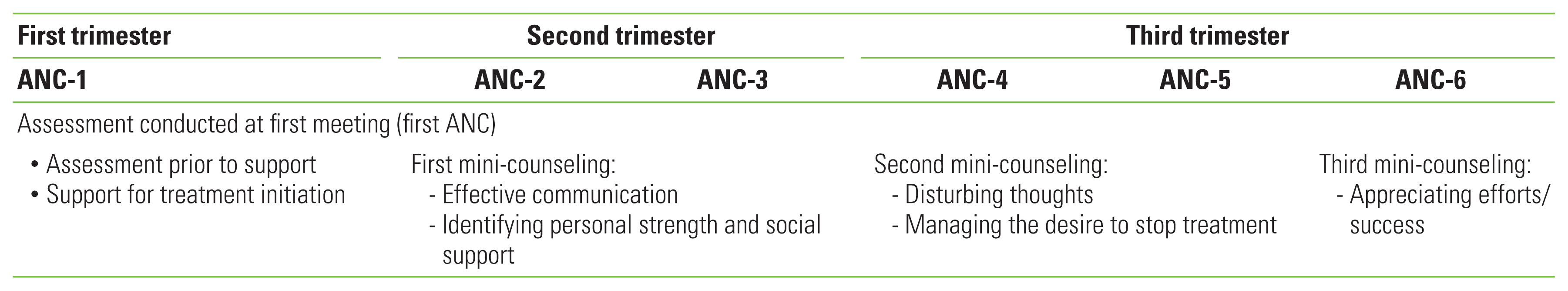
We have developed a structured support model for HIV-positive pregnant women, based on the key barriers and challenges they face. This model was created in collaboration with cross-sector stakeholders, including women living with HIV from local Civil Society Organizations such as the Indonesian Positive Women Association of Kupang City and the Flobamora Foundation, health workers from primary health centers (midwives, HIV program coordinators), professional associations (midwives association, obstetric gynecologists and pediatrician associations), the Kupang City Health Office, and the Civil Registration Office (Dukcapil). The model outlines steps for an initial assessment and for overcoming administrative barriers before implementation, ensuring that all pregnant women with HIV can access services. The structured mentoring model is implemented by trained peer supporters or mentors and is integrated into antenatal care services, aligning with the antenatal care (ANC) schedule. During the support period, the peer supporter or mentor will provide assistance in line with the ANC schedule, for a minimum of five times. This includes an initial and final assessment, as well as three mini-counseling sessions (30–45 minutes per session) based on pre-determined topics using flipcharts. These flipcharts contain information about HIV, its transmission, prevention, and treatment, as well as counseling information to aid the pregnant women. This peer support is provided for a minimum of 6 months or until the mothers give birth.
The first counseling session takes place after the pregnant woman has a meeting with assigned peer supporter/mentor, facilitated by health workers at the community health center (Puskesmas). During this initial meeting, an assessment is conducted to evaluate the mother’s knowledge, perceptions, and understanding of HIV transmission, treatment, and care. The mother’s physical, emotional, and socioeconomic conditions are also evaluated. This is followed by setting a date for the next meeting or counseling session. The counseling focuses on three main psychosocial themes identified during the research: building effective communication, identifying personal and social support, and managing disturbing thoughts. It also addresses managing the desire to stop therapy and presents appreciation for their motivation to continue with the ARV treatment (Figure 1).
Peer supporters or mentors offer psychosocial support to HIV-positive pregnant women and their families. They provide education and information about HIV, with the goal of enhancing family knowledge and acceptance of the HIV-positive status of pregnant women. This, in turn, encourages mothers to pursue treatment and improve adherence. Collaborating with healthcare facilities and staff can bolster this mentoring model. In this model, peer supporters or mentors, pregnant women and their families, and healthcare workers all function as a community, fostering a supportive environment. Interventions, structured and integrated with ANC, can boost motivation, enhance social support, and diminish stigma-related behaviors that prevent HIV-positive pregnant women from accessing services and treatment. This approach has the potential to increase self-acceptance, making mothers more likely to take ARV medication and stick to their treatment plan. Counseling sessions, when integrated with routine ANC checks, can minimize loss to follow-up and ensure that mothers adhere to HIV treatment and care throughout their pregnancy and up to delivery. Adherence to ARV therapy is crucial for suppressing the replication of the HIV virus until it becomes undetectable, thereby preventing mother-to-child transmission.
Notes
-
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
Figure 1Format of peer support mentoring and counseling. ANC, antenatal care.
REFERENCES
- 1. Camellia A, Swandari P, Rahma G, Merati TP, Bakta IM, Duarsa DP. A peer-support mini-counseling model to improve treatment in hiv-positive pregnant women in Kupang City, East Nusa Tenggara, Indonesia. J Prev Med Public Health 2023;56(3):238-247ArticlePubMedPMCPDF
- 2. Sawitri AA, Sutarsa IN, Merati TP, Bakta M, Nyoman D. Perceptions dynamics about antiretroviral treatment among HIV patients in Bali. Int J Public Health Sci 2021;10(3):500-507ArticlePDF
- 3. Camellia A, Swandari P, Irwanto Irwanto GR, Merati TP. Peer facilitators’s role to support pregnant women in utilizing HIV services during the COVID-19 pandemic. Int J Public Health Sci 2023;12(1):377-384ArticlePDF
Citations
Citations to this article as recorded by

 , Gusni Rahma2
, Gusni Rahma2


 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


