Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 57(1); 2024 > Article
-
Original Article
Relationship Between Pesticide Exposure Factors and Health Symptoms Among Chili Farmers in Northeast Thailand -
Ratchadaporn Pengpan1
 , Kulthida Y. Kopolrat1
, Kulthida Y. Kopolrat1 , Sribud Srichaijaroonpong1
, Sribud Srichaijaroonpong1 , Nutta Taneepanichskul2
, Nutta Taneepanichskul2 , Patiwat Yasaka3
, Patiwat Yasaka3 , Ratanee Kammoolkon1
, Ratanee Kammoolkon1

-
Journal of Preventive Medicine and Public Health 2024;57(1):73-82.
DOI: https://doi.org/10.3961/jpmph.23.353
Published online: December 20, 2023
1Faculty of Public Health, Kasetsart University Chalermphrakiat Sakon Nakhon Province Campus, Sakon Nakhon, Thailand
2College of Public Health Sciences, Chulalongkorn University, Bangkok, Thailand
3Faculty of Management Technology, Rajamangala University of Technology Isan, Surin Campus, Surin, Thailand
- Corresponding author: Ratanee Kammoolkon, Faculty of Public Health, Kasetsart University Chalermphrakiat Sakon Nakhon Province Campus, 59 Moo 1, Chiangkhruea Subdistrict, Sakon Nakhon 47000, Thailand E-mail: rattanee.k@ku.th
Copyright © 2024 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives:
- The unsafe use of pesticides in agriculture represents a major hazard to human health. This study was conducted to investigate the association between pesticide exposure and health symptoms among chili farmers in northeast Thailand.
-
Methods:
- This cross-sectional analytic study included 141 chili farmers in Sakon Nakhon Province, in northeast Thailand. Data regarding health symptoms were gathered using a self-report questionnaire. A medical technician tested blood cholinesterase activity using an erythrocyte method, and an occupational medicine specialist at Ramathibodi Hospital in Bangkok, Thailand reviewed the results. Associations between personal characteristics, pesticide exposure factors, and health symptoms were analyzed using multiple logistic regression.
-
Results:
- Of the 141 chili farmers studied, 66.7% experienced pesticide poisoning, as indicated by below-normal cholinesterase levels. Fatigue was the most frequently reported symptom associated with pesticide exposure, affecting 37.6% of participants. This was followed by nausea and vomiting (31.9%), dizziness (14.9%), and dry throat (14.9%). Multivariate logistic regression analysis revealed that several factors were significantly associated with adverse symptoms: amount of work experience, volume of pesticides used, use of chemical pesticides, use of leaking containers during spraying, direct pesticide exposure while working, contact with pesticide-soaked clothing, consumption of food and drinks in the fields, and blood cholinesterase level indicating risk.
-
Conclusions:
- This study suggests potential health risks for chili farmers stemming from exposure to and contamination by pesticides used in agricultural practices. To mitigate these risks, it is essential to supply personal protective equipment and to implement educational programs aimed at improving protective behaviors among farmers.
- Agriculture is a vital sector in Thailand, providing much of the population with both food and a livelihood. Rice, along with chilies and maize, plays a key role in the Thai economy and labor force. Pesticides are commonly used in Thailand’s agricultural regions to enhance crop yields and food production. Farmers employ these substances to control crop diseases and pests. Thailand’s annual pesticide imports have been on the rise [1]. The increase in pesticide usage can be attributed to several factors, including insect resistance and pest resurgence, the industrialization of agricultural practices, and the need to switch crop types from season to season in response to market demands, despite varying weather conditions [2]. In 2019, the majority of agricultural chemicals imported into Thailand were insecticides [3]. The most popular families of pesticides are organophosphates (OPs) and carbamates (CAs) [4-6]. Pesticides are most heavily utilized within the subsector of smallholder agricultural production systems.
- Farm workers constitute a high-risk group for agrichemical poisoning exposure [7,8]. Serious health effects are facilitated by the unregulated environment, inadequate use of personal protective equipment, and limited awareness regarding pesticide application [9]. Moreover, the excessive and unsafe use of pesticides poses a major threat to human health, environmental integrity, and food quality [10]. Pesticide applicators, in particular, have grown increasingly concerned about the potential acute and long-term health consequences associated with intensive pesticide use [4,11]. The most pressing issue facing farm workers is exposure to pesticides. The majority of agricultural activities, including pesticide mixing, spraying, harvesting, and cultivation, are conducted manually, which subjects farm workers to dangerous agricultural chemicals [12].
- Most farmers are exposed to pesticides that are absorbed through the skin and inhaled, leading to health issues [13]. This exposure is often due to improper chemical handling and a heavy reliance on pesticides like OPs and CAs to enhance agricultural yields. Such practices can have both immediate and long-term health consequences, including the impact on blood cholinesterase levels from pesticides absorbed through the skin or through breathing [14]. In the present research, pesticide use among chili farmers was monitored by screening blood cholinesterase levels, specifically using the standard method for erythrocyte acetylcholinesterase (AChE). This screening approach is a novel and localized method that has not been previously examined. Moreover, few studies have analyzed the laboratory confirmation of unusual blood cholinesterase levels in Thailand. Consequently, this study aimed to examine the prevalence of health symptoms and their relationship with factors of pesticide exposure and occupational blood cholinesterase levels among chili farmers in Sakon Nakhon Province, Thailand.
INTRODUCTION
- Study Design and Participants
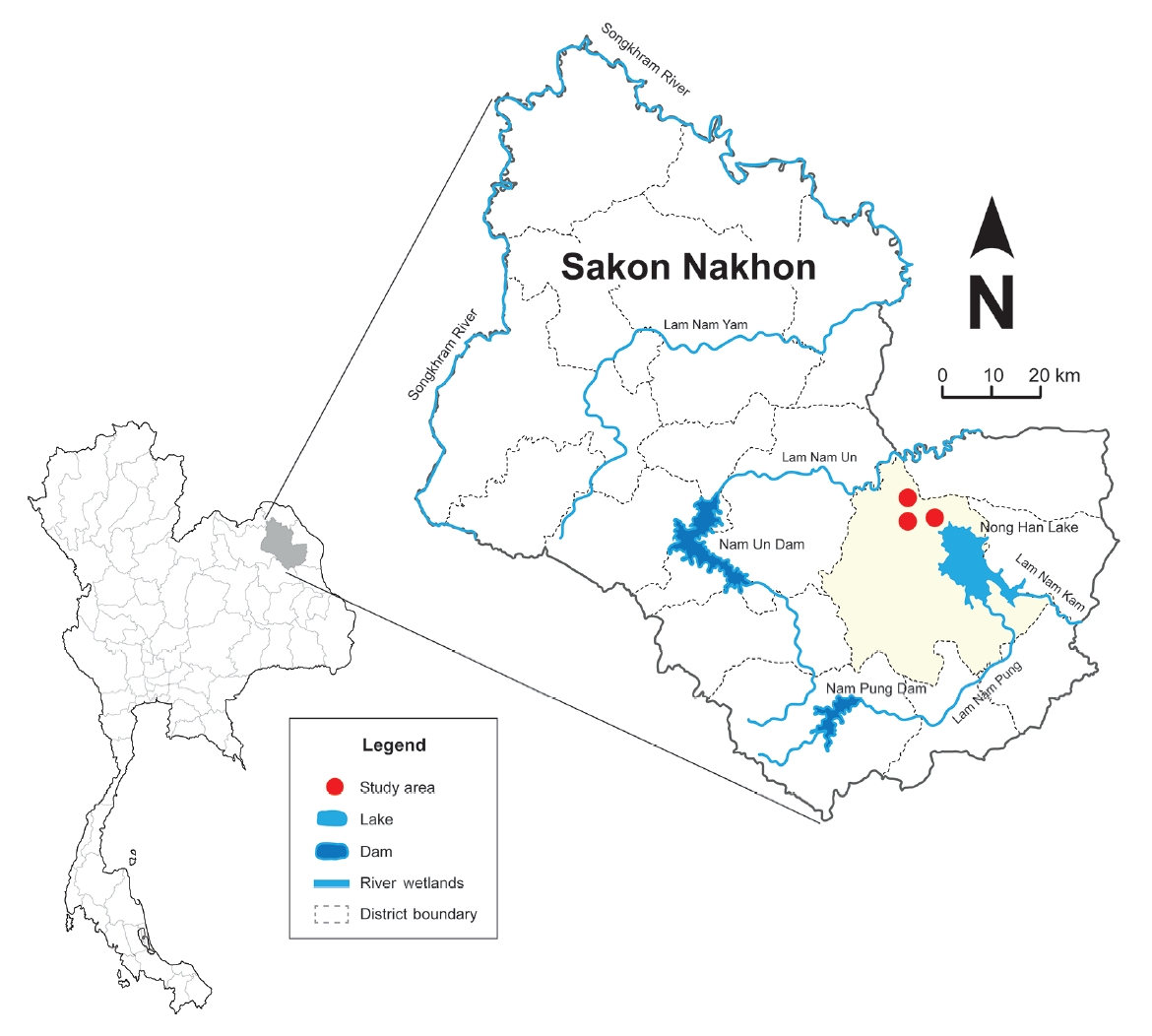
- A cross-sectional analytical study was conducted from September 2021 to March 2022 in northeast Thailand. Three rural communities in Sakon Nakhon Province were selected as the study area because the main occupation in that region is chili farming (Figure 1). Using a purposive sampling method, 47 households from each of the 3 villages were randomly chosen. If a household was unoccupied at the time of the visit, the next nearest household was selected. Within each household, 1 chili farmer was chosen based on convenience. Eligible chili farmers were those over 30 years of age, registered as chili farmers for more than a year, literate, and willing to participate in the study. Health volunteers received training to conduct face-to-face interviews with a structured questionnaire. The sample size was calculated using the formula for the proportion of the population in cases where the entire population is known [15], with a 95% confidence interval (CI). This calculation was informed by the finding that 27.8% of chili farmers reported health symptoms associated with pesticide exposure [15], and the desired precision of the estimate was set at 8%. To account for potential loss or incomplete data, we increased the sample size by at least 20%. In total, 141 chili farmers were included in the study.
- Questionnaire
- Data were gathered through the use of questionnaires and the Health Risk Assessment Form for Pesticide Exposure (NGP 1-56), developed by the Division of Occupational and Environmental Diseases, Department of Disease Control, Ministry of Public Health, Thailand [14]. These instruments were administered during interviews that utilized self-reports to assess health-related issues. The questionnaire was divided into 5 sections. The first section collected demographic information, including sex, age, marital status, congenital diseases, use of pain relievers or muscle relaxants after a long workday, experience in chili cultivation, smoking habits, alcohol consumption, practices of combining chemicals, the likelihood of remaining in areas where chemicals had been sprayed, pesticide application practices, use of chemical pesticides, and chemical usage. The second section focused on the types of work and pesticides employed. The third section addressed the knowledge of pesticide use and the self-protective measures chili farmers take when using pesticides. The fourth section explored behaviors related to pesticide use and prevention strategies, while the fifth section inquired about health symptoms or conditions that arose following pesticide use or exposure.
- The health symptoms reported following pesticide use or exposure within the past month were categorized into 5 groups: (1) nervous system symptoms, which encompass nausea, vomiting, dizziness, headaches, excessive sweating, watery eyes, palpitations, twitching eyelids, insomnia, red eyes, burning eyes, itchy eyes, numbness, drooling, blurred vision, chest pain, chest tightness, trembling hands, an unsteady walk, seizures, blackouts, and loss of consciousness; (2) muscular system symptoms, such as fatigue, muscle weakness, and cramps; (3) respiratory system symptoms, including a dry throat, a burning sensation in the nose, sore throat, cough, difficulty breathing, and nasal discharge; (4) integumentary system symptoms, which cover skin itching, dry or chapped skin, rashes, blisters, and a sensation of burning pain; and (5) gastrointestinal system symptoms, namely stomach pain and diarrhea. Participants who reported experiencing at least one symptom from any of these categories were considered to have symptoms associated with that system. The reliability of the health symptoms questionnaire was tested with a pilot study involving 50 chili farmers from different regions. The results demonstrated reliability, as indicated by a Cronbach alpha coefficient of 0.75.
- Measurement of Erythrocyte Acetylcholinesterase
- A medical technologist performed blood collection to assess cholinesterase levels. The blood was drawn from the antecubital vein in a volume of 3 mL, with the collection process taking 5 minutes per individual, and the samples were kept at a temperature between 2°C and 8°C. To determine erythrocyte cholinesterase levels, we utilized either whole blood or washed erythrocytes. The washed erythrocytes were prepared by removing the plasma and washing the cells three times with an equal volume of saline solution. For the assay of erythrocyte cholinesterase activity, we combined 10 μL of whole blood with 820 μL of a working buffer that included quinidine. Subsequently, 10 μL of a 69 mmol/L acetylcholine solution (yielding a final concentration of 2.0 mmol/L) was added to initiate the reaction. The introduction of 10 μL of a 275 mmol/L acetylcholine solution into the buffer resulted in a blank drift of 4×104 pH/min, whereas the addition of 10 μL of the 69 mmol/L solution produced a drift of 1×104 pH/min [16]. The toxicology laboratory employed a standard method for measuring erythrocyte AChE activity. The reference range was set at 70% of an individual’s sensitivity/detection baseline (per the American Conference of Governmental Industrial Hygienists 2019 guidelines) [17], with the normal range being 1.0 to 1.5. The analysis was carried out by a medical technologist in the toxicology laboratory of the Faculty of Medicine at Ramathibodi Hospital, Bangkok. Blood cholinesterase levels were categorized into two groups: at risk (levels below 1.30 U/g) and normal (levels at or above 1.30 U/g). This classification was based on the cut-off value for the enzyme, which is below the limit of detection value used for biomonitoring AChE among farmers in Bandung, Indonesia [18].
- Statistical Analysis
- The association between personal characteristics, pesticide exposure factors, and health symptoms in chili farmers was examined using multiple logistic regression. In our analyses, the dependent variable was the presence of health effects, coded as 0 for ‘no’ if participants did not report any acute symptoms related to pesticide exposure, and as 1 for ‘yes’ if they reported one or more symptoms [12,15]. The potential confounding factors in the model, namely age and sex, were adjusted based on the recommended factor effect for health symptoms [12,15]. Adjusted odds ratios (aORs) and 95% CIs were reported to describe the strength of the association between the determinants and health symptoms.
- A p-value of less than 0.05 was considered to indicate statistical significance. Analyses were performed using SPSS version 26 (IBM Corp., Armonk, NY, USA).
- Ethics Statement
- Ethical approval for this research was granted by Kasetsart University, Sakon Nakhon, and the accredited human ethics committee approved the research study protocol (Kucsc.HE-64-022). Written informed consent was obtained from all study participants, who voluntarily agreed to take part in the research.
METHODS
Demographic information
Health symptoms
- Demographic Information
- Of the 141 chili farmers surveyed, 62.4% were female, and the mean±standard deviation was 51.43±9.49 years. Among the participants, 24.1% had comorbidities. A majority did not smoke (73.8%), abstained from alcohol (80.1%), and did not use muscle relaxants after a long day of work (68.1%). Most of the farmers had over five years of experience in chili cultivation (80.9%) and were accustomed to using pesticides (83.7%). Of these, 62.4% mixed chemicals themselves, 92.9% remained in the vicinity where chemicals were sprayed, 46.8% personally applied pesticides, and 65.2% used less than 100 L of chemicals per application. The mean activity level of AChE was 1.25±0.08 U/g, with participants divided into 2 categories: 66.7% were considered at risk (with levels below 1.30 U/g), while 33.3% fell within the normal range with levels of 1.30 U/g or higher) (Table 1).
- Health Symptoms Among Chili Farmers
- Table 2 reveals that 119 farmers (84.4% of participants) reported experiencing at least 1 symptom of acute pesticide poisoning following the use or handling of pesticides. In contrast, 15.6% of the respondents did not attribute any health issues they experienced to pesticide exposure. The most frequently reported symptoms associated with pesticide exposure were fatigue (37.6%), nausea and vomiting (31.9%), dizziness (14.9%), and dry throat (14.9%), in that order. Additional symptoms identified by respondents included headaches, nasal irritation, itchy skin, sore throat, excessive sweating, dry or chapped skin, watery eyes, heart palpitations, eyelid twitches, cough, skin rashes with itching, blisters, stomachache, and diarrhea.
- Relationships Between Pesticide Exposure Factors and Pesticide-related Symptoms Among Chili Farmers
- Multiple logistic regression models suggest an association between factors related to pesticide exposure and the occurrence of health symptoms in chili farmers. When the models were adjusted for age and sex, a strong positive association was observed between pesticide exposure and health symptoms. The likelihood of developing health symptoms was higher in association with the chili farmers’ work experience (aOR, 4.54; 95% CI, 1.43 to 14.38; p<0.01), the volume of pesticides used (aOR, 4.15; 95% CI, 1.15 to 14.93; p <0.05), the use of chemical pesticides (aOR, 15.14; 95% CI, 3.09 to 74.21; p<0.001), spraying using a leaking chemical container (aOR, 8.98; 95% CI, 1.95 to 41.44; p<0.01), pesticide exposure during work (aOR, 3.50; 95% CI, 1.23 to 9.94; p<0.05), wearing clothes soaked with pesticides (aOR, 2.93; 95% CI, 1.06 to 8.11; p<0.05), consuming food and drinks in the workplace (aOR, 4.16; 95% CI, 1.12 to 15.35; p<0.05), and blood cholinesterase levels (aOR, 3.36; 95% CI, 1.28 to 8.82; p<0.05). However, the analysis revealed no significant associations between the pesticide-related health symptoms and variables such as sex, age, the area of chili production, and the number of days worked per month (Table 3).
- Relationships Between Health Effects and Blood Cholinesterase Levels in Chili Farmers
- Table 4 presents the multiple logistic regression models that demonstrate a link between health outcomes, occupational characteristics, and blood cholinesterase levels among chili farmers. When the model was adjusted for age and sex, a positive association was observed between blood cholinesterase level and certain adverse health effects, namely those of the nervous (aOR, 2.22; 95% CI, 1.06 to 4.64; p <0.05), muscular (aOR, 3.45; 95% CI, 1.48 to 8.06; p<0.01), and integumentary systems (aOR, 8.80; 95% CI, 1.10 to 70.33; p<0.05). However, no significant correlation was observed for the respiratory and gastrointestinal systems (Table 4).
RESULTS
- This study explored the potential links between pesticide exposure and the occurrence of health symptoms. Our findings indicate that chili farmers are at an increased risk of experiencing health issues associated with pesticide exposure, particularly when considering blood cholinesterase levels. By employing the standard method for measuring erythrocyte AChE activity, we were able to more accurately assess the relationship between pesticide exposure and health symptoms. Consequently, we are confident in our results, which suggest that blood cholinesterase concentrations in chili farmers could influence the manifestation of health symptoms. These findings are consistent with research from Thailand, which reported average activities of AChE and plasma cholinesterase (PChE) at 2.73±0.88 U/mL and 1.58±0.56 U/mL, respectively. Notably, approximately 80% of the chili farmers had detectable OP residues on their hands, and half of the study participants reported experiencing acute health symptoms within 48 hours of pesticide application [15].
- The prevalence of symptoms reported in the survey aligned with previous studies conducted in the Arusha region of Tanzania, where the most common health symptoms were neurological (57.1%), followed by perspiration and headache (40.7%), poor appetite and depression (29.3%), and irritation (26.4%) [19]. Studies from Thailand, Brazil, and Cameroon also indicated that among pesticide-related symptoms, the most frequent included dizziness, coughs, and headaches [20], dyspnea, wheezing, poor digestion, tiredness, and feelings of worthlessness [10], and weakness, itchiness, a burning sensation, sneezing, and vomiting [21]. Furthermore, a study in southern Thailand found that the most frequently self-reported symptoms were coughing (5.7%), tiredness (5.4%), dizziness (5.1%), and dry skin and irritation (4.8%) [22]. Similarly, in western Ethiopia, the prevalence of respiratory symptoms among small-scale farmers exposed to pesticide chemicals was 87.2%, with coughing, headaches, skin irritation, and inhalation and skin contact issues primarily attributed to inadequate knowledge, practices, and education, as well as factors such as age, work, and low income [23]. Applicators were more likely than residents to report skin irritation, shortness of breath, coughing, and dizziness, which may be related to the perceived toxicity of the mixture of pesticides in use [11].
- Multiple logistic regression analysis revealed 8 factors independently associated with persistent health symptoms in chili farmers, even after adjusting for major confounders. These confounders included work experience, the volume of pesticide use, use of chemical pesticides, leakage from chemical containers during spraying, pesticide exposure while working, wearing clothes soaked with pesticides, consuming food and drinks in the workplace, and blood cholinesterase levels. The studies suggest that pesticide exposure in chili farmers is significantly linked to a higher prevalence of health symptoms. These finding echoes research on rice farmers in Indonesia, which identified the frequency of pesticide spraying as the most critical factor in pesticide poisoning incidents. Other risk factors include the mixing dosage, frequency of spraying, working hours, and wind direction [24]. Additionally, research from the Chitwan District in Nepal reported acute symptoms in the prior 12 months among chemical pesticide users [25]. In the previously referenced study from Thailand, exposure to certain pesticides (OP, chlorpyrifos, and profenofos) on the hands was significantly associated with health symptoms in chili farmers [15]. Observations indicated inadequate pesticide handling and application practices, such as leaking spray tanks, smoking while working, and consuming food and alcohol in the work area [20]. The work experience of farmers, along with their level of knowledge and attitudes, may influence the occurrence of acute health symptoms [12]. These findings also suggest a link between blood cholinesterase levels and health symptoms, which is consistent with research from Tanzania that showed a correlation between self-reported fatigue symptoms and lower AChE levels [13]. In the study from southern Thailand, individuals with abnormal serum AChE levels were more likely to report dizziness as a primary symptom [22]. These studies propose that blood cholinesterase levels are related to health effects in chili farmers. Multiple logistic regression analysis also revealed health effects on the nervous, muscular, and integumentary systems associated with blood cholinesterase levels in chili farmers, after accounting for major confounders. This result is supported by the study from the Arusha Region, which found that the most frequently reported neurological symptom was fatigue (57.1%), and 27% of pesticide applicators had AChE levels below the permissible limit [19]. AChE is a cholinergic enzyme primarily located at postsynaptic neuromuscular junctions, especially in nerves and muscles. The primary role of AChE is to terminate neuronal transmission and synaptic signaling to prevent AChE dispersal and the activation of nearby receptors. OPs and CAs can impact cholinesterase activity in both the central and peripheral nervous systems, potentially affecting various body systems, including the exocrine glands, eyes, gastrointestinal tract, respiratory tract, cardiovascular system, and skeletal muscles [26]. Symptoms such as confusion, headache, and impaired memory can arise from exposure to these substances, with repeated exposure leading to neurotoxic and neuromuscular effects. The prevalence of organophosphates in this study underscores the importance of monitoring cholinesterase activity as a primary test for pesticide poisoning.
- Several limitations of this study should be considered when interpreting the results. First, the study relied on self-reported data collected during interviews, which may be subject to memory biases. Despite this, the data were gathered using a standardized questionnaire for health risk assessment from pesticide exposure in farmers (NGP 1-56), developed by the Division of Occupational and Environmental Diseases, Department of Disease Control, Ministry of Public Health, Thailand. In future research, blood AChE activity, in conjunction with the questionnaire on risk assessment from pesticide exposure, could be utilized to predict health impairments. Secondly, establishing a causal link between factors related to pesticide exposure and the blood cholinesterase levels of chili farmers, and their health symptoms, is challenging. This is due to the nature of cross-sectional analytic studies, which can only suggest potential associations among the 141 participants involved. Lastly, the study was conducted with a relatively small sample size as it was a preliminary investigation. Nevertheless, the findings demonstrate a significant association between factors related to pesticide exposure and health symptoms in rural community settings. Consequently, additional studies are required.
- In conclusion, our findings revealed that various factors related to pesticide exposure and blood AChE levels are associated with a higher prevalence of health symptoms among chili farmers. These results indicate a need for targeted public health education and training programs for chili farmers, particularly emphasizing the importance of using appropriate personal protective equipment to minimize chemical exposure and enhance their proficiency in pesticide application. Furthermore, it is essential to conduct regular monitoring of blood cholinesterase levels and implement effective strategies to decrease pesticide exposure in order to safeguard the health of chili farmers.
DISCUSSION
-
Conflict of Interest
The authors have no conflicts of interest associated with the material presented in this paper.
-
Funding
The study received support from the Graduate Research Fellowships at Kasetsart University, Thailand.
-
Author Contributions
Conceptualization: Kammoolkon R, Pengpan R. Data curation: Pengpan R, Kopolrat KY, Kammoolkon R. Formal analysis: Kopolrat KY, Pengpan R. Funding acquisition: Kammoolkon R, Pengpan R. Methodology: Kammoolkon R, Kopolrat KY, Srichaijaroonpong S, Taneepanichskul N. Visualization: Yasaka P, Kopolrat KY. Writing – original draft: Pengpan R, Kammoolkon R, Kopolrat KY. Writing – review & editing: Kammoolkon R, Kopolrat KY, Pengpan R, Srichaijaroonpong S, Taneepanichskul N, Yasaka P.
Notes
Acknowledgements
| Factors | No. of examined |
Health symptoms, n (%) |
cOR (95% CI) | aOR (95% CI) | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Sex1 | |||||
| Female | 88 | 74 (84.1) | 14 (15.9) | 1.08 (0.43, 2.70) | 1.03 (0.40, 2.63) |
| Male | 53 | 44 (83.0) | 9 (17.0) | 1.00 (reference) | 1.00 (reference) |
| Age (y)2 | |||||
| ≤40 | 17 | 16 (94.1) | 1 (5.9) | 5.33 (058, 49.18) | 6.45 (0.67, 62.42) |
| 41-50 | 48 | 42 (87.5) | 6 (12.5) | 2.33 (066, 8.22) | 2.31 (0.64, 8.32) |
| 51-60 | 52 | 42 (80.8) | 10 (19.2) | 1.40 (0.44, 4.43) | 1.45 (0.45, 4.63) |
| >60 | 24 | 18 (75.0) | 6 (25.0) | 1.00 (reference) | 1.00 (reference) |
| Work experience (y)3 | |||||
| >5 | 114 | 99 (86.8) | 15 (13.2) | 2.78 (1.03, 7.47)* | 4.54 (1.43, 14.38)** |
| ≤5 | 27 | 19 (70.4) | 8 (29.6) | 1.00 (reference) | 1.00 (reference) |
| Chili production area (ha)3 | |||||
| >1 | 46 | 40 (87.0) | 6 (13.0) | 1.45 (0.53, 3.97) | 1.41 (0.51, 3.91) |
| ≤1 | 95 | 78 (82.1) | 17 (17.9) | 1.00 (reference) | 1.00 (reference) |
| No. days per month work3 | |||||
| >7 | 12 | 11 (91.7) | 1 (8.3) | 2.26 (0.28, 18.43) | 2.12 (0.26, 17.50) |
| ≤7 | 129 | 107 (82.9) | 22 (17.1) | 1.00 (reference) | 1.00 (reference) |
| Volume of pesticides usage (L)3 | |||||
| >100 | 49 | 46 (93.9) | 3 (6.1) | 4.26 (1.20, 15.15)* | 4.15 (1.15, 14.93)* |
| ≤100 | 92 | 72 (78.3) | 20 (21.7) | 1.00 (reference) | 1.00 (reference) |
| Chemical pesticide usage3 | |||||
| Yes | 132 | 115 (87.1) | 17 (12.9) | 13.53 (3.09, 59.23)*** | 15.14 (3.09, 74.21)*** |
| No | 9 | 3 (33.3) | 6 (66.7) | 1.00 (reference) | 1.00 (reference) |
| While spraying, use a leaking chemical container3 | |||||
| Yes | 55 | 53 (96.4) | 2 (3.6) | 8.56 (1.92, 38.18)** | 8.98 (1.95, 41.44)** |
| No | 86 | 65 (75.6) | 21 (24.4) | 1.00 (reference) | 1.00 (reference) |
| Pesticide exposure while working3 | |||||
| Yes | 117 | 102 (87.2) | 15 (12.8) | 3.40 (1.24, 9.31)* | 3.50 (1.23, 9.94)* |
| No | 24 | 16 (66.7) | 8 (33.3) | 1.00 (reference) | 1.00 (reference) |
| Clothes soaked with pesticides3 | |||||
| Yes | 113 | 99 (87.6) | 14 (12.4) | 3.35 (1.27, 8.84)* | 2.93 (1.06, 8.11)* |
| No | 28 | 19 (67.9) | 9 (32.1) | 1.00 (reference) | 1.00 (reference) |
| Consume food and drinks in the workplace3 | |||||
| Yes | 47 | 44 (93.6) | 3 (6.4) | 3.96 (1.11, 14.11)* | 4.16 (1.12, 15.35)* |
| No | 94 | 74 (78.7) | 20 (21.3) | 1.00 (reference) | 1.00 (reference) |
| Blood cholinesterase level3 | |||||
| Risk level (<1.30 U/g) | 95 | 84 (88.4) | 11 (11.6) | 2.69 (1.09, 6.70)* | 3.36 (1.28, 8.82)* |
| Normal level (≥1.30 U/g) | 46 | 34 (73.9) | 12 (26.1) | 1.00 (reference) | 1.00 (reference) |
| Health effects | No. of examined |
Blood cholinesterase level, n (%) |
cOR (95% CI) | aOR (95% CI)1 | |
|---|---|---|---|---|---|
| Risk level (<1.30 U/g) | Normal level (≥1.30 U/g) | ||||
| Nervous system | |||||
| Yes | 75 | 56 (74.7) | 19 (25.3) | 2.04 (0.99, 4.17) | 2.22 (1.06, 4.64)* |
| No | 66 | 39 (59.1) | 27 (40.9) | 1.00 (reference) | 1.00 (reference) |
| Muscular system | |||||
| Yes | 53 | 43 (81.1) | 10 (18.9) | 2.98 (1.33, 6.68)** | 3.45 (1.48, 8.06)** |
| No | 88 | 52 (59.1) | 36 (40.9) | 1.00 (reference) | 1.00 (reference) |
| Respiratory system | |||||
| Yes | 49 | 38 (77.6) | 11 (22.4) | 2.12 (0.96, 4.68) | 2.24 (1.00, 5.04) |
| No | 92 | 57 (62.0) | 35 (38.0) | 1.00 (reference) | 1.00 (reference) |
| Integumentary system | |||||
| Yes | 16 | 15 (93.7) | 1 (6.3) | 8.44 (1.08, 66.00)* | 8.80 (1.10, 70.33)* |
| No | 125 | 80 (64.0) | 45 (36.0) | 1.00 (reference) | 1.00 (reference) |
| Gastrointestinal system | |||||
| Yes | 2 | 1 (50.0) | 1 (50.0) | 0.48 (0.03, 7.83) | 1.91 (0.11, 31.84) |
| No | 139 | 94 (67.6) | 45 (32.4) | 1.00 (reference) | 1.00 (reference) |
- 1. Laohaudomchok W, Nankongnab N, Siriruttanapruk S, Klaimala P, Lianchamroon W, Ousap P, et al. Pesticide use in Thailand: current situation, health risks, and gaps in research and policy. Hum Ecol Risk Assess 2021;27(5):1147-1169. https://doi.org/10.1080/10807039.2020.1808777ArticlePubMed
- 2. Panuwet P, Siriwong W, Prapamontol T, Ryan PB, Fiedler N, Robson MG, et al. Agricultural pesticide management in Thailand: situation and population health risk. Environ Sci Policy 2012;17: 72-81. https://doi.org/10.1016/j.envsci.2011.12.005ArticlePubMedPMC
- 3. Wattanathada S. In situation and information on the use of chemicals pesticides of Thailand. Talat Khwan: Department of Disease Control; 2019. (Thai)
- 4. Ntow WJ, Gijzen HJ, Kelderman P, Drechsel P. Farmer perceptions and pesticide use practices in vegetable production in Ghana. Pest Manag Sci 2006;62(4):356-365. https://doi.org/10.1002/ps.1178ArticlePubMed
- 5. Ngowi AV, Mbise TJ, Ijani AS, London L, Ajayi OC. Pesticides use by smallholder farmers in vegetable production in Northern Tanzania. Crop Prot 2007;26(11):1617-1624. https://doi.org/10.1016/j.cropro.2007.01.008ArticlePubMedPMC
- 6. Vikkey HA, Fidel D, Elisabeth YP, Hilaire H, Hervé L, Badirou A, et al. Risk factors of pesticide poisoning and pesticide users’ cholinesterase levels in cotton production areas: Glazoué and Savè townships, in central Republic of Benin. Environ Health Insights 2017;11: 1178630217704659. https://doi.org/10.1177/1178630217704659ArticlePubMedPMC
- 7. McConnell R, Cedillo L, Keifer M, Palomo MR. Monitoring organophosphate insecticide-exposed workers for cholinesterase depression. New technology for office or field use. J Occup Med 1992;34(1):34-37PubMed
- 8. Watterson A. Pesticide health and safety and the work and impact of international agencies: partial successes and major failures. Int J Occup Environ Health 2001;7(4):339-347. https://doi.org/10.1179/107735201800339245ArticlePubMed
- 9. Mattah MM, Mattah PA, Futagbi G. Pesticide application among farmers in the catchment of Ashaiman irrigation scheme of Ghana: health implications. J Environ Public Health 2015;2015: 547272. https://doi.org/10.1155/2015/547272ArticlePubMedPMC
- 10. Buralli RJ, Ribeiro H, Iglesias V, Muñoz-Quezada MT, Leão RS, Marques RC, et al. Occupational exposure to pesticides and health symptoms among family farmers in Brazil. Rev Saude Publica 2020;54: 133. https://doi.org/10.11606/s1518-8787.2020054002263ArticlePubMedPMC
- 11. Tessema RA, Nagy K, Ádám B. Occupational and environmental pesticide exposure and associated health risks among pesticide applicators and non-applicator residents in rural Ethiopia. Front Public Health 2022;10: 1017189. https://doi.org/10.3389/fpubh.2022.1017189ArticlePubMedPMC
- 12. Kangkhetkron T, Juntarawijit C. Factors influencing practice of pesticide use and acute health symptoms among farmers in Nakhon Sawan, Thailand. Int J Environ Res Public Health 2021;18(16):8803. https://doi.org/10.3390/ijerph18168803ArticlePubMedPMC
- 13. Kapeleka JA, Sauli E, Sadik O, Ndakidemi PA. Biomonitoring of acetylcholinesterase (AChE) activity among smallholder horticultural farmers occupationally exposed to mixtures of pesticides in Tanzania. J Environ Public Health 2019;2019: 3084501. https://doi.org/10.1155/2019/3084501ArticlePubMedPMC
- 14. Department of Disease Control, Ministry of Public Health. Division of occupational and environmental diseases [cited 2022 May 7]. Available from: https://ddc.moph.go.th/doed/newspic.php (Thai)
- 15. Nganchamung T, Robson MG, Siriwong W. Association between blood cholinesterase activity, organophosphate pesticide residues on hands, and health effects among chili farmers in Ubon Ratchathani Province, northeastern Thailand. Rocz Panstw Zakl Hig 2017;68(2):175-183PubMed
- 16. Barenghi L, Ceriotti F, Luzzana M, Ripamonti M, Mosca A, Bonini PA. Measurement of erythrocyte acetylcholinesterase and plasma cholinesterase activity by a differential pH technique. Ann Clin Biochem 1986;23(Pt 5):538-545. https://doi.org/10.1177/000456328602300509ArticlePubMed
- 17. American Conference of Governmental Industrial Hygienists (ACGIH). TLV/BEI guidelines; 2019 [cited 2024 Jan 26]. Available from: https://www.acgih.org/science/tlv-bei-guidelines/
- 18. Mulyana M, Sugiarta I, Fuk LJ, Pratami VN, Fitriani DY, Adi NP, et al. Biomonitoring of acetylcholinesterase (AChE) inhibitor and the association with hypertension among farmers in Bandung, Indonesia. Indones Biomed J 2020;12(4):325-332. https://doi.org/ 10.18585/inabj.v12i4.1220Article
- 19. Mwabulambo SG, Mrema EJ, Ngowi AV, Mamuya S. Health symptoms associated with pesticides exposure among flower and onion pesticide applicators in Arusha region. Ann Glob Health 2018;84(3):369-379. https://doi.org/10.29024/aogh.2303ArticlePubMedPMC
- 20. Laor P, Keawdounglek V, Hongtong A, Suma Y, Pasukphun N, Songla T, et al. Health risk and health status of farmers exposed to chemical pesticides used in agriculture. J Curr Sci Technol 2019;9(2):89-98. https://doi.org/10.14456/jcst.2019.9Article
- 21. Manfo FP, Suh CF, Nantia EA, Moundipa PF, Cho-Ngwa F. Occupational use of agrochemicals results in inhibited cholinesterase activity and altered reproductive hormone levels in male farmers from Buea, Cameroon. Toxicol Res (Camb) 2021;10(2):232-248. https://doi.org/10.1093/toxres/tfaa113ArticlePubMedPMC
- 22. Guytingco A, Thepaksorn P, Neitzel RL. Prevalence of abnormal serum cholinesterase and associated symptoms from pesticide exposure among agricultural workers in the south of Thailand. J Agromedicine 2018;23(3):270-278. https://doi.org/10.1080/1059924X.2018.1470049ArticlePubMed
- 23. Afata TN, Mekonen S, Shekelifa M, Tucho GT. Prevalence of pesticide use and occupational exposure among small-scale farmers in western Ethiopia. Environ Health Insights 2022;16: 11786302211072950. https://doi.org/10.1177/11786302211072950ArticlePubMedPMC
- 24. Sodikin A, Muhyi R, Suhartono E, Marlinae L. Analysis of factors related to pesticide poisoning in rice farmers in Teweh Selatan Subdistrict, Barito Utara District. Indian J Forensic Med Toxicol 2020;14(3):1763-1768. https://doi.org/10.37506/ijfmt.v14i3.10671Article
- 25. Kafle S, Vaidya A, Pradhan B, Jørs E, Onta S. Factors associated with practice of chemical pesticide use and acute poisoning experienced by farmers in Chitwan District, Nepal. Int J Environ Res Public Health 2021;18(8):4194. https://doi.org/10.3390/ijerph18084194ArticlePubMedPMC
- 26. Sapbamrer R, Nata S. Health symptoms related to pesticide exposure and agricultural tasks among rice farmers from Northern Thailand. Environ Health Prev Med 2014;19(1):12-20. https://doi.org/10.1007/s12199-013-0349-3ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Emerging diseases: trend research and omics-based analysis reveals mechanisms of endophytes modulate Chilli plant resilience
Wiwiek Harsonowati, Evy Latifah, Arinal Haq Izzawati Nurrahma, Jati Purwani, Rashid Iqbal, Javid Ahmad Parray, Ashish D. Patel
Symbiosis.2024;[Epub] CrossRef - An Analysis of Occupational Hazards Based on the Physical Ergonomics Dimension to Improve the Occupational Health of Agricultural Workers: The Case in Mayo Valley, Mexico
Víctor Manuel Ramos-García, Josué Aarón López-Leyva, Ana Paola Balderrama-Carmona, Iván Ochoa-Vázquez, Juan José García-Ochoa, Manuel de Jesús Espinoza-Espino
Safety.2024; 10(3): 61. CrossRef
 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite


