Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 45(3); 2012 > Article
-
Special Article
Korean National Health Insurance Value Incentive Program: Achievements and Future Directions - Sun Min Kim, Won Mo Jang, Hyun Ah Ahn, Hyang Jeong Park, Hye Sook Ahn
-
Journal of Preventive Medicine and Public Health 2012;45(3):148-155.
DOI: https://doi.org/10.3961/jpmph.2012.45.3.148
Published online: May 31, 2012
Health Insurance Review and Assessment Service, Seoul, Korea.
- Corresponding author: Won Mo Jang, MD, PhD. 267 Hyoryeong-ro, Seocho-gu, Seoul 137-706, Korea. Tel: +82-2-2182-2637, Fax: +82-2-6710-5818, thomasjang2@gmail.com
Copyright © 2012 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- Since the reformation of the National Health Insurance Act in 2000, the Health Insurance Review and Assessment Service (HIRA) in the Republic of Korea has performed quality assessments for healthcare providers. The HIRA Value Incentive Program (VIP), established in July 2007, provides incentives for excellent-quality institutions and disincentives for poor-quality ones. The program is implemented based on data collected between July 2007 and December 2009. The goal of the VIP is to improve the overall quality of care and decrease the quality gaps among healthcare institutions. Thus far, the VIP has targeted acute myocardial infarction (AMI) and Caesarian section (C-section) care. The incentives and disincentives awarded to the hospitals by their composite quality scores of the AMI and C-section scores. The results of the VIP showed continuous and marked improvement in the composite quality scores of the AMI and C-section measures between 2007 and 2010. With the demonstrated success of the VIP project, the Ministry of Health and Welfare expanded the program in 2011 to include general hospitals. The HIRA VIP was deemed applicable to the Korean healthcare system, but before it can be expanded further, the program must overcome several major concerns, as follows: inclusion of resource use measures, rigorous evaluation of impact, application of the VIP to the changing payment system, and expansion of the VIP to primary care clinics.
- Since the reformation of the National Health Insurance Act in 2000, the Health Insurance Review and Assessment Service (HIRA) in the Republic of Korea has performed quality assessments for healthcare providers. Under the single unified National Health Insurance system, the HIRA quality assessments have progressed rapidly due to advanced technologies in information collection and communication.
- Information regarding the performance of individual institutions is made accessible to the public and each provider. The HIRA quality assessments include a number of measures to help all nationwide healthcare institutions improve the quality of care and lower costs. HIRA includes 16 items (2011) as follows: acute myocardial infarction, acute stroke, use of prophylactic antibiotics for surgery (11 surgeries), Caesarian section, surgical volume indicator, coronary artery bypass graft, prescription (6 sub-measures), hypertension, diabetes mellitus, long-term care hospitals, mental hospital within medical aid, hemodialysis, otitis media in children, colorectal cancer, gastric cancer, and breast cancer.
- More than 36% of all National Health Insurance medical expenses are evaluated by HIRA quality assessment. The Reformed National Health Insurance Act of 2000 authorized a financial incentive structure that could adjust the payment by increasing or reducing the cost of the medical care benefit in accordance with performance. Previously, the government postponed the financial incentive because providers, administrators, and patients were not experienced in the HIRA quality assessment. However, the need to implement financial incentives for performance emerged after the mid-2000s, and the Board of Audit and Inspection and the National Assembly recommended the implementation of pay for performance. The Ministry of Health and Welfare (MOHW) allowed financial incentives for performance to be adopted and allowed HIRA to implement the Value Incentive Program (VIP). Currently, VIPs are under expansion for primary clinics, hospitals, and nursing facilities. This article documents the experience of the VIP for acute-phase hospitals.
INTRODUCTION
- I. History
- The VIP, established in July 2007, provides incentives for excellent-quality institutions and disincentives for poor-quality ones [1,2]. The program was implemented based on data collected between July 2007 and December 2009. During this period, tertiary hospitals were evaluated for their rates of acute myocardial infarction (AMI) and Caesarean section (C-section). The results were announced based on these data, and the incentives were provided in the following year. Hence, a 1-year time lag exists between each period reflecting the clinical treatment performed and the reporting of the results.
- The expanded VIP was launched in 2010. Data collection started in January 2010 and will continue until December 2012. Target institutions have been expanded to general hospitals, and target groups of incentives (and disincentives) have also been extended. The first results of the expanded VIP were announced in November 2011 and incentives were provided in December 2011.
- II. Goal
- The goal of the VIP is to improve the overall quality of care and decrease the quality gaps among healthcare institutions. Thus far, the VIP has targeted AMI and C-section care. The 30-day case fatality of AMI in Korea (6.3%) is the highest among the member countries of the Organization for Economic Cooperation and Development (OECD, average rate across OECD countries was 5.4% in 2009) [3]. The C-section rate in Korea (35.1%) is also among the highest levels of the OECD member countries (average rate across OECD countries was 25.8% in 2008) [3].
- III. Target Hospitals
- Forty-four tertiary hospitals have thus far been mandated to participate in the VIP for the following reasons. First, many of them already have mechanisms of quality assessment and experience with quality improvement. Second, they are expected to practice social accountability in terms of quality. Hospitals that are designated as tertiary hospitals are provided with an additional payment amounting to 30% of the total payment within the National Health Insurance.
- IV. Quality Measures
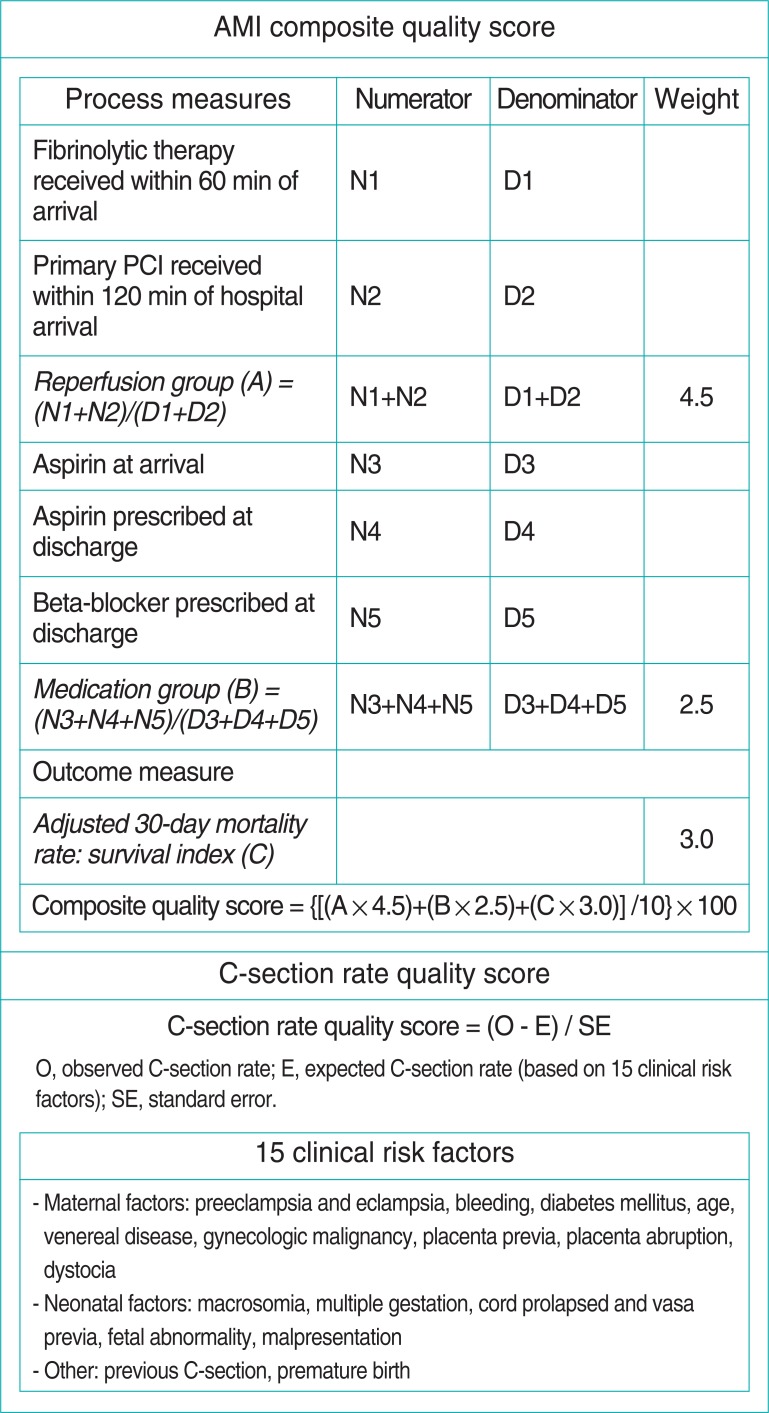
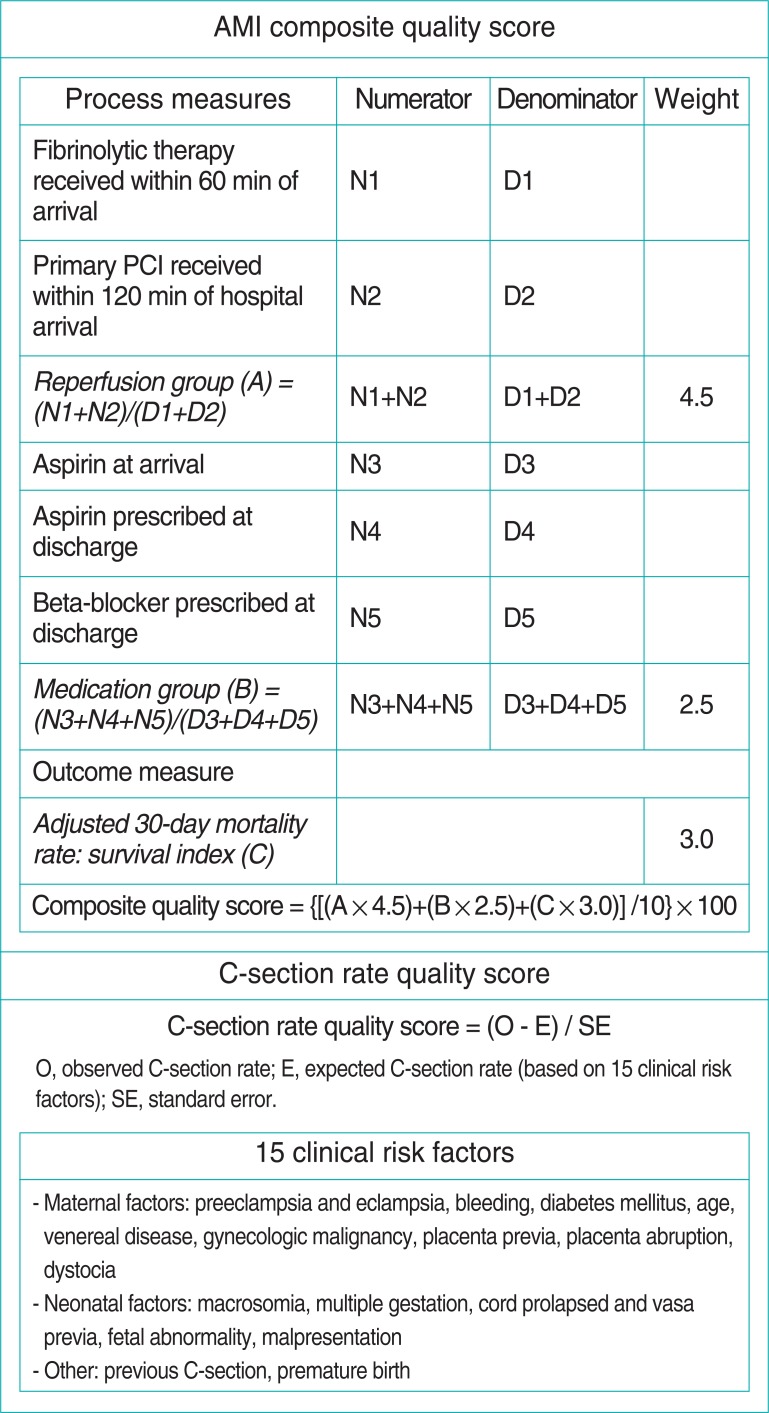
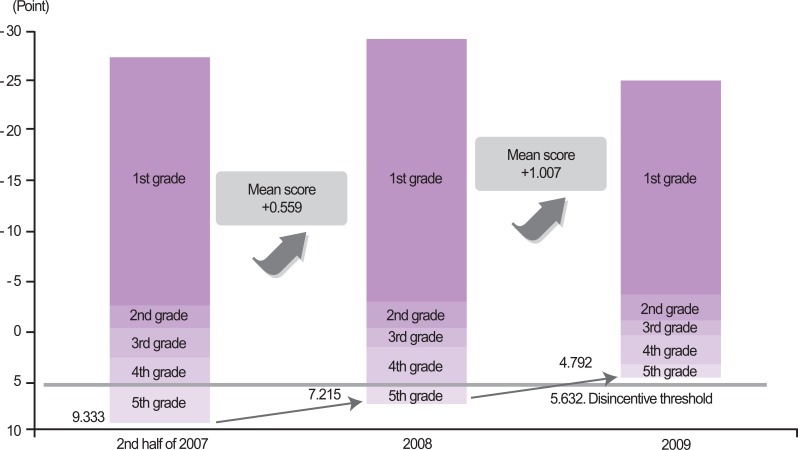
- To evaluate the quality of AMI care, the VIP has assessed six indicators to date: 1) the rate of thrombolytic drug administration within 60 minutes of hospital arrival; 2) the rate of primary percutaneous coronary intervention (PCI) performance within 120 minutes of arrival; 3) the rate of aspirin administration upon arrival (as a percentage of all arrival patients); 4) the rate of aspirin prescription at discharge (as a percentage of all discharge patients); 5) the rate of beta-blocker prescription at discharge (as a percentage of all discharge patients); and 6) the 30-day case fatality after hospitalization [4-10]. After measuring these six indicators, a composite quality score (CQS) is calculated for each hospital (Figure 1 shows the CQSs for VIP and expanded VIP). The rates of thrombolytic drug administration and primary PCI performance were incorporated into the reperfusion indicators, and the rates of aspirin prescription at arrival and discharge and the rate of beta-blocker prescription were merged into the drug prescription rate. To produce the composite score, a relative weight was given to three indicators: 4.5 for reperfusion, 2.5 for drug prescription, and 3.0 for case fatality rate. In 2010, the thresholds of first and second measures of AMI were shortened from 60 minutes and 120 minutes to 30 minutes and 90 minustes.
- The quality of the C-section rate was assessed by the quality score, which is the difference between the observed and expected C-section rates (Figure 1) [11-16]. The expected C-section rate was calculated by a multiple regression equation with 16 risk factors of C-section. Bleeding was excluded, and a total of 15 risk factors were used from 2010 (expanded VIP). Institutions are excluded when their total number of cases comes to less than 30, or when each indicator comprises fewer than 10 cases in AMI CQS.
- The information needed for AMI quality assessment was gathered from the claims data warehouse and a Web-based hospital quality data acquisition system, while the C-section rate was calculated only with the claims data warehouse. Using an independent survey, the validity of the data was investigated. Institutions are excluded when their total number of cases comes to less than 30 in C-section CQS.
- There are four steps from the development to utilization of the measures. The first step leads to developing a plan for the included items, institutions, periods, inclusion/exclusion criteria, and utilization of results. The next step is to formulate a detailed plan for each item, and when medical advice is required, it can be collected by an expert consultative body. The third step is to execute the assessment plan including data collection, analysis, etc. The last step is to disclose the assessment results and pay for performance (e.g., VIP). The central assessment committee, which was established by Article 59 of the National Health Insurance Act, reviews each step of the assessment implementation procedures.
- V. Applying Incentives
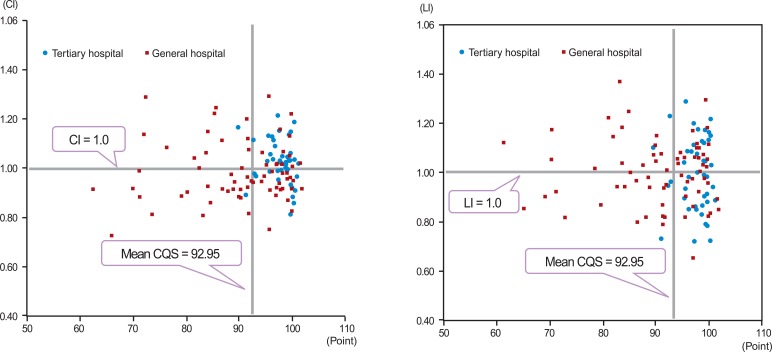
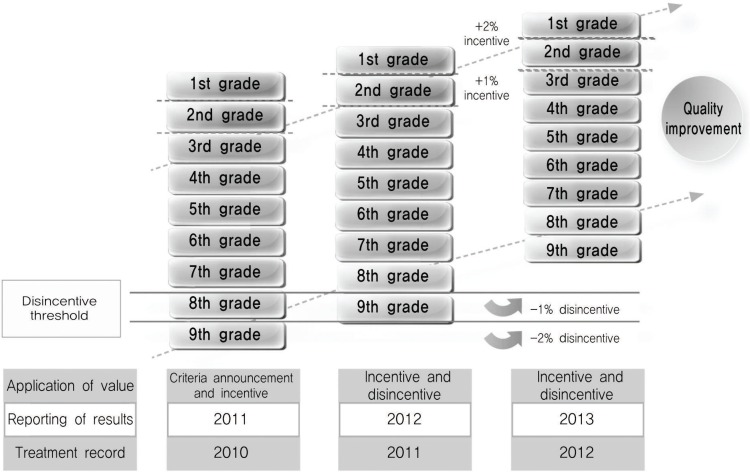
- The VIP was designed after the Premier Hospital Quality Incentive Demonstration Project of the United States Centers for Medicare and Medicaid Services (Figure 2). The hospitals were categorized into five performance grades by the composite quality scores of the AMI and C-section scores. In the first year, the performance grade of each hospital was reported to the public, but the incentive or penalty was not applied. The upper limit of the fifth-ranked group in the first year was announced as the threshold of the penalty 2 years later. If a hospital attained a quality score lower than this threshold 2 years later, the penalty would be applied. The incentive and the penalty were 1% of the cost paid by the National Health Insurance Corporation. In the second year, the 1% incentive was provided to the top performers and those that improved their quality of care. In the third year, the 1% penalty would have been applied to any hospitals that performed lower that the threshold. However, each hospital scored higher than the threshold level so none were penalized. An incentive was given to all hospitals, some for being high performers and others for improving their quality of care.
- VI. Amount of Incentives
- The incentives awarded to the hospitals were Korean won (KRW) 857 million in total between 2008 and 2010. In the second year, KRW 453 million was provided to 21 hospitals, and in the third year KRW 404 million was awarded to 26 hospitals (Table 1). Because the overall quality scores improved, a penalty was not applied to any hospital.
FRAMEWORK OF THE VALUE INCENTIVE PROGRAM
- I. Acute Myocardial Infarction
- The results of the VIP and expanded VIP showed continuous and marked improvement in the CQSs of the AMI measures between 2007 and 2010. There was a 5.60-point increase in the mean CQS and 6.72 decrease in the standard deviation (or variation in performance) among institutions.
- There were clear improvements in the process indicators, including the fibrinolytic administration rate within 60 minutes of hospital arrival and primary PCI rate within 120 minutes of hospital arrival. These results show that the margin for improvement was actually quite low because the hospitals already had high rates of aspirin administration at arrival, aspirin prescription at discharge, and beta-blocker prescription at discharge.
- The CQSs of AMI care indicated improvement in all grades (Figure 3). The mean, minimum, and maximum values were improved and the standard deviation was reduced. In particular, quality improvement was more prominent in the lower grades.
- II. Caesarian Section
- The results of the VIP and expanded VIP showed continuous and marked improvement in standard scores of the C-section rate measured between 2007 and 2010. There was a 1.82-point decrease in the mean standard score and a 0.64-point decrease in the standard deviation among institutions.
- Compared to 2009, the standard scores of the C-section rate in 2010 improved slightly, by 1.11 points. In 2010, general hospitals were included as eligible institutions for the VIP, and in this group, there was greater improvement (2.52 points) in the standard score. The C-section rate standard scores of general hospitals were lower than tertiary hospitals, suggesting that newer participants and lower-performing institutions showed greater improvement.
- The results of the standard score of the C-section rate showed improvement in all grades (Figure 4). The mean, minimum, and maximum values improved and the standard deviation was reduced. In particular, quality improvement was more prominent in the lower grades.
QUALITY CHANGES BY THE VALUE INCENTIVE PROGRAM
- With the demonstrated success of the VIP project, the Ministry of Health and Welfare expanded the program in 2011 to include general hospitals (data of 2010). However, general hospitals were excluded when their total number of delivery cases comes to less than 200 in C-section. Among the hospitals that treated AMI patients in 2010, 98% of tertiary hospitals (43) and 49% of general hospitals (71) were mandated to participate in the Expanded VIP. For the C-section Expanded VIP, all tertiary hospitals (44) and 46% of general hospitals (50) participated (data of 2010).
- Five performance grades were sub-divided into nine grades. The amount of the incentive was also enlarged: 2% of the cost paid by NHIC would be provided to the highest performing group and 1% to the second-highest performing group (Figure 5). There were two thresholds of penalties. For the low performers whose quality scores were less than the upper limit of the lowest group, a 2% penalty would be applied. For those performing below the upper limit of the second-lowest group, a 1% penalty would be applied.
- The expanded VIP also included a broader area of quality assessment. Acute stroke care and prophylactic use of antibiotics for surgical care were selected as the next items for inclusion in the VIP. Although mortality has steadily decreased, stroke is still the leading cause of death, and the geographical gap in the quality of stroke care is significant. Furthermore, acute stroke increases the number of disabled persons, resulting in higher healthcare costs. Whereas HIRA and many providers are experienced in quality assessment and have achieved quality improvement in general, there are non-responding institutions with low performance despite the quality assessment incentive and public report. To address these challenges, the MOHW will include acute stroke care in the VIP in May 2013.
- Excessive drug utilization is one of the challenges of Korea's healthcare system. The irrelevant use of antibiotics leads to resistance to antibiotics and high surgical infection rates. The prophylactic use of antibiotics became a pay-for-performance subject in January 2012, and the target institutions are tertiary hospitals and general hospitals. The details of these issues, including the quality grades, are still under discussion.
EXPANDED VALUE INCENTIVE PROGRAM
- The HIRA VIP was deemed applicable to the Korea healthcare system, but before it can be expanded further, the program must overcome several major concerns, outlined below.
- I. Inclusion of Resource Use Measure
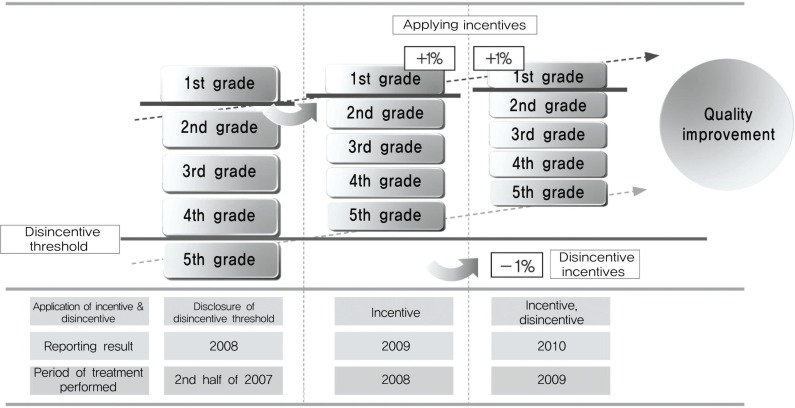
- The results of the HIRA VIP revealed the lack of association between quality and low cost (Figure 6). To move toward meeting higher quality and efficiency, the HIRA prepared methods that adapted and applied resource use measures to the VIP in 2011. HIRA uses the costliness index (CI) and length of stay index (LI) as resource use measures. The CI and LI can be calculated after controlling the case-mix difference of each provider within the Korean diagnosis-related group (KDRG) as follows:
- Utilizing the VIP, tertiary hospitals with a quality of care below that of general hospitals, or which have costs and/or lengths of stay above that of general hospitals, have been targeted for improvement.
- II. Rigorous Evaluation of Impact
- The impact of the VIP can be seen in that variation in quality has decreased and the mean quality has increased. However, this has not been rigorously evaluated, and needs further analysis for distinction from the time trend bias.
- III. Application of Value Incentive Program to the Changing Payment System
- In July 2012, the diagnosis related group (DRG) payment system was changed from voluntary participation to mandatory in seven DRG inpatient services as follow: Lens procedures, tonsillectomy and/or adenoidectomy, appendectomy, vaginal delivery, Caesarean section, inguinal and/or femoral hernia procedures, anal and/or perianal procedures. as authorized by the Health Insurance Policy Deliberation Committee in 2011. This expansion was established under the MOHW in accordance with the National Health Insurance Act and the DRG payment system. Because the VIP is a complementary payment system, the objective and incentive structure should be redesigned depending on the main payment system.
- IV. Expansion of the Value Incentive Program to Primary Care Clinics
- While increases in national medical expenses are mainly attributed to acute hospitals, higher-quality and more efficient payment systems are required without delay in primary care clinics and long-term care facilities. If the VIP is adopted in these areas, it should be redesigned to enhance the delivery system.
FURTHER CHALLENGES AND FUTURE DIRECTIONS
- Seven years after HIRA executed quality assessment (2000), the HIRA VIP was established (2007) for improving quality of care and decreasing the quality gaps. Thus far, the VIP has targeted AMI and C-section care. The results of the VIP showed continuous and marked improvement in the CQSs of the AMI and C-section measures between 2007 and 2010. Based on the VIP's success, the HIRA VIP was expanded to include general hospitals. The HIRA VIP was deemed applicable to the Korean healthcare system, but before it can be expanded further, the program must address several major concerns.
SUMMARY
-
The authors have no conflicts of interest with the material presented in this paper.
-
This article is available at http://jpmph.org/.
Notes
- 1. Health Insurance Review and Assessment Service. Comprehensive quality report of National Health Insurance 2009. 2010. Seoul: Health Insurance Review and Assessment Service; p. 3-38 p. 60-68 p. 105-117 (Korean)
- 2. Health Insurance Review and Assessment Service. Comprehensive quality report of National Health Insurance 2010. 2011. Seoul: Health Insurance Review and Assessment Service; p. 3-43 p. 66-73 p. 127-141 (Korean)
- 3. Organisation for Economic Cooperation and Development. Health at a glance 2011: OECD indicators, OECD publishing. 2011. Paris: Organisation for Economic Co-operation and Development; p. 96-97
- 4. Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction). J Am Coll Cardiol 2004;44(3):E1-E211. 15358047PubMed
- 5. Spertus JA, Radford MJ, Every NR, Ellerbeck EF, Peterson ED, Krumholz HM, et al. Challenges and opportunities in quantifying the quality of care for acute myocardial infarction: summary from the Acute Myocardial Infarction Working Group of the American Heart Association/American College of Cardiology First Scientific Forum on Quality of Care and Outcomes Research in Cardiovascular Disease and Stroke. Circulation 2003;107(12):1681-1691. 12668506ArticlePubMed
- 6. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 2003;361(9351):13-20. 12517460ArticlePubMed
- 7. Boersma E, Pieper KS, Steyerberg EW, Wilcox RG, Chang WC, Lee KL, et al. The PURSUIT Investigators. Predictors of outcome in patients with acute coronary syndromes without persistent ST-segment elevation. Results from an international trial of 9461 patients. Circulation 2000;101(22):2557-2567. 10840005ArticlePubMed
- 8. Marciniak TA, Ellerbeck EF, Radford MJ, Kresowik TF, Gold JA, Krumholz HM, et al. Improving the quality of care for Medicare patients with acute myocardial infarction: results from the Cooperative Cardiovascular Project. JAMA 1998;279(17):1351-1357. 9582042ArticlePubMed
- 9. Baigent C, Collins R, Appleby P, Parish S, Sleight P, Peto R. The ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. ISIS-2: 10 year survival among patients with suspected acute myocardial infarction in randomised comparison of intravenous streptokinase, oral aspirin, both, or neither. BMJ 1998;316(7141):1337-1343. 9563981ArticlePubMedPMC
- 10. Collaborative overview of randomised trials of antiplatelet therapy. I. Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Antiplatelet Trialists' Collaboration. BMJ 1994;308(6921):81-106. 8298418ArticlePubMedPMC
- 11. Park JS, Kang CH, Kim CY. Can cesarean section rate be used as a hospital-wide quality indicator in Korean hospitals? Korean J Obstet Gynecol 1997;40(9):1943-1953
- 12. Librero J, Peiro S, Calderon SM. Inter-hospital variations in caesarean sections. A risk adjusted comparison in the Valencia public hospitals. J Epidemiol Community Health 2000;54(8):631-636. 10890876ArticlePubMedPMC
- 13. Joint Commission on Accreditation of Healthcare Organizations. Framework for improving performance: a guide for nurse. 1994. Oakbrook Terrace: Joint Commission on Accreditation of Healthcare Organizations; p. 205
- 14. Mann LI, Gallant J. Modern indications for cesarean section. Am J Obstet Gynecol 1979;135(4):437-441. 484640ArticlePubMed
- 15. Lee SI, Khang YH, Ha BM, Lee MS, Kang W, Koo HJ, et al. Inter-hospital comparison of cesarean section rates after risk adjustment. Korean J Prev Med 2001;34(4):337-346. (Korean)
- 16. Lee KS, Lee SI, Seo K, Do YM. Impact of risk adjustment with insurance claims data on cesarean delivery rates of healthcare organizations in Korea. J Prev Med Public Health 2005;38(2):132-140. (Korean). 16315749PubMed
REFERENCES
|
1st year (treatment record of second half of 2007) |
2nd year (treatment record of 2008) |
3rd year (treatment record of 2009) |
|
|---|---|---|---|
| Set the disincentive threshold | Applied incentives | Applied incentives and disincentives | |
| Incentives1 | |||
| No. of institutions | |||
| Total | 212 | 262 | |
| AMI | - | 15 | 13 |
| C-section | - | 15 | 17 |
| Amount of money | |||
| Total | - | 45 300 | 40 400 |
| AMI | - | 31 000 | 25 000 |
| C-section | - | 14 300 | 15 400 |
| Disincentives3 | - | - | None |
Unit: institution, 10 000 Korean won.
AMI, acute myocardial infarction; C-section, Caesarian section.
1 First grade and quality-improved institutions.
2 Number of overlapped institutions: nine institutions for the second year (first grade for both items: five institutions, first grade or quality-improved: four institutions); four institutions for the third year (first grade for both items: one institution, quality-improved in both items: one institution, first grade or qualityimproved: two institutions).
3 Institutions under the disincentive threshold.
Figure & Data
References
Citations

- Relationship between patient outcomes and patterns of fragmented cancer care in older adults with gastric cancer: A nationwide cohort study in South Korea
Dong-Woo Choi, Seungju Kim, Sun Jung Kim, Dong Wook Kim, Kwang Sun Ryu, Jae Ho Kim, Yoon-Jung Chang, Kyu-Tae Han
Journal of Geriatric Oncology.2024; 15(2): 101685. CrossRef - Effects of intensive care unit quality assessment on changes in medical staff in medical institutions and in-hospital mortality
Seungju Kim, Gui Ok Kim, Syalrom Lee, Yong Uk Kwon
Human Resources for Health.2024;[Epub] CrossRef - Beta-blocker therapy in patients with acute myocardial infarction: not all patients need it
Seung-Jae Joo
Acute and Critical Care.2023; 38(3): 251. CrossRef - Patient Perspectives of Chronic Disease Management and Unmet Care Needs in South Korea: A Qualitative Study
Kyunghee Yi, Sujin Kim
Journal of Patient Experience.2023;[Epub] CrossRef - Epidemiological changes in cytomegalovirus end-organ diseases in a developed country: A nationwide, general-population-based study
Seul Gi Yoo, Kyung Do Han, Kyoung Hwa Lee, Joohee Lim, Yeonju La, Da Eun Kwon, Sang Hoon Han
Journal of Microbiology, Immunology and Infection.2022; 55(5): 812. CrossRef - Improvement in Age at Mortality and Changes in Causes of Death in the Population with Diabetes: An Analysis of Data from the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
Eugene Han, Sun Ok Song, Hye Soon Kim, Kang Ju Son, Sun Ha Jee, Bong-Soo Cha, Byung-Wan Lee
Endocrinology and Metabolism.2022; 37(3): 466. CrossRef - Feasibility of Capturing Adverse Events From Insurance Claims Data Using International Classification of Diseases, Tenth Revision, Codes Coupled to Present on Admission Indicators
Juyoung Kim, Eun Young Choi, Won Lee, Hae Mi Oh, Jeehee Pyo, Minsu Ock, So Yoon Kim, Sang-il Lee
Journal of Patient Safety.2022; 18(5): 404. CrossRef - Trends and disparities in avoidable, treatable, and preventable mortalities in South Korea, 2001-2020: comparison of capital and non-capital areas
Sang Jun Eun
Epidemiology and Health.2022; 44: e2022067. CrossRef - Performance and Challenges in Implementing the National Quality Assessment Program
Bo Yeon Kim
Health Insurance Review & Assessment Service Research.2021; 1(1): 23. CrossRef - The effect of pay for performance on income inequality between medical and non-medical staff
Mohammad Mohammadi, Mehdi Yousefi, Amin Mohammadi, Elahe Pourahmadi, Hossein Ebrahimipour, Saeed Malek Sadati
Journal of Health Administration.2021; 24(3): 43. CrossRef - Cardiovascular and Bleeding Risks Associated With Nonsteroidal Anti-Inflammatory Drugs After Myocardial Infarction
Dong Oh Kang, Hyonggin An, Geun U Park, Yunjin Yum, Eun Jin Park, Yoonjee Park, Won Young Jang, Woohyeun Kim, Jah Yeon Choi, Seung-Young Roh, Jin Oh Na, Jin Won Kim, Eung Ju Kim, Seung-Woon Rha, Chang Gyu Park, Hong Seog Seo, Cheol Ung Choi
Journal of the American College of Cardiology.2020; 76(5): 518. CrossRef - Dilemmas Within the Korean Health Insurance System
Donghwi Park, Min Cheol Chang
Journal of Preventive Medicine and Public Health.2020; 53(4): 285. CrossRef - Performance Pay in Hospitals: An Experiment on Bonus–Malus Incentives
Nadja Kairies-Schwarz, Claudia Souček
International Journal of Environmental Research and Public Health.2020; 17(22): 8320. CrossRef - Increased Age of Death and Change in Causes of Death Among Persons With Diabetes Mellitus From the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
Eugene Han, Sun Ok Song, Hye Soon Kim, Kang Ju Son, Sun Ha Jee, Bong-Soo Cha, Byung-Wan Lee
SSRN Electronic Journal .2020;[Epub] CrossRef - Design and effects of outcome-based payment models in healthcare: a systematic review
F. P. Vlaanderen, M. A. Tanke, B. R. Bloem, M. J. Faber, F. Eijkenaar, F. T. Schut, P. P. T. Jeurissen
The European Journal of Health Economics.2019; 20(2): 217. CrossRef - Accuracy of an administrative database for pancreatic cancer by international classification of disease 10th codes: A retrospective large-cohort study
Young-Jae Hwang, Seon Mee Park, Soomin Ahn, Jong-Chan Lee, Young Soo Park, Nayoung Kim
World Journal of Gastroenterology.2019; 25(37): 5619. CrossRef - Relationship between nurse staffing level and adult nursing-sensitive outcomes in tertiary hospitals of Korea: Retrospective observational study
Chul-Gyu Kim, Kyun-Seop Bae
International Journal of Nursing Studies.2018; 80: 155. CrossRef - Designing a Framework for “Iranian Pay for Performance” Program for Non-Medical Workforce in Hospitals
Serajaddin Gray, Alireza Olyaee Manesh, Iraj Harirchi, Saharnaz Nedjat
Health Scope.2018;[Epub] CrossRef - Caesarean Section Rates and Activity-Based Funding in Northern Norway: A Model-Based Study Using the World Health Organization’s Recommendation
Jan Norum, Tove Elisabeth Svee
Obstetrics and Gynecology International.2018; 2018: 1. CrossRef - Pay-for-performance reduces healthcare spending and improves quality of care: Analysis of target and non-target obstetrics and gynecology surgeries
Seung Ju Kim, Kyu-Tae Han, Sun Jung Kim, Eun-Cheol Park
International Journal for Quality in Health Care.2017; 29(2): 222. CrossRef - Impact of health insurance status changes on healthcare utilisation patterns: a longitudinal cohort study in South Korea
Jae-Hyun Kim, Sang Gyu Lee, Kwang-Soo Lee, Sung-In Jang, Kyung-Hee Cho, Eun-Cheol Park
BMJ Open.2016; 6(4): e009538. CrossRef - Pay for performance in the inpatient sector: A review of 34 P4P programs in 14 OECD countries
Ricarda Milstein, Jonas Schreyoegg
Health Policy.2016; 120(10): 1125. CrossRef - Association Between Results of Quality Assessment of Long‐Term Care Facilities and Hospital‐Acquired Pneumonia in Individuals with Stroke or Neurodegenerative Disease in Korea
Seung J. Kim, Kyu‐Tae Han, Sun J. Kim, Eun‐Cheol Park
Journal of the American Geriatrics Society.2016;[Epub] CrossRef - Association between human resources and risk of hospitalisation in end-stage renal disease outpatients receiving haemodialysis: a longitudinal cohort study using claim data during 2013–2014
Hoon-Hee Choi, Kyu-Tae Han, Chung Mo Nam, Ki Tae Moon, Woorim Kim, Eun-Cheol Park
BMJ Open.2016; 6(8): e011319. CrossRef - Changes in Saturday outpatient volume and billings after introducing the Saturday incentive programme to clinics in South Korea: a longitudinal cohort study using claims data from 2012 to 2014
Hyun Ji Ha, Kyu-Tae Han, Sun Jung Kim, Tae Yong Sohn, Byungyool Jeon, Eun-Cheol Park
BMJ Open.2016; 6(6): e011248. CrossRef - The Possibility of Expanding Pay-for-Performance Program as a Provider Payment System
Byongho Tchoe, Suehyung Lee
Health Policy and Management.2013; 23(1): 3. CrossRef
 KSPM
KSPM



 PubReader
PubReader ePub Link
ePub Link Cite
Cite