Articles
- Page Path
- HOME > J Prev Med Public Health > Volume 55(4); 2022 > Article
-
Original Article
Evaluation of the Public Health Emergency Response to the COVID-19 Pandemic in Daegu, Korea During the First Half of 2020 -
Hwajin Lee1
 , Keon-Yeop Kim1
, Keon-Yeop Kim1 , Jong-Yeon Kim2
, Jong-Yeon Kim2 , Sin Kam1
, Sin Kam1 , Kyeong Soo Lee3
, Kyeong Soo Lee3 , Jung Jeung Lee4
, Jung Jeung Lee4 , Nam Soo Hong1
, Nam Soo Hong1 , Tae-Yoon Hwang3
, Tae-Yoon Hwang3
-
Journal of Preventive Medicine and Public Health 2022;55(4):360-370.
DOI: https://doi.org/10.3961/jpmph.22.068
Published online: June 22, 2022
1Department of Preventive Medicine, Kyungpook National University School of Medicine, Daegu, Korea
2Department of Public Health, Kyungpook National University Hospital, Daegu, Korea
3Department of Preventive Medicine and Public Health, Yeungnam University College of Medicine, Daegu, Korea
4Department of Preventive Medicine, Keimyung University College of Medicine, Daegu, Korea
- Corresponding author: Keon-Yeop Kim, Department of Preventive Medicine, Kyungpook National University School of Medicine, 680 Gukchaebosang-ro, Jung-gu, Daegu 41944, Korea, E-mail: pmkky@knu.ac.kr
Copyright © 2022 The Korean Society for Preventive Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Objectives
- This study evaluated the response in Daegu, Korea to the first wave of the coronavirus disease 2019 (COVID-19) pandemic according to a public health emergency response model.
-
Methods
- After an examination of the official data reported by the city of Daegu and the Korea Centers for Disease Control and Prevention, as well as a literature review and advisory meetings, we chose a response model. Daegu’s responses were organized into 4 phases and evaluated by applying the response model.
-
Results
- In phase 1, efforts were made to block further transmission of the virus through preemptive testing of a religious group. In phase 2, efforts were concentrated on responding to mass infections in high-risk facilities. Phase 3 involved a transition from a high-intensity social distancing campaign to a citizen participation–based quarantine system. The evaluation using the response model revealed insufficient systematic preparation for a medical surge. In addition, an incorporated health-related management system and protection measures for responders were absent. Nevertheless, the city encouraged the participation of private hospitals and developed a severity classification system. Citizens also played active roles in the pandemic response by practicing social distancing.
-
Conclusions
- This study employed the response model to evaluate the early response in Daegu to the COVID-19 pandemic and revealed areas in need of improvement or maintenance. Based on the study results, creation of a systematic model is necessary to prepare for and respond to future public health emergencies like the COVID-19 pandemic.
- From December 31, 2019, to January 3, 2020, 44 cases of pneumonia with unknown cause were reported to the World Health Organization (WHO). The novel coronavirus was subsequently isolated and the WHO declared a pandemic. Following confirmation of the first case in Korea on January 20, 2020, large numbers of residents of Daegu tested positive for coronavirus disease 2019 (COVID-19). The National Crisis Alert Level was raised to the highest level on February 23, 2020.
- The first patient detected in Daegu was a member of a certain religious group, and the number of daily confirmed cases surged among church members [1,2]. Although the initial problem of hospital bed shortages was resolved by dedicating hospitals and residential treatment centers to COVID-19 cases, mass infections persisted in convalescent hospitals and psychiatric hospitals. After the number of daily cases peaked at 741, it decreased and then remained in single digits after April 8. Social distancing, which had begun on February 29, 2020, was eased temporarily.
- After the 2009 H1N1 pandemic and the 2015 Middle East respiratory syndrome (MERS) outbreak, the Korea Centers for Disease Control and Prevention (KCDC; currently the Korea Disease Control and Prevention Agency) attempted to build a response strategy for public health emergencies [3,4]. However, there were no unified guidelines for emergency response until the first wave of the COVID-19 pandemic in Korea began. During the early stages of the pandemic, the authorities established a strategy based on the MERS response guidelines [5]. While repeating revisions, operations of residential treatment centers and drive-through testing were promoted for the first time [6–8].
- It is the state’s obligation to prepare for all kinds of community health crises [9]. In the United States, the European Union (EU), and the WHO, models for emergency response had been built prior to COVID-19 [10–13]. On the basis of the most appropriate for the evaluation of Daegu’s response among those models, we intended to conduct a thorough exploration between every response process so that a foundation will be provided for developing a Korean emergency response model.
INTRODUCTION
- The COVID-19 Situation During the Study Period
- The target period of the study was between January 20, 2020, when the nation’s first COVID-19 case was identified, and the end of April 2020, when the first wave of the pandemic stabilized. The city of Daegu and the KCDC announced daily counts of COVID-19 cases, deaths, and the number of people released from self-quarantine [14,15]. We examined both official databases to understand the pattern of the pandemic, and graphically represented the daily and cumulative incidence.
- Classification of Responses by Phase
- To consider the timeliness of Daegu’s public health emergency response, we classified the target period into 4 phases: the preparatory phase and phases 1–3. Agreement was reached to use the trends in daily and cumulative incidence and major changes in the city’s response strategies (e.g., the introduction of residential treatment centers and the conversion of the quarantine from city-led to citizen participation–based) as criteria for classification by phases. The adequacy of the classification criteria was subsequently reviewed with external specialists.
- Our target period was equivalent to stages 1 and 2 of the KCDC report [16], which organized the domestic situation into 5 stages. Stage 1 in the report was from January 20 to February 17, 2020, when sporadic cases were coming in from abroad. Stage 2 was from February 18 to May 5, 2020, when the outbreak in a religious group was predominant in Daegu, coinciding with the target period of our study.
- Evaluation of Responses According to the Response Model
- We referred to the emergency response models produced by the WHO, the EU, and the United States [10–13]. Of these, the Public Health Emergency Preparedness and Response Capabilities [10], established by the Centers for Disease Control and Prevention (CDC) in the United States, had more subdivided definitions for capabilities that we could use to inspect the city’s response in detail. The CDC model, announced in 2011 and updated in 2018, consists of 6 domains and 15 capabilities (Table 1). Each capability consists of (1) its definition, (2) the functions critical for accomplishing that capability’s definition, (3) the tasks necessary to achieve 1 or more functions, and (4) the resources necessary to perform the tasks [10]. Since Daegu’s response was not based on the CDC response model, it was decided not to evaluate their response based on the completion of a function or a task. Taking this practical aspect into account, we adopted the capability definitions as criteria for assessing how Daegu reacted to the first wave of the COVID-19 pandemic in Korea. In other words, we investigated whether the city’s responses fulfilled each of the capability definitions, as presented in Supplemental Material 1.
- The city’s responses to COVID-19 were summarized by collecting the officially announced data and internal data of the city of Daegu, such as daily records of the COVID-19 response and meeting notes. The responses were sorted according to the capability definitions of the CDC model. Next, preventive medicine specialists who engaged directly in Daegu’s COVID-19 response evaluated whether the city’s response achieved the capability definitions, followed by a secondary evaluation by the entire research team. A final review was done during 5 advisory meetings.
- Ethics Statement
- This study was based on data open to the public. Ethical approval by an institutional review board and written informed consent were not required.
METHODS
- COVID-19 Case and Death Counts in Daegu
- Figure 1 shows the status of both the daily COVID-19 cases and the daily number of people released from self-quarantine between February 18 and April 30, 2020. On February 27, 10 days after the first COVID-19 case was identified in Daegu, the cumulative number of confirmed cases exceeded 1000. On February 29, the number of daily confirmed cases peaked at 741. After the number of cumulative cases reached over 5000 on March 7, the number of daily cases was approximately 100, decreasing to less than 100 on March 11 and remaining in single digits after April 8. The number of people released from self-quarantine steadily increased and became greater than the number of daily confirmed cases on March 11.
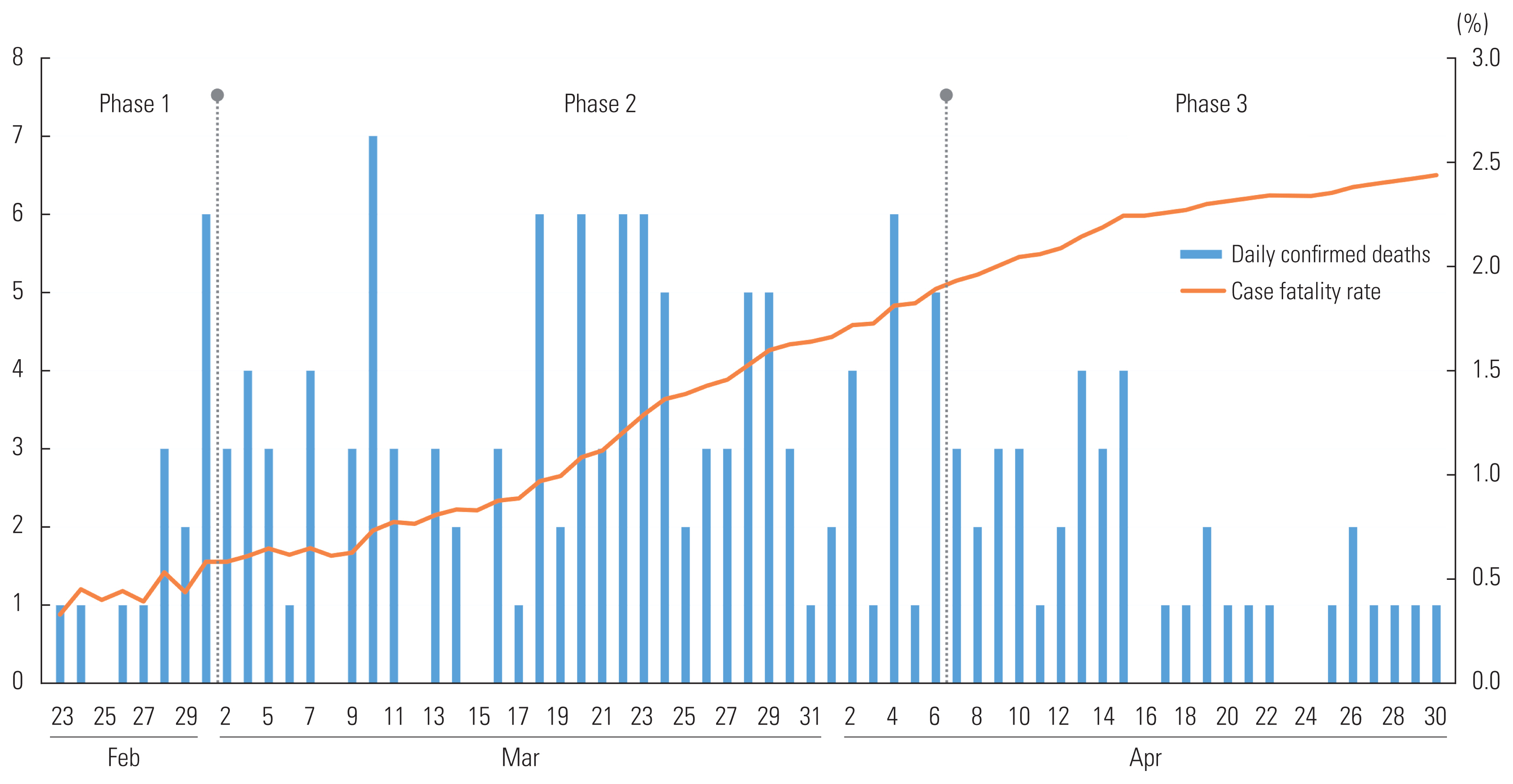
- Figure 2 shows the daily death counts and the case fatality rates. On March 7, approximately 2 weeks after the first COVID- 19 death was identified, the number of confirmed deaths reached 33. The highest number of daily deaths was 7 on March 10, and the number of cumulative deaths until March 31 was 111. With 1 death to 5 deaths occurring every day in April, the cumulative deaths by April 30 was 169. The case fatality rate was 2.43%.
- Phases Based on COVID-19 Status and the Major Responses in Daegu
- Daegu’s response was divided into the preparation phase and phases 1–3, according to COVID-19 status and the timing of the introduction of quarantine policies. Table 2 shows the major events during the early pandemic in Daegu and the responses by authorities, as well as the national crisis alert level corresponding to each phase.
- During the preparation phase from January 20, 2020 (when the nation’s first case was confirmed) until February 16, 2020, Daegu prepared for the occurrence of cases within the community. As the crisis alert level was raised to Level 2 (caution) on January 20, 2020 and again to Level 3 (alert) on January 27, 2020 the city expanded the countermeasure team.
- Phase 1, from February 17 (when the city’s first case was detected) until March 1, was the period when the number of confirmed patients surged in a certain religious group. The city responded by forming a public-private joint task force, and the government aided by forming a pan-government support team. More hospitals were designated for COVID-19 treatment, and doctors monitored patients waiting to be hospitalized by telephone. As a full-scale investigation of the religious group was conducted, the increasing demand for tests was handled by arranging drive-through testing and increasing the number of screening centers. On February 23, the crisis alert level was raised to Level 4 (severe), the highest level, as preemptive action against nationwide spread of the virus.
- Phase 2 ran from March 2 (when residential treatment centers began to operate) until April 6. The implementation of designated COVID-19 hospitals and residential treatment centers allowed for a more stable treatment environment. However, the response concentrated on fighting the mass infections in convalescent hospitals and psychiatric hospitals. Although there were attempts to transfer groups of confirmed patients out of these facilities, it was difficult to secure beds because of limited nursing services or the difficulties in managing patients with mental disorders. This resulted in additional cases. By allocating one public official to each hospital and organizing a joint task force with the designated COVID-19 hospitals, it was possible to share information on inpatient status and facilitate patient transfers.
- Phase 3 was between April 7 and the end of April. Despite stabilization of the early pandemic, long-term responses to COVID-19 appeared necessary. To relieve the physical and emotional exhaustion caused by prolonged high-intensity social distancing, the city formed a pan-citizen committee composed of 200 civic representatives. By holding regular videoconferences between the city and the committee to review government proposals, the 7 basic living rules for Daegu residents and quarantine rules for 9 areas including the economy, medical care, and education were established. While the crisis alert level remained at Level 4, the government announced that it would extend its social distancing rules for 16 days beginning April 20, but would relax some of the rules.
- Evaluation of Daegu’s COVID-19 Response According to the Emergency Response Model
- The evaluation of the response to the early pandemic in Daegu is outlined in Table 3 according to the CDC model capabilities.
- First, the fundamental problem of the community preparedness capability (categorized under the community resilience domain), was that organized preparation for a public health emergency had not been developed in advance. In Korea, the Framework Act on the Management of Disasters and Safety, which stipulates preparation and restoration measures for social and natural disasters, was enacted in 2004, but was partially amended every 1–2 years [17]. Whenever a crisis occurred, the act was supplemented to correct shortcomings [18], leading the public to feel that the performance of both central and local governments was not effective [19]. The CDC, after defining infectious disease outbreaks, biochemical accidents, and natural disasters as public health emergencies and developing a response model, encouraged local governments to use the model in preparation for and response to emergencies [10,20]. The Korean government also needs to establish an integrated and systematic guideline for local governments and communities to prepare for and respond to any kind of emergency. In addition, the community recovery capability within the same domain should be taken into account while responding to a crisis, not after the crisis ends. Considering the economic and psychological impact of repeated emerging infectious diseases such as the H1N1 pandemic, the MERS outbreak, and the COVID-19 pandemic on the community, true recovery of the community can be achieved only by accepting a life that exists with these crises, not expecting or waiting for them to end. This is in line with the CDC’s definition of community resilience, which is the process of adapting to a crisis beyond resistance to it [10]. Furthermore, unlike recovery, which focuses on restoring normal conditions [21], resilience means strengthening the ability of a community to do what it can do during a crisis [10]. Thus, when recovery is implemented in terms of resilience, communities can continue their activities without having to wait for a crisis to end. This is especially important in a continually changing crisis like the COVID-19 pandemic [21].
- Second, regarding the emergency operations coordination capability (under the incident management domain), in the early stage of an emerging infectious disease like COVID-19 when its characteristics are not fully known [22], governance must be flexible so that decision-making and rapid cooperation are feasible. Moreover, a single management system linked to health care and all other public and private sectors must be developed for emergency response. In Korea, where private medical services predominate, a close relationship with private medical institutions is critical, and prior cooperative governance between the Ministry of Health and Welfare, the Ministry of the Interior and Safety, the national government, and local governments must be established [17]. In Daegu’s response, it was desirable that public officials and preventive medicine specialists, both of whom could make major decisions, shared an office from the beginning to overcome any physical barriers to communication and to enable rapid cooperation.
- Third, regarding the emergency public information and warning capability (under the information management domain), the city held regular briefings for the media and informed citizens of the pandemic status through various channels. Risk communication is the process of informing the public of an unexpected crisis, and the person in charge should carefully deliberate how to alert the public to the crisis. Appropriate content, format, and timing of risk communication can improve the situation, whereas inappropriate risk communication may worsen the situation [23]. The CDC suggests 6 principles of risk communication: be first, be right, be credible, express empathy, promote action, and show respect [23]. In an infectious disease crisis like the COVID-19 pandemic, each citizen is not simply an object of crisis management, but rather an agent for overcoming the crisis who can promote an early end to the crisis by complying with quarantine rules and trusting in the authorities. Therefore, it is vitally important to provide accurate information to citizens in a timely manner. Regarding the information sharing capability of the same domain, information was not shared in real time between the health and medical resource management systems operated individually by ministries [24], creating an obstacle to rapidly responding to the surge in COVID-19 patients. Furthermore, even though an integrated management system for diseases and health care was developed by the KCDC, its operation was unsystematic and it was inconvenient to use [24]. Recognizing these problems, it is urgently necessary to incorporate management systems that are spread across ministries or to introduce another, more efficient system that would enable local governments to share information and identify the status of health and medical resources as they respond to the public health emergency.
- Fourth, regarding the medical countermeasure dispensing and administration capability (under the countermeasures and mitigation domain), the Central Clinical Committee proposed an initial patient classification system. Because this involved checking the vital signs of those waiting for hospitalization at home, it could not be applied on-site. Therefore, with the help of the Daegu Medical Association, a more practical patient severity classification system was introduced using the available epidemiological data and the National Health Insurance Service data on underlying diseases, allowing doctors to monitor patients by telephone [7,25]. Regarding the medical material management and distribution capability of the same domain, medical supplies must be managed and dispensed according to the guidelines once they are supplied. Next, regarding the non-pharmaceutical interventions capability, citizens voluntarily engaged in social distancing and, as a result, helped to control the early COVID-19 pandemic and prevent a nationwide spread. Regarding the responder safety and health capability, protection systems were not adequate for either public officials or medical staff. The safety of responders must be assured by identifying risks and providing both physical and psychological protection [26–29].
- Fifth, regarding the fatality management capability (under the surge management domain), the government quickly distributed guidance for the funerals of those who died with COVID-19 [30]. In Phase 1 of Daegu’s response, deaths occurred in severely ill patients or patients whose symptoms worsened while waiting for hospitalization. Delays were due to limited availability of the negative-pressure rooms being used for confirmed cases. In Phase 2, many deaths occurred due to the mass infections in convalescent hospitals for elderly patients. Daegu quickly formed a response team based on the government’s funeral guidelines that had been distributed 6 days after the city’s first case was confirmed. Regarding the mass care capability of the same domain, mass infections in convalescent hospitals and psychiatric hospitals resulted in many COVID-19 cases. Public officials were assigned to those hospitals that lacked infectious disease specialists and were in charge of overall management, including the isolation of close contacts and patient transfers. Next, regarding the medical surge capability, the rapid increase in the demand for inpatient treatment was resolved with the prompt help of private hospitals. Confronting a public health emergency like an emerging infectious disease, a response organization should be able to determine the level of crisis; predict medical needs; establish plans to secure additional personnel, facilities, and equipment; and request necessary support from the private sector [10]. Regarding the volunteer management capability, there was dissatisfaction among responders over the volunteers’ wage differences. This issue impeded the emergency response process and needs to be improved.
- Last, regarding the public health laboratory testing capability (under the biosurveillance domain), to meet the increasing demand for tests in Phase 1, Kyungpook National University Chilgok Hospital implemented drive-through testing based on a large-scale screening center model suggested by Kim Jin Yong at the Incheon Medical Center [8]. Safe and fast tests were performed, reducing contact with others and saving time because there was no need to leave the vehicle for sample collection [8]. This strengthened testing capabilities, which enabled comprehensive surveillance of the high-risk facilities, including the religious group and convalescent hospitals, and served as a key component in Daegu’s response. Regarding the public health surveillance and epidemiological investigation capability of the same domain, the 2-stage investigation, basic and in-depth, was challenging due to the rapid increase in confirmed cases in the early pandemic. The investigation method was adjusted by introducing phone surveys with simplified forms. Nonetheless, it was difficult to conduct an accurate investigation, including determination of close contacts and estimation of the onset of symptoms, because the personnel performing the surveys had insufficient pre-training.
RESULTS
- The present study examined the COVID-19 response in the city of Daegu, Korea from February to April 2020. Besides the dedication of medical staff and volunteers, combating the early COVID-19 pandemic in Korea was possible because citizens willingly practiced social distancing, the leadership of the city preemptively induced public-private cooperation, and the central and local governments provided assistance. The city of Daegu, together with the central government, established the world’s first residential treatment centers and drive-through testing centers, led the revision of guidelines required for an emergency response, and gained experience in managing sources of infection within the community. Nevertheless, preparation for the initial surge in cases, proactive control of the pandemic in high-risk facilities, and the integration of health-related management systems were insufficient.
- To handle public health emergencies, including an emerging infectious disease outbreak, systematic and well-founded guidelines are needed. In Korea, a COVID-19 response guideline was written and modified, based on the MERS response guidelines and the white papers written in response to the H1N1 pandemic and the MERS outbreak [31–33]. Nevertheless, it was an inadequate response to the initial surge of confirmed cases and the subsequent pandemic. Referring to international data on response systems, Lee [34] pointed out that there are only manuals for departmental duties in Korea, and recommended implementing a response framework based on the results of monitoring, analysis, risk assessment, and planning in 13 areas. Shon et al. [35] employed the CDC model to analyze the achievements and failures of Seoul’s COVID-19 response. The WHO Regional Office for Europe proposed 20 strategies for each country to adopt in recovery from the COVID-19 crisis [36].
- This study had some limitations in its methods. First, although we evaluated the COVID-19 response in Daegu using the CDC model, the response in Daegu was not based on the components of the CDC model. Therefore, the validity of the evaluation criteria may be questionable. However, even in the absence of a Korean public health emergency response model to serve as a criterion, it was meaningful to attempt an evaluation. Also, despite our efforts to describe in detail the components of the CDC model and our evaluation method, we applied a model composed of qualitative evaluations and objectivity may have been affected. In fact, it is difficult to evaluate a crisis quantitatively, and most response models, including the CDC model, contain qualitative evaluations. Building on the results of this evaluation, consideration must be given to enabling an objective evaluation while creating an advanced Korean response model for the next public health emergency.
- Grounded in Daegu’s experience and our evaluation, we would like to suggest that the central government refer to the following recommendations when developing a Korean response model. First, response to a medical surge must be built on public-private cooperation, rather than the abilities of individual medical institutions. Second, in addition to testing, tracing, and treatment, it is necessary to have an information system, a surveillance system, and prepared scenarios fitting each level of a crisis. Third, to reinforce regional governance, administration and information sharing at all governance levels (i.e., local, regional, and national) are needed. Next, the central government must construct a response system for recurring and emerging infectious diseases. At the same time, a paradigm in which we accept risks that can be taken is required. Finally, both central and local governments must be ready for future public health emergencies after COVID-19.
- This study examined Korea’s early COVID-19 pandemic and the response process in the city of Daegu. From February to April 2020, the city and the central government had to adapt to the absence of specific response guidelines for this health emergency. Based on the results of our study, a solid emergency response model must be established by the time another public health emergency occurs.
DISCUSSION
SUPPLEMENTAL MATERIALS
-
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
-
FUNDING
This study was conducted with the support of the Ministry of Health and Welfare.
Notes
ACKNOWLEDGEMENTS
-
AUTHOR CONTRIBUTIONS
Conceptualization: Kim KY, Lee H, Lee KS, Kim JY. Data curation: Lee H, Lee KS, Kim JY, Kim KY. Formal analysis: Kim KY, Lee H, Kim JY. Funding acquisition: Kim KY, Lee KS. Methodology: Lee H, Kim KY, Kim JY, Kam S, Lee KS, Lee JJ, Hong NS, Hwang TY. Project administration: Kim KY. Visualization: Lee H, Lee KS, Kim JY. Writing - original draft: Lee H, Kim KY. Writing - review and editing: Lee H, Kim KY, Kim JY, Kam S, Lee KS, Lee JJ, Hong NS, Hwang TY.
Notes

Data from Centers for Disease Control and Prevention. Public health emergency preparedness and response capabilities [Internet] [10].
- 1. Jeong E, Hagose M, Jung H, Ki M, Flahault A. Understanding South Korea’s response to the COVID-19 outbreak: a real-time analysis. Int J Environ Res Public Health 2020;17(24):9571ArticlePubMedPMC
- 2. Kim JY, Lee YM, Lee H, Kim JW, Kim SW. Epidemiological characteristics of a COVID-19 outbreak caused by religious activities in Daegu, Korea. Epidemiol Health 2021;43: e2021024ArticlePubMedPMC
- 3. Seoul National University Hospital. Strategy development of public health emergency response system for natural and manmade disaster; 2013 [cited 2021 Nov 10]. Available from: https://library.nih.go.kr/ncmiklib/archive/rom/reportView.do?upd_yn=Y&rep_id=RP00001878 (Korean)
- 4. Korea Disease Control and Prevention Agency. 2014 Operational planning of public health emergency response project group; [cited 2021 Nov 10]. Available from: https://www.mohw.go.kr/react/al/sal0101vw.jsp?PAR_MENU_ID=04&MENU_ID=040101&CONT_SEQ=300115 (Korean)
- 5. Central Disease Control Headquarters. Response guidelines for novel coronavirus infection disease; [cited 2021 Nov 11]. Available from: https://library.nih.go.kr/ncmiklib/mlib/mlibViewVolume.do?bibctrlno=8272334 (Korean)
- 6. Yang Y, Kim H, Hwang J. Quarantine facility for patients with COVID-19 with mild symptoms in Korea: experience from eighteen residential treatment centers. J Korean Med Sci 2020;35(49):e429ArticlePubMedPMCPDF
- 7. Kim SW, Lee KS, Kim K, Lee JJ, Kim JY; Daegu Medical Association. A brief telephone severity scoring system and therapeutic living centers solved acute hospital-bed shortage during the COVID-19 outbreak in Daegu, Korea. J Korean Med Sci 2020;35(15):e152ArticlePubMedPMCPDF
- 8. Kwon KT, Ko JH, Shin H, Sung M, Kim JY. Drive-through screening center for COVID-19: a safe and efficient screening system against massive community outbreak. J Korean Med Sci 2020;35(11):e123ArticlePubMedPMCPDF
- 9. Bae SS. New public health: challenges to healthy society. Seoul: Gyechuk Munhwasa; 2017. p. 387-411 (Korean)
- 10. Centers for Disease Control and Prevention. Public health emergency preparedness and response capabilities; [cited 2021 Apr 7]. Available from: https://www.cdc.gov/cpr/readiness/00_docs/CDC_PreparednesResponseCapabilities_October2018_Final_508.pdf
- 11. European Centre for Disease Prevention and Control. Public health emergency preparedness – core competencies for EU member states; 2017 [cited 2021 Apr 7]. Available from: https://www.ecdc.europa.eu/sites/default/files/documents/public-health-emergency-preparedness-core-competencies-eu-member-states.pdf
- 12. European Observatory on Health Systems and Policies. COVID-19 health system response monitor (HSRM); [cited 2021 Apr 7]. Available from: https://eurohealthobservatory.who.int/monitors/hsrm
- 13. World Health Organization. Critical preparedness, readiness, and response actions for COVID-19; 2021 [cited 2021 Apr 7]. Available from: https://www.who.int/publications/i/item/critical-preparedness-readiness-and-response-actions-for-covid-19
- 14. Daegu Metropolitan City. City briefing archive 2020.2.20-2020.4.30; [cited 2021 Nov 11]. Available from: https://www.daegu.go.kr/icms/bbs/selectBoardList.do?bbsId=BBS_02098 (Korean)
- 15. Korea Disease Control and Prevention Agency. Press releases 2020.2.18-2020.4.30; [cited 2021 Nov 11]. Available from: https://www.kdca.go.kr/board/board.es?mid=a20501010000&bid=0015 (Korean)
- 16. Kim Y, Kim YY, Yeom H, Jang J, Hwang I, Park K, et al. COVID-19 1-year outbreak report as of January 19, 2021 in the Republic of Korea. Public Health Wkly Rep 2021;14(9):472-481. (Korean)
- 17. Korean Law Information Center. The Framework Act on the Management of Disasters and Safety; [cited 2022 Apr 28]. Available from: https://www.law.go.kr/LSW//lsSc.do?section=&menuId=1&subMenuId=15&tabMenuId=81&eventGubun=060101&query=%EC%9E%AC%EB%82%9C+%EB%B0%8F+%EC%95%88%EC%A0%84%EA%B4%80%EB%A6%AC+%EA%B8%B0%EB%B3%B8%EB%B2%95#undefined (Korean)
- 18. Kim BS, Ko MS. A study on the enhancement of the framework act on the management of disasters and safety. Korean J Public Saf Crim Justice 2020;29(4):3-32. (Korean)Article
- 19. Lee DK, Kim JH, Kim Y, Lim N. The 7-year anniversary of Sewol Ferry: survey analysis of disaster and safety awareness; [cited 2022 Apr 28]. Available from: https://blog.naver.com/schema209/222310716726 (Korean)
- 20. Centers for Disease Control and Prevention. About the center for preparedness and response; [cited 2022 Apr 28]. Available from: https://www.cdc.gov/cpr/aboutus/index.htm
- 21. Barton MA, Christianson M, Myers CG, Sutcliffe K. Resilience in action: leading for resilience in response to COVID-19. BMJ Leader 2020;4(3):117-119Article
- 22. Ryu S, Chun BC; Korean Society of Epidemiology 2019-nCoV Task Force Team. An interim review of the epidemiological characteristics of 2019 novel coronavirus. Epidemiol Health 2020;42: e2020006ArticlePubMedPMC
- 23. Centers for Disease Control and Prevention. Crisis and emergency risk communication (CERC): introduction; [cited 2021 Dec 20]. Available from: https://emergency.cdc.gov/cerc/ppt/CERC_Introduction.pdf
- 24. Heo Y, Sung HK, Lee S, Hwang SW. Commissioned research to prepare an integrated management plan for health and medical resources: focusing on infectious disease crisis response. Wonju: Health Insurance Review and Assessment Service; 2021. p. 1-201 (Korean)
- 25. Kim JH, An JA, Min PK, Bitton A, Gawande AA. How South Korea responded to the COVID-19 outbreak in Daegu. NEJM Catal Innov Care Deliv 2020. doi:https://doi.org/10.1056/CAT.20.0159 Article
- 26. Delgado D, Wyss Quintana F, Perez G, Sosa Liprandi A, Ponte-Negretti C, Mendoza I, et al. Personal safety during the COVID-19 pandemic: realities and perspectives of healthcare workers in Latin America. Int J Environ Res Public Health 2020;17(8):2798ArticlePubMedPMC
- 27. Nguyen J, Liu A, McKenney M, Liu H, Ang D, Elkbuli A. Impacts and challenges of the COVID-19 pandemic on emergency medicine physicians in the United States. Am J Emerg Med 2021;48: 38-47ArticlePubMedPMC
- 28. Ju G, Lee J, Ahn MH, Lee J, Kim EJ, Suh S, et al. Effects of depression and resilience of public workers on work-related stress and anxiety in response to the COVID-19 pandemic. J Korean Med Sci 2021;36(36):e262ArticlePubMedPMCPDF
- 29. Ehrlich H, McKenney M, Elkbuli A. Defending the front lines during the COVID-19 pandemic: protecting our first responders and emergency medical service personnel. Am J Emerg Med 2021;40: 213-214ArticlePubMedPMC
- 30. Ministry of Health and Welfare. Guidance for funerals of the deaths with COVID-19; 2020 [cited 2022 Mar 14]. Available from: https://www.mohw.go.kr/react/jb/sjb0406vw.jsp?PAR_MENU_ID=03&MENU_ID=030406&CONT_SEQ=353446 (Korean)
- 31. Korea Disease Control and Prevention Agency. MERS response guidelines; [cited 2021 Nov 15]. Available from: https://www.kdca.go.kr/upload_comm/syview/doc.html?fn=157311784588300.pdf&rs=/upload_comm/docu/0019 (Korean)
- 32. Korea Disease Control and Prevention Agency. The 2015 MERS outbreak in the Republic of Korea: learning from MERS; [cited 2021 Dec 20]. Available from: https://www.kdca.go.kr/board/board.es?mid=a20504000000&bid=0014&act=view&list_no=128379 (Korean)
- 33. Central Disease Control Headquarters. COVID-19 response guidelines; [cited 2021 Nov 11]. Available from: http://ncov.mohw.go.kr/upload/viewer/skin/doc.html?fn=16508495 (Korean)
- 34. Gyeonggi Infectious Disease Control Center. Coronavirus disease 2019 (COVID-19) Gyeonggi daily report – 188 data as reported by 25 September 2020; [cited 2021 August 4]. Available from: https://www.gidcc.or.kr/SUB/410 (Korean)
- 35. Shon CW, Kim CB, So YK, Kim MS, Chun BH, Tak SW, et al. Evaluation and improvement plan of the COVID-19 management system in Seoul; [cited 2021 Aug 4]. Available from: https://www.si.re.kr/node/65029 (Korean)
- 36. European Observatory on Health Systems and Policies. Health systems resilience during COVID-19: lessons for building back better; 2021 [cited 2021 Dec 20]. Available from: https://eurohealthobservatory.who.int/publications/i/health-systems-resilience-during-covid-19-lessons-for-building-back-better
REFERENCES
Figure & Data
References
Citations

- Factors influencing psychological concerns about COVID-19 in South Korea: direct and indirect damage during the early stages of pandemic
Min-sung Kim, Sung-il Cho
BMC Public Health.2024;[Epub] CrossRef - Estimation of the Effectiveness of a Tighter, Reinforced Quarantine for the Coronavirus Disease 2019 (COVID-19) Outbreak: Analysis of the Third Wave in South Korea
Marn Joon Park, Ji Ho Choi, Jae Hoon Cho
Journal of Personalized Medicine.2023; 13(3): 402. CrossRef
 KSPM
KSPM

 PubReader
PubReader ePub Link
ePub Link Cite
Cite



